Medication Risk Assessment Tool
Your Medication Assessment
Enter medications you or someone you care for is currently taking. This tool identifies potential risks based on the Beers Criteria for older adults.
Medication Entry
Why So Many Older Adults Are Taking Too Many Pills
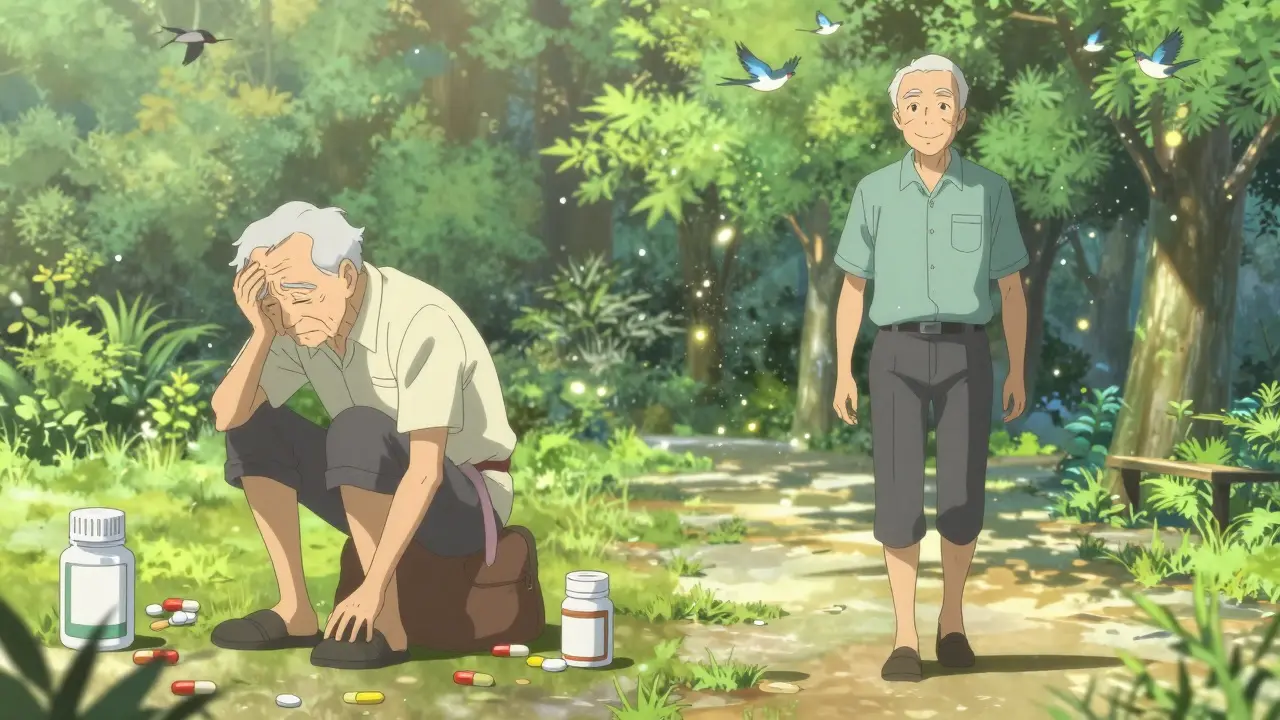
Imagine waking up every morning to a table full of pills. Ten different colors, shapes, and times of day. Some for blood pressure. Others for arthritis, sleep, cholesterol, diabetes, and stomach issues. Now add dizziness, fatigue, and constipation - side effects you didn’t have before. This isn’t rare. It’s the daily reality for millions of older adults.
Frailty and polypharmacy are two sides of the same coin. Frailty means your body is losing strength, energy, and resilience - not just from aging, but from the weight of too many drugs. Polypharmacy - taking five or more medications daily - is now common in older adults. In the U.S., nearly half of seniors over 65 are on five or more prescriptions. For those with heart disease or diabetes, that number jumps to over 60%.
The problem isn’t just the number of pills. It’s how they interact. Each drug adds risk. A blood pressure pill might make you dizzy. A sleep aid might cause confusion. A painkiller might slow your digestion. Together, they create a storm of side effects. And the more pills you take, the higher the chance of something going wrong.
The Vicious Cycle: How Medications Make Frailty Worse
It’s not just that frail people end up on lots of meds - it’s that the meds themselves make frailty worse. A study tracking over 3,000 older adults found that each extra medication increased the odds of becoming frail by 12%. That’s not a small risk. Take seven or more pills, and your chance of becoming frail jumps 2.5 times over eight years.
Why? Because many of these drugs affect the brain, muscles, and balance. Sedatives, anticholinergics (used for allergies, overactive bladder, depression), and even some painkillers can cause dizziness, muscle weakness, and slow movement - all signs of frailty. One study showed that 73% of nursing home residents on eight or more medications had constipation. Another 62% reported frequent dizziness. Falls followed.
