Understanding GERD and Its Effects on Daily Life
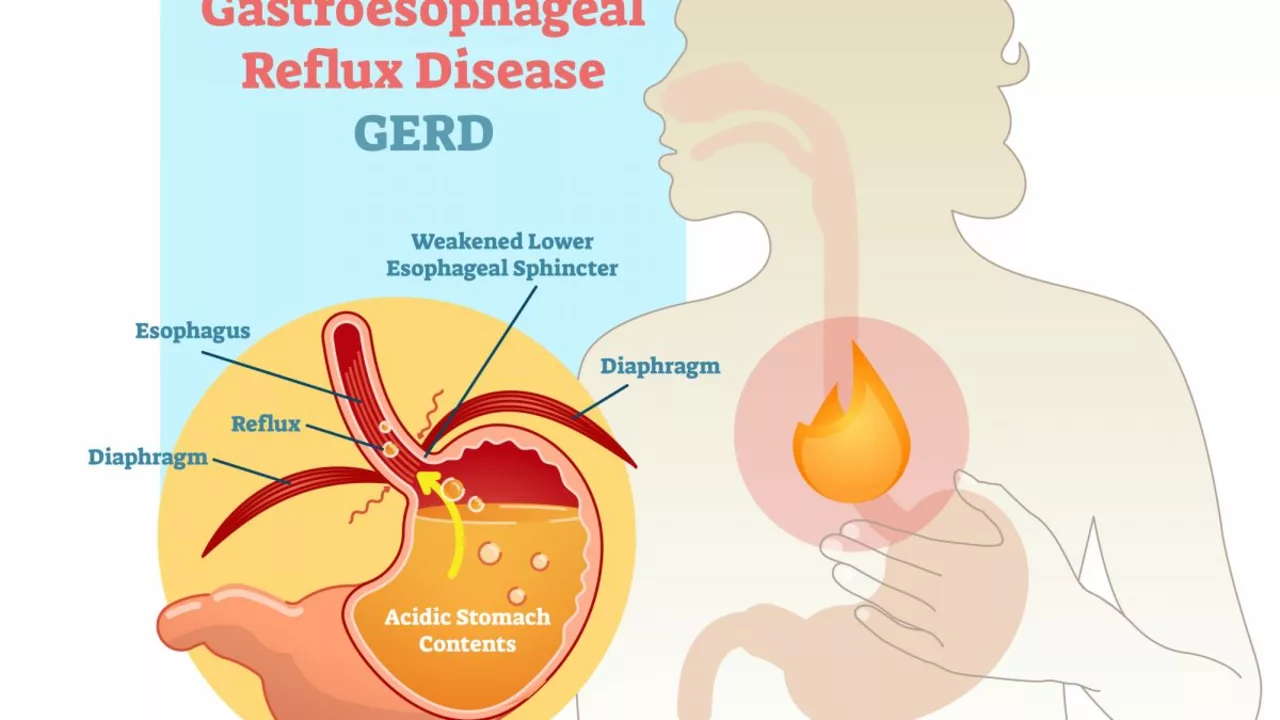
Gastroesophageal Reflux Disease, or GERD, is a chronic digestive disorder that affects millions of people worldwide. It occurs when stomach acid or bile flows back into the esophagus, causing irritation and inflammation. Symptoms of GERD can range from mild heartburn to severe chest pain and difficulty swallowing, which can severely impact an individual's quality of life. In this article, we will explore the various ways GERD affects daily living and how to manage its symptoms effectively.
The Physical Symptoms of GERD and How They Interfere with Daily Activities
GERD can manifest in various physical symptoms, which can significantly interfere with daily activities. For instance, heartburn – a burning sensation in the chest – can be so severe that it disrupts sleep and makes it difficult to concentrate on work or other tasks. Difficulty swallowing or the feeling of a lump in the throat can make eating a challenge, leading to unintentional weight loss and malnutrition. Additionally, GERD sufferers may experience frequent regurgitation, making it difficult to enjoy meals and social situations involving food.
