Introduction to Warfarin and Drug-Induced Lupus
As a blogger who has been researching and writing about various medications and their potential side effects, I have come across a rare but serious side effect of the anticoagulant medication Warfarin - drug-induced lupus. In this article, I will provide a comprehensive overview of this rare condition, its symptoms, