Introduction: Understanding Meniere's Disease and Allergies
Meniere's Disease is a disorder of the inner ear that causes symptoms such as vertigo, ringing in the ears, and hearing loss. On the other hand, allergies are a common condition that occurs when your immune system overreacts to a substance, such as pollen or pet dander. But is there a link between Meniere's Disease and allergies? In this article, we'll explore the possible connection between these two conditions and provide you with essential information to better understand this topic.
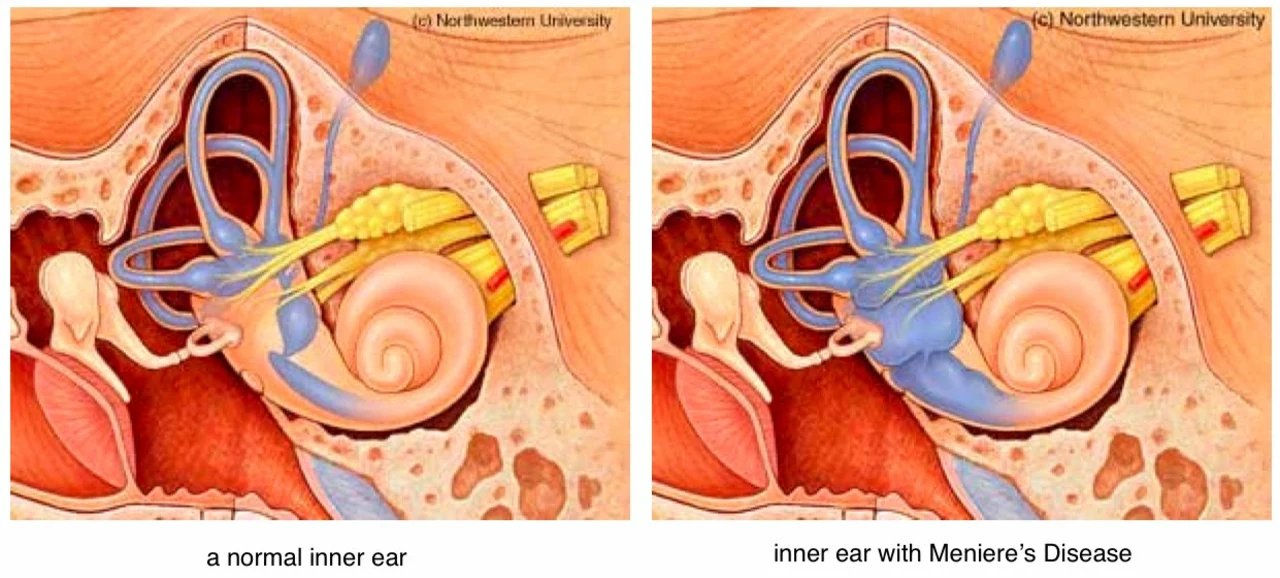
What is Meniere's Disease?
Meniere's Disease is a chronic condition that affects the inner ear, resulting in a range of symptoms that can significantly impact a person's quality of life. The most common symptoms include:
- Vertigo (a sensation of spinning or dizziness)
- Tinnitus (ringing or buzzing in the ears)
- Hearing loss (which can be temporary or permanent)
- A feeling of fullness or pressure in the ear
Although the exact cause of Meniere's Disease remains unknown, it is believed to be related to a build-up of fluid in the inner ear, which can interfere with the proper functioning of the ear's balance and hearing mechanisms.
Common Types of Allergies
Allergies are a widespread condition that affects millions of people worldwide. An allergic reaction occurs when your immune system overreacts to a substance that is typically harmless for most individuals. Some of the most common types of allergies include:
- Hay fever (allergic rhinitis)
- Asthma
- Food allergies
- Drug allergies
- Latex allergies
- Insect sting allergies
Allergies can cause a wide range of symptoms, such as sneezing, runny nose, itchy eyes, skin rashes, and difficulty breathing. In some cases, allergies can even trigger life-threatening reactions, known as anaphylaxis.
Exploring the Possible Connection Between Meniere's Disease and Allergies
Over the years, researchers have looked into the possibility of a link between Meniere's Disease and allergies. Although there is no definitive evidence to prove that allergies cause Meniere's Disease, some studies have suggested that individuals with allergies may be at a higher risk of developing Meniere's Disease.
One theory is that allergies could contribute to the build-up of fluid in the inner ear, which is the main factor associated with Meniere's Disease. Allergic reactions can cause inflammation and swelling, which may potentially affect the inner ear and lead to an increase in fluid levels.
Managing Allergies to Potentially Reduce Meniere's Disease Symptoms
If you have Meniere's Disease and also suffer from allergies, it's essential to manage your allergic reactions effectively. By doing so, you may be able to reduce the severity or frequency of your Meniere's Disease symptoms. Some steps you can take to manage your allergies include:
- Avoiding known allergens whenever possible
- Taking allergy medications as prescribed by your doctor
- Using nasal corticosteroid sprays to help reduce inflammation
- Receiving allergy shots (immunotherapy) to help your body build a tolerance to allergens
It's crucial to discuss your symptoms and treatment options with your healthcare provider, as they can help you determine the best course of action for managing your allergies and Meniere's Disease.
