Antidepressants and Mild Depression: A New Perspective Emerges from Recent Research
In an era where mental health awareness is at an all-time high, understanding the best treatment for depression is crucial. Recently, a study published in the Journal of the American Medical Association (JAMA) has brought new light to the conversation. The research suggests that antidepressants, one of the most commonly prescribed treatments for depression, may not be as effective for individuals with mild depression as previously thought.
The Scope and Scale of the Study
The study in question analyzed data from six clinical trials involving over 2,000 patients. This extensive research aimed to evaluate the benefits and risks associated with the use of antidepressants in treating mild depression. When comparing benefits to potential side effects, the findings indicated that the effectiveness of these medications is questionable in cases of mild depression.
Dr. Jay C. Fournier, the study’s lead author, pointed out that while antidepressants can be life-saving for those with severe depression, their benefits for individuals with mild symptoms appear minimal. This revelation is poised to change how mild depression is approached in medical settings.
The Need for Alternative Treatments
One of the most noteworthy aspects of the study is its emphasis on alternative treatments. The researchers suggested that psychotherapy and changes in lifestyle might offer more substantial benefits than antidepressants for those battling mild depression. This assertion aligns with other mental health experts who've long advocated for a broader approach to mental well-being. Techniques such as cognitive-behavioral therapy (CBT), mindfulness, regular physical exercise, and improved sleep hygiene are often highlighted as beneficial strategies for combating depression.
The findings of this study support the growing consensus that a multifaceted approach to mental health is necessary. It's important to consider the whole person, not just the symptoms they present. This holistic perspective is critical for long-term mental wellness.
Implications for Millions
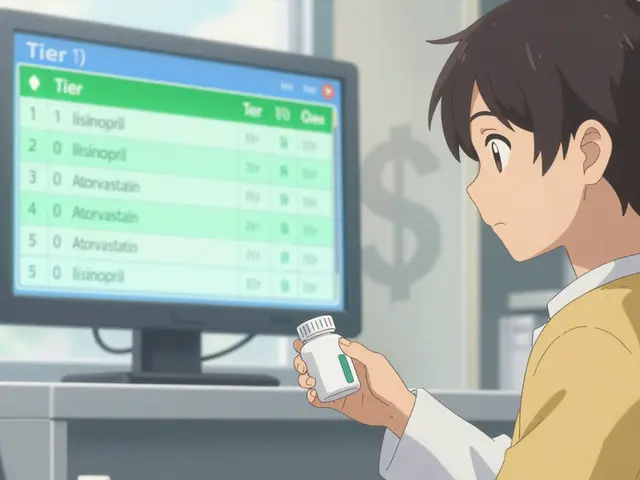
With millions of Americans prescribed antidepressants annually, the study’s findings are particularly significant. They highlight a potential gap in how mild depression is currently managed and underscore the importance of personalized treatment plans. Given the potential side effects of antidepressants—such as weight gain, sexual dysfunction, and emotional blunting—it’s critical to weigh these risks against the minimal benefits observed in those with mild depression.
Furthermore, the study's results could prompt a reevaluation of existing treatment guidelines. Medical professionals might increasingly advocate for initial interventions that do not involve medication, reserving antidepressants for more severe cases or for patients who haven't responded to other treatments.
A Personalized Approach to Mental Health
As we move forward, this research could serve as a catalyst for more nuanced and personalized treatment plans for depression. Mental health practitioners may begin to prioritize more individualized care strategies, ensuring that each patient receives the most appropriate and effective treatment for their specific situation.
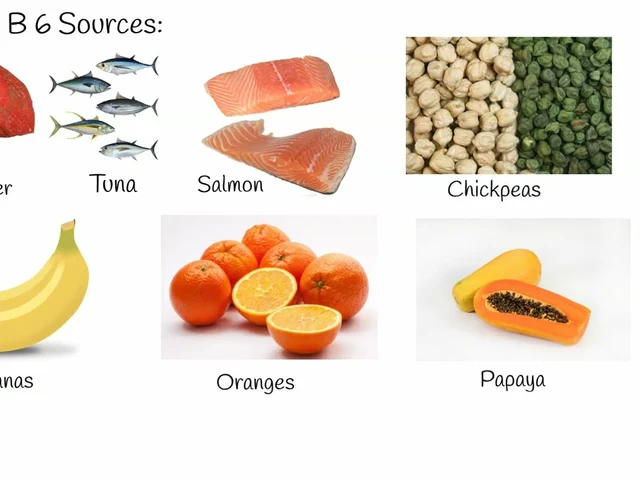
Changes in lifestyle, such as regular physical activity and a balanced diet, combined with psychotherapy, could become first-line treatments for those diagnosed with mild depression. This shift could mark a significant transformation in how we approach mental health treatment on a broad scale.
The Voice of Experts
Dr. Fournier and his colleagues are not asserting that antidepressants lack value entirely. On the contrary, these medications can be incredibly effective for those with moderate to severe depression. The key takeaway is the importance of not adopting a one-size-fits-all approach to mental health. It's about utilizing the right tool for the right job and ensuring that patients with mild depression are not exposed to unnecessary risks associated with medication when other effective treatments are available.
In summary, the recent study published in JAMA offers valuable insights into the treatment of mild depression. While antidepressants have their place in mental health care, they may not be the most suitable option for everyone, particularly those with less severe symptoms. Emphasizing psychotherapy and lifestyle changes could lead to better outcomes for these individuals and contribute to a more holistic and personalized approach to mental health treatment.