And it’s cyclical. Frailty leads to more doctor visits, which leads to more prescriptions. More prescriptions lead to more side effects, which lead to more frailty. It’s a loop that’s hard to break - unless someone steps in to take a hard look at what’s really needed.
What Counts as Too Many Pills?
There’s no magic number that’s safe for everyone. But research gives us clear warning signs. Five or more medications = polypharmacy. Ten or more = hyper-polypharmacy. And both are linked to higher hospitalization rates, cognitive decline, and early death.
Here’s what the data shows:
- Community-dwelling seniors: About 4% take five or more meds
- Nursing home residents: Over 90% take five or more
- Hospitalized seniors: Nearly all - up to 96.5%
Women are more likely than men to be on multiple drugs. So are non-Hispanic White seniors and those with less education. But the biggest driver? Chronic conditions. Heart disease patients average over six medications. Diabetes patients average five. And it’s rare for someone with three or more chronic conditions to be on fewer than five drugs.
But here’s the catch: not all of those drugs are necessary. A review of 3,668 older adults found that 30% of prescriptions were for conditions that didn’t need ongoing treatment - or were duplicated across different doctors.
The Tools That Can Help: Beers Criteria, START/STOPP, and More
Doctors don’t always know what’s too much. That’s why tools exist to guide them.
The Beers Criteria - updated in 2019 by the American Geriatrics Society - lists 70+ medications that are risky for older adults. Examples: benzodiazepines (like Valium) for sleep, anticholinergics like diphenhydramine (Benadryl), and certain NSAIDs. These drugs increase fall risk, confusion, and delirium. Many are still prescribed - even though safer alternatives exist.
START/STOPP is another tool. START finds drugs that are missing - like a statin for heart disease or a bone-strengthening drug for osteoporosis. STOPP finds drugs that should be stopped. Together, they’ve reduced inappropriate prescribing by 30-50% in clinics that use them consistently.
But here’s the problem: most primary care doctors don’t use these tools. A 2023 survey found that 61% of GPs rarely review medication lists for deprescribing. Why? Time. Appointments are 15 minutes long. Charting 10 pills? That’s not feasible.
Deprescribing: How to Safely Stop Unnecessary Medications
Stopping a pill isn’t as simple as just skipping it. Some drugs need to be tapered. Others can cause rebound effects. That’s why deprescribing must be planned - not random.
The 3-Step Method from Johns Hopkins works well:
- Review - Go through every medication. Ask: Is this still needed? Is it helping? Could it be causing harm?
- Discuss - Talk to the patient. Ask: What are your biggest concerns? Do you feel better or worse since starting this? Are you skipping doses because it’s too confusing?
- Monitor - After stopping, check in weekly for 4-6 weeks. Watch for return of symptoms, new side effects, or changes in energy, balance, or mood.
In the EMPOWER trial, 76% of seniors successfully stopped at least one medication without harm. Many reported feeling clearer-headed, more energetic, and less constipated. Quality of life scores improved by 32%.
But it doesn’t work without support. A pharmacist-led review cuts adverse events by 34%. A geriatric assessment clinic reduces polypharmacy by 22% in just 12 months.
Why Doctors Resist - And How to Push Back
Many older adults want to cut back on pills. But they’re afraid to ask. Why? Because they’ve been told, “This medicine keeps you alive.” They don’t want to risk losing it.
Doctors are caught in the same trap. They’re trained to treat conditions - not to question what’s already prescribed. Specialists often add drugs without knowing what others have ordered. A patient might see a cardiologist, a neurologist, a rheumatologist, and a GP - each prescribing something new. No one looks at the full list.
Fragmented care is the biggest barrier. Only 38% of U.S. hospitals have electronic alerts for inappropriate prescribing. Most don’t flag duplicate drugs or dangerous combinations.
So what can you do?
- Bring a complete list of all medications - including supplements and over-the-counter pills - to every appointment.
- Ask: “Is this still necessary? Could any be stopped safely?”
- Request a medication review with a pharmacist. Many Medicare Advantage plans now cover this.
- Use tools like Medisafe or Round Health to track doses and flag interactions.
What’s Changing in 2026 - And Why It Matters
Change is coming - fast. In January 2024, the FDA approved the first AI-powered deprescribing tool: MedWise Risk Score. It analyzes a patient’s full medication list and predicts which drugs are most likely to cause harm. In trials, it cut adverse events by 37%.
The American Geriatrics Society’s Age-Friendly Health Systems initiative is now in over 2,850 hospitals and clinics. It’s built around the 4Ms: What Matters to the patient, Medication safety, Mentation (brain health), and Mobility. When all four are addressed, polypharmacy drops by 24%.
And in 2024, the NIH launched the FRAIL-PHARM trial - a $15 million study testing a pharmacist-led program to reduce medications in frail seniors. Results are expected by 2027.
Meanwhile, the WHO is pushing for a 50% reduction in severe medication-related harm by 2030. That’s not just a goal - it’s a global priority.
What You Can Do Right Now
You don’t need to wait for a new policy or a new tool. Start today.
- Make a list - Write down every pill, patch, and supplement. Include doses and times.