Other Possible Triggers for Meniere's Disease
While allergies may potentially contribute to the development or worsening of Meniere's Disease symptoms, there are several other factors that can also play a role. Some possible triggers for Meniere's Disease include:
- Stress
- High salt intake
- Caffeine
- Alcohol consumption
- Certain medications
It's essential to work closely with your healthcare provider to identify and manage any potential triggers for your Meniere's Disease symptoms.
Diagnosing Meniere's Disease and Allergies
Diagnosing Meniere's Disease can be challenging, as there is no specific test to confirm the condition. Instead, doctors rely on a thorough medical history and a series of tests, such as hearing and balance tests, to rule out other possible causes of your symptoms.
Similarly, diagnosing allergies often involves a detailed medical history and allergy testing, which may include skin tests or blood tests to determine the specific allergens causing your reactions.
If you suspect that you may have Meniere's Disease or allergies, it's crucial to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Conclusion: The Importance of Understanding the Link Between Meniere's Disease and Allergies
Although there is no definitive evidence to prove that allergies cause Meniere's Disease, understanding the potential link between these two conditions can be beneficial for individuals who suffer from both. By effectively managing your allergies and working closely with your healthcare provider, you may be able to reduce the severity or frequency of your Meniere's Disease symptoms and improve your overall quality of life.


Meniere's stuff is kinda weird.
Allergies can totally mess with your ears, so keep those meds handy.
Staying on top of triggers helps keep vertigo at bay.
The inner‑ear fluid dynamics are complex, and inflammatory responses from allergies might influence them.
Clinical observations suggest a modest correlation, though causation remains elusive.
When we contemplate the labyrinthine architecture of the vestibular system, we realize that even subtle perturbations can echo loudly in our lived experience.
Allergic inflammation, though often dismissed as peripheral, possesses the capacity to alter vascular permeability within the endolymphatic space.
This alteration may precipitate an excess of fluid, thereby intensifying the hydrops that underlies Meniere's manifestations.
Yet the philosophical quandary persists: does the allergic cascade act as a primary catalyst or merely as an accomplice to an already vulnerable inner ear?
Consider the seasonal ebb and flow of pollen; many patients report symptom spikes during high‑allergy periods, hinting at a temporal link.
Conversely, individuals with chronic allergic rhinitis sometimes endure years without any vestibular disturbance, suggesting that additional variables modulate risk.
Genetic predisposition, stress hormones, and dietary sodium collectively shape the homeostatic balance.
Thus, attributing causality solely to allergies would be an oversimplification that neglects the multifactorial nature of the disease.
From a therapeutic standpoint, however, targeting the allergic component can be pragmatically beneficial.
Antihistamines, nasal corticosteroids, and immunotherapy have been observed to attenuate vertigo episodes in select cohorts.
These interventions may reduce mucosal edema, indirectly stabilizing inner‑ear pressure.
Nevertheless, the evidence base remains heterogeneous, composed of small case series rather than robust randomized trials.
Clinicians should therefore adopt a personalized approach, weighing the potential benefits of allergy control against the side‑effect profile of each medication.
In summary, while allergies are not a definitive cause of Meniere's disease, they represent a modifiable factor that can influence symptom severity for many patients.
From a scholarly perspective, the purported link between atopic conditions and vestibular pathology warrants rigorous scrutiny.
Current literature offers anecdotal correlations but lacks the statistical power requisite for definitive conclusions.
Dear readers, it is imperative to approach this subject with both scientific rigor and compassionate understanding.
Patients navigating the dual challenges of Meniere's disease and allergic sensitivities deserve comprehensive, evidence‑based guidance.
Oh sure, because taking a daily antihistamine totally cures the spinning world you’re living in. 🙄
i think allergies r kinda like the sneaky villain in a movie.
Yo, if you’ve got both issues, make a plan: diet, meds, and stress‑busting.
Stick to it and you’ll see fewer flare‑ups.
Picture this: a storm of allergens colliding with the delicate canals of the inner ear, creating a symphony of chaos.
The drama is palpable, and the body's response is nothing short of theatrical.
Right, because everyone’s just waiting for the next groundbreaking study on pollen‑induced vertigo. 🙃
Behold, the grand tapestry where allergens weave themselves into the very fabric of equilibrium, daring the vestibular realm to betray its poise.
Such intrigue demands our utmost attention.
I think it helps to keep a simple list of what makes you feel worse and try to avoid those things.
yeah, just cut the salty snacks and watch your vertigo chill out.
Both suggestions are valuable; integrating dietary modifications with a systematic tracking of allergen exposure can empower patients to make evidence‑based adjustments.
Practical steps, like regular follow‑ups and clear documentation, are essential for managing such multifactorial conditions.
Honestly, the medical community is just pushing meds while the real cause is hidden in environmental toxins.