Emotional and Psychological Effects of GERD
Living with GERD can also take a toll on an individual's emotional and psychological well-being. The constant discomfort and pain can lead to feelings of frustration, anxiety, and depression. Many people with GERD may feel embarrassed or self-conscious about their symptoms, particularly when it comes to eating in public or discussing their condition with others. This can lead to social isolation and a decreased quality of life. It's essential to recognize and address these emotional and psychological effects to help improve overall well-being and effectively manage GERD symptoms.
Impact of GERD on Sleep Quality
One of the most significant ways GERD impacts daily life is through its effect on sleep quality. The discomfort and pain associated with GERD can make it difficult to fall asleep or stay asleep, leading to insomnia and chronic sleep deprivation. Sleep is vital for overall health and well-being, and a lack of quality sleep can contribute to a wide range of health issues, including weakened immune function, weight gain, and increased risk for chronic diseases. By addressing GERD symptoms and improving sleep quality, individuals can greatly improve their overall quality of life.
GERD's Effect on Work and Productivity
The symptoms of GERD can also have a significant impact on work and productivity. People with GERD may find it challenging to focus and concentrate due to pain, discomfort, and fatigue resulting from poor sleep quality. This can lead to decreased job performance, missed deadlines, and increased sick days. In some cases, GERD symptoms may be so severe that individuals may need to take time off work or even consider a change in career. Therefore, it's crucial to find effective ways to manage GERD symptoms and minimize their impact on daily life.
Relationships and Social Life Affected by GERD
Lastly, GERD can also have a negative impact on relationships and social life. As previously mentioned, the discomfort and embarrassment associated with GERD symptoms can lead to social isolation and a reluctance to participate in activities that involve food. This can strain relationships with friends and family members and create feelings of loneliness and isolation. By finding ways to manage GERD symptoms effectively, individuals can regain control of their social lives and improve their overall quality of life.
Managing GERD Symptoms for Improved Quality of Life
While GERD can have a significant impact on daily living, there are several ways to manage its symptoms effectively. Lifestyle changes, such as losing weight, avoiding trigger foods, and elevating the head of the bed, can help reduce the severity and frequency of GERD symptoms. Additionally, over-the-counter and prescription medications can provide relief and help control acid production. In some cases, surgery may be recommended for those who do not respond to other treatments. By working with a healthcare professional to create a personalized treatment plan, individuals with GERD can improve their quality of life and regain control of their daily activities.




Listen up, folks! If you're not taking GERD seriously, you're basically saying it's okay to let chronic pain ruin your life. The fact that many people just ignore the diet warnings is absolutely indefensible. Skip the junk food, quit the late-night pizza, and stop making excuses! Your body deserves better, and you owe it to yourself to make those changes now.
Understanding the multifaceted impact of gastroesophageal reflux disease (GERD) necessitates an interdisciplinary lens that synthesizes pathophysiological mechanisms, psychosocial determinants, and therapeutic modalities. From a gastroenterological standpoint, the chronic exposure of esophageal mucosa to acid and bile precipitates mucosal inflammation, which can culminate in erosive esophagitis, Barrett's esophagus, and even neoplastic transformation.
Concomitantly, the neurohumoral dysregulation inherent in GERD amplifies visceral hypersensitivity, thereby exacerbating the perception of discomfort and magnifying its intrusion into daily functioning.
From a psychoneuroimmunological perspective, persistent nocturnal reflux episodes disrupt circadian rhythms, attenuating sleep architecture and precipitating systemic inflammation, both of which are well-documented risk factors for mood disorders such as anxiety and depression.
Clinically, the bidirectional relationship between GERD and psychiatric comorbidities underscores the necessity for integrated care pathways that address both somatic and affective symptomatology.
Moreover, the socioeconomic ramifications of uncontrolled GERD cannot be overstated; frequent absenteeism, diminished occupational productivity, and heightened healthcare utilization collectively impose a substantial economic burden.