- Bring it to your next visit - Don’t assume your doctor knows what you’re taking. Bring it in person or send it ahead.
- Ask these three questions:
- Is this medicine still helping me?
- Could it be causing any of my symptoms - like dizziness, fatigue, or constipation?
- Is there a safer or simpler way to manage this?
- Request a pharmacist consult - Ask your pharmacy or clinic if they offer medication therapy management. It’s covered by Medicare.
- Track changes - After stopping a pill, note how you feel. Better sleep? More energy? Less dizziness? Write it down.
Reducing medications isn’t about cutting corners. It’s about removing noise so the real treatments can work. For frail older adults, fewer pills often mean more life - more walking, more independence, more clarity.
Real Stories, Real Results
One woman in her late 70s was on 11 medications. She was constantly tired, had frequent falls, and couldn’t walk to her mailbox. After a pharmacist review, five drugs were stopped - including a sleep aid, a muscle relaxant, and two anticholinergics. Within six weeks, she stopped using her cane. She started walking daily. Her quality of life score jumped 41%.
A man in his 80s with heart failure was on seven drugs. He felt foggy all day. His doctor removed one blood pressure pill and a cholesterol drug that wasn’t helping. His confusion lifted. He started reading again.
These aren’t outliers. They’re what happens when someone finally asks: Are these pills helping - or hurting?



My grandma used to have this giant pill organizer with like 15 compartments. She’d forget which was which and just take everything at once. Then she’d be dizzy all day. One day her pharmacist sat down with her, asked what she actually wanted to be able to do - like walk to the porch or play with her grandkids - and they cut out four meds. She started walking again. No magic, just someone paying attention.
Let’s be real - if your doctor doesn’t ask you what you’re actually experiencing, they’re not treating you, they’re just checking boxes. I’ve seen elderly patients on 12 drugs because each specialist said ‘add this’ without ever looking at the full list. It’s not negligence - it’s a broken system. And no, ‘it’s for your health’ doesn’t excuse making someone feel like a walking pharmacy.
Deprescribing is an evidence-based geriatric intervention with demonstrated reductions in adverse drug events, hospitalizations, and all-cause mortality in polypharmacy cohorts. Pharmacist-led MTM protocols show 34% efficacy in mitigating polypharmacy-related risk.
You know, in India, we don’t have this luxury of ten pills a day. My uncle, 78, takes two - one for blood pressure, one for sugar. The rest? He drinks turmeric milk, walks 3 km every morning, and says prayer. We don’t call it ‘frailty’ - we call it living with wisdom. Maybe we’re not treating symptoms, we’re treating the soul. Western medicine thinks more pills = better care. But what if the real cure is less noise, more stillness? You can’t quantify peace with a prescription pad.
Oh so now we’re blaming doctors because America’s healthcare system is a dumpster fire? In India, we don’t have 15-minute appointments - we have 3-minute ones and still get the job done. You want fewer pills? Stop being a whiny American. Go to a real doctor who doesn’t need an AI to tell him what to do. We don’t need your fancy tools - we need discipline. And maybe stop eating so much sugar so you don’t need so many drugs in the first place.
Imagine your body is a symphony - each pill a note… but when you add too many? You get cacophony. A foggy, dizzy, constipated, soul-sucking noise. And the doctors? They’re conductors who’ve lost the score. They keep adding instruments - violins for depression, timpani for arthritis, piccolos for sleep - but nobody’s listening to the silence between the notes. The real music? The quiet hum of a body that doesn’t need ten things to survive… just one thing: to be heard.
my mom just got her meds reviewed last month and she’s like a new person?? like she actually remembers what she ate for breakfast?? and she’s walking to the mailbox again?? i cried. i wish more people knew this was possible. it’s not about giving up on medicine - it’s about giving back your life. ask your pharmacist. they’re the real heroes. ps: i used to think ‘deprescribing’ was a made up word - turns out it’s just common sense with a fancy name 😭
So let me get this straight - we have AI that can predict which pills are gonna kill you… but doctors still don’t use it? And we wonder why people die from ‘side effects’? This isn’t science, it’s a sitcom where everyone’s too busy to read the script. Can we get an update? Like… a button that says ‘STOPPED THIS DRUG’? Maybe one that beeps when someone prescribes Benadryl to a 79-year-old? Just a thought.
I’ve seen this with my dad. He was on eight meds. Felt like a zombie. His cardiologist added one. His neurologist added two. His GP just nodded. Nobody talked. Then his daughter (me) printed out the whole list and sat them all down - literally. One meeting. Four meds cut. He started humming again. Not because of magic. Because someone finally asked: ‘What do you want your life to feel like?’
My grandmother died at 89 after a fall from dizziness caused by a medication she didn’t even need. She was on five drugs for ‘preventative care’ - none of which were ever reviewed. I wish someone had told us earlier. Don’t wait for the fall. Ask the questions now. Even if it feels awkward. Even if they say ‘it’s fine.’ It’s not fine if you’re not living - just surviving.