Bioequivalence: What It Means for Generic Drugs and Your Health
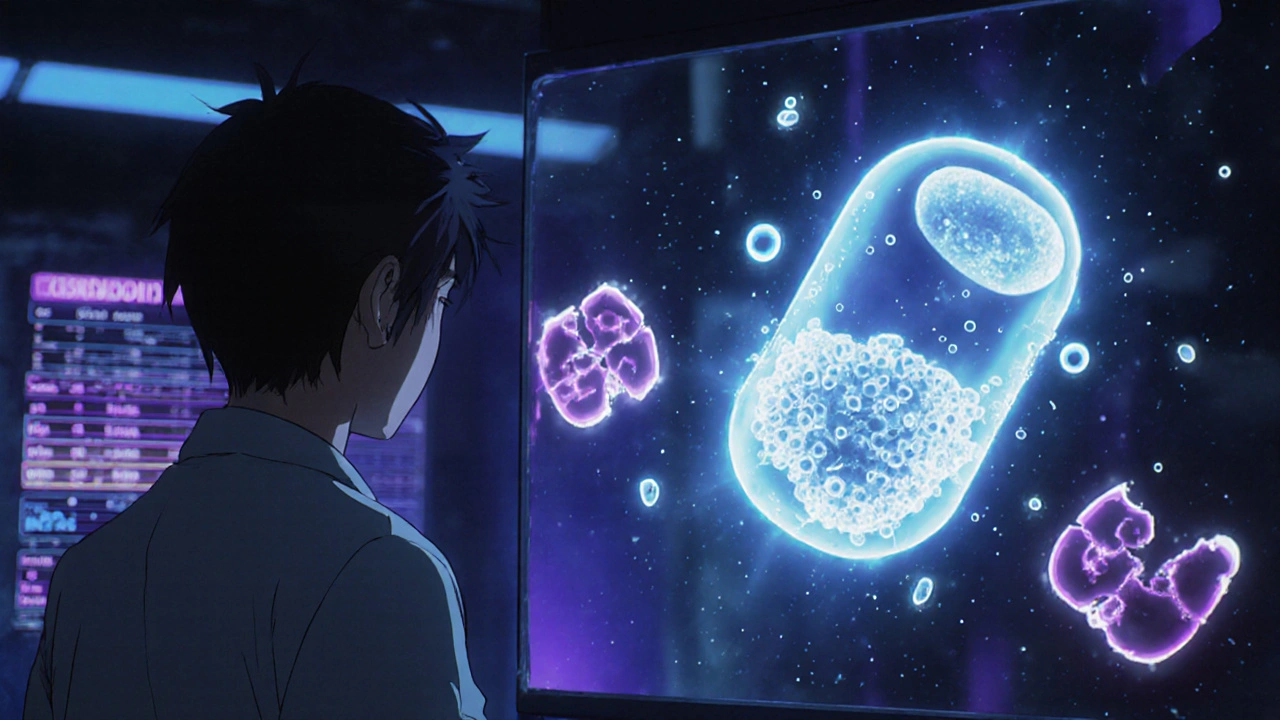
When you pick up a generic pill, you expect it to do the same job as the brand-name version. That’s where bioequivalence, the scientific standard that proves two drug formulations produce the same effect in the body. Also known as therapeutic equivalence, it’s the reason your pharmacist can swap medications without asking your doctor. Without bioequivalence, generics could be too weak, too strong, or just plain useless—and sometimes, that’s exactly what happens when the rules aren’t followed.
At its core, bioequivalence compares how fast and how much of a drug enters your bloodstream. If two versions of a drug—say, generic lisinopril and brand-name Zestril—don’t deliver the same amount of active ingredient at the same rate, your blood pressure might swing unpredictably. This isn’t theoretical. Studies have shown that even small differences in absorption can lead to treatment failure or side effects, especially with drugs that have a narrow safety window, like warfarin or levothyroxine. That’s why regulators require strict testing: same dose, same route, same timing, and nearly identical blood levels. It’s not about price—it’s about your body getting exactly what it needs.
But bioequivalence isn’t just about the active ingredient. It’s also about how the pill is made. Fillers, coatings, and how the drug breaks down in your stomach all matter. A generic version might have the same chemical formula, but if it dissolves too slowly, your body won’t absorb enough. If it dissolves too fast, you might get a spike in side effects. That’s why some patients notice differences even when a drug is labeled bioequivalent—because the testing standards, while strict, don’t always capture real-world variability across populations or long-term use. And that’s where things get messy. Some drugs, like extended-release formulations or those absorbed in the gut, are harder to match. That’s why you’ll see more reports of issues with generics for epilepsy, thyroid meds, or blood thinners than with simple pain relievers.
What you’ll find in the posts below isn’t just a list of articles—it’s a practical guide to how bioequivalence affects real people. You’ll learn why some patients switch back to brand-name drugs, how counterfeit meds fake bioequivalence with deadly results, and why even something as simple as storage can break the balance. You’ll see how CYP450 enzymes, drug interactions, and even citrus fruits can interfere with how your body handles a drug, no matter how well it was labeled. And you’ll understand why pharmacists are your best line of defense when it comes to making sure what’s in your pill bottle actually works the way it should.
Complex Generic Drugs: Why Some Products Are Harder to Approve
Complex generic drugs face steep scientific and regulatory hurdles that make FDA approval far harder than for simple generics. Learn why only a handful have been approved despite high demand and billion-dollar market potential.