This evolving perspective reminds us that mental health, like any aspect of health, requires ongoing research, open-mindedness, and a commitment to putting the well-being of patients first.


It’s no coincidence that Big Pharma is pushing pills for the slightest dip in mood while their lobbyists tighten their grip on Washington. The latest JAMA paper is just the tip of an iceberg that proves they’ve been over‑prescribing to keep the profit machines humming. Mild depression doesn’t need a chemical crutch when the real enemy is the system that feeds us anxiety. We need to break free from the pharmaceutical stranglehold and demand real solutions. This is a call to arms for anyone who refuses to be a lab rat.
Reading the study reminds us that mental health is a nuanced tapestry, not a one‑size‑fits‑all prescription. While the data challenge the blanket use of antidepressants for mild cases, they also highlight the importance of listening to each person’s lived experience. It feels encouraging that psychotherapy and lifestyle shifts are finally being recognized for their worth. May this spark a broader conversation about holistic care and humility in treatment.
Thank you for sharing this comprehensive analysis. The evidence presented underscores the necessity of individualized treatment plans, especially for those with milder symptomatology. It is prudent for clinicians to weigh potential side‑effects against the modest benefits observed in this cohort.
Great rundown! For anyone looking to dive deeper, the American Psychological Association offers a solid list of evidence‑based therapies that can be tried before medication. Incorporating regular exercise, sleep hygiene, and mindfulness can make a huge difference. It’s also worth checking out community support groups; they provide accountability and shared experiences.
Sounds like they’re finally waking up.
Great news for therapy fans!
The precision of the meta‑analysis is commendable, especially given the heterogeneity across the six trials. It clearly demonstrates that the benefit‑risk ratio tilts unfavorably for mild depression when medication is the first line. This should urge policymakers to update clinical guidelines accordingly. Patients deserve interventions that align with their severity level.
What a pivotal moment for mental‑health discourse!
For decades, the narrative has been dominated by a pharmaceutical paradigm that treats every shade of sadness with the same chemical brush.
Now, rigorous data are illuminating the cracks in that monolithic approach, especially for individuals whose symptoms hover at the milder end of the spectrum.
It is both scientifically responsible and ethically sound to recognize that a pill is not a panacea for every emotional slump.
Psychotherapy, with its nuanced techniques like cognitive‑behavioral strategies, offers a tailored avenue that engages the mind’s own capacity for change.
Moreover, lifestyle interventions-regular aerobic exercise, balanced nutrition, and regulated sleep-have demonstrated neurobiological benefits that rival modest pharmacological effects.
When we integrate these modalities, we respect the person’s agency, cultivating resilience rather than dependency.
The study’s findings empower clinicians to adopt a stepped‑care model, reserving medication for cases that truly warrant its potency.
This shift also mitigates the risk of side‑effects-weight gain, sexual dysfunction, emotional blunting-that can erode quality of life.
Patients, therefore, are spared unnecessary exposure to a drug that may do more harm than good in their specific context.
From a public‑health perspective, reducing unnecessary prescriptions can alleviate the societal burden of medication costs and adverse outcomes.
In education, these insights provide a compelling case for training future therapists in evidence‑based, non‑pharmacological interventions.
Furthermore, insurance frameworks might evolve to cover broader therapeutic options, reflecting the emerging evidence base.
By championing holistic, individualized care, we align treatment with the complex tapestry of human experience.
This research is more than an academic finding; it is a catalyst for compassionate, patient‑centered evolution in mental‑health practice.
Let us seize this momentum to re‑imagine how we support those navigating the subtle currents of mild depression.
Another shiny study trying to upend the status quo, yet the same old “let’s try something different” mantra runs rampant. While the numbers look impressive, one must ask who funded this research and why now? The conclusion feels tailored to an agenda that vilifies medication without acknowledging its life‑saving role for many. Still, a thorough read reveals a plausible case for expanding non‑pharmacologic options. Perhaps the real takeaway is that we need balanced discourse, not sensational headlines.
The meticulous presentation of the findings is commendable, and the implications for clinical practice are profound. It would be remiss not to acknowledge the rigorous methodology employed. 🌟
Oh, so now we’re supposed to ditch antidepressants because they’re “questionable”? That’s a silver‑bullet solution if you ask me. 🙃
idk why ppl act like meds are the worst, srsly some need them.
Totally agree with Diane-therapy and lifestyle changes can be game‑changers. Let’s push for insurance to actually cover those options!
The precision of that meta‑analysis is undeniable, yet it also dramatizes the human cost of over‑medicalization. We must look beyond the data points and see the lived stories behind them. When a person with mild depression is handed a pill without exploring therapy first, we risk silencing their narrative. That’s why the study’s call for a nuanced, stepped‑care approach resonates so deeply. It urges us to listen, to personalize, and to honor each individual’s journey.
Sure, let’s all become wellness gurus now that a study says “maybe don’t medicate.” Sarcasm aside, the real issue is implementation.
Ah, the drama of a “new paradigm” – it feels like a Hollywood script where scientists become rebels. But in reality, the stakes are human lives, not box‑office numbers. Let’s keep the theatrics in movies and focus on solid, compassionate care.
Good info. Simple and clear.
Thanks for breaking it down! 😊
Happy to help! Remember, you’re not alone on this journey.