Patients often report impaired concentration, reduced cognitive bandwidth, and an overall decrement in quality of life metrics, which are quantifiable using validated instruments such as the GERD-HRQL and SF-36 scales.
Therapeutically, lifestyle modifications-including weight reduction, avoidance of trigger foods (e.g., high-fat meals, caffeine, alcohol, chocolate, and acidic fruits), head-of-bed elevation, and temporal separation of meals from sleep-constitute the cornerstone of non-pharmacologic intervention.
Pharmacotherapy, ranging from H2 receptor antagonists to proton pump inhibitors (PPIs), offers symptomatic relief but must be calibrated to mitigate potential adverse effects associated with long-term use, such as nutrient malabsorption and microbiome perturbations.
Surgical options, such as laparoscopic Nissen fundoplication, are reserved for refractory cases and demand a thorough preoperative assessment to balance risk-benefit ratios.
Importantly, patient education and shared decision-making are pivotal; empowering individuals with knowledge about pathogenesis, symptom monitoring, and trigger avoidance fosters adherence and enhances therapeutic outcomes.
Incorporating behavioral health strategies-cognitive-behavioral therapy, mindfulness-based stress reduction, and tailored exercise regimens-can further ameliorate the psychosomatic sequelae of GERD.
Community support structures, including peer-led groups and digital health platforms, provide additional scaffolding for individuals navigating chronic disease management.
Finally, ongoing research into novel therapeutic agents, such as potassium-competitive acid blockers and mucosal protective compounds, promises to expand our armamentarium against GERD's pervasive impact.
In sum, GERD is not merely a trivial heartburn issue; it is a complex, systemic disorder that intrudes upon physical, emotional, and socioeconomic domains, demanding a holistic, patient-centered approach.
What the mainstream media won't tell you is that GERD is part of a larger agenda to keep us dependent on pharmaceutical monopolies. The way they push PPIs like they're miracle drugs is a clear signal of covert control. Wake up, people-your sleep disruption and weight gain are engineered outcomes!
It's understandable to feel overwhelmed when the symptoms intrude on every facet of life. By acknowledging the emotional weight, we can start to disentangle the anxiety from the physical sensations. Mindfulness and gentle breathing exercises often create a buffer between the mind and the reflux sensations.
May I respectfully suggest that establishing clear boundaries with one’s diet is paramount? It is advisable to consult a qualified gastroenterologist to formulate an individualized management plan, thereby ensuring both safety and efficacy.
From a practical standpoint, elevating the head of your bed by about six inches can markedly reduce nocturnal reflux. Also, try to eat your last meal at least three hours before bedtime and keep a symptom diary to identify personal triggers.
lol just skip the spicy stuff.
Stay positive! Small changes = big results.
Implementing a structured meal schedule-preferably small, frequent meals-can mitigate the volume of gastric contents that reflux. Coupled with a low-fat, high-fiber diet, this strategy often yields measurable improvements in symptom frequency.
Reflecting on the human condition, chronic ailments such as GERD remind us of the delicate equilibrium between bodily functions and environmental influences. By fostering awareness of this interplay, individuals can cultivate resilience against such disruptions.
I must formally critique the article’s lack of statistical rigor; no specific prevalence rates or confidence intervals were provided, which undermines its scientific credibility.
Thank you for shedding light on such an important health issue. Your thoroughness is commendable. 🌟👏
Oh sure, because everyone loves waking up with a burning chest-said no one ever. 🙄
Idk, same old thing.
Let’s pool our experiences and create a community guide on trigger foods-that way, we all benefit from collective knowledge.
Picture this: a night without the fiery sting of reflux, where you drift peacefully into sleep, unburdened by the tyranny of acid. That's the destiny we can claim if we rally together and champion evidence‑based interventions.
Great, another blog telling us to “just eat better.” Because that’s never been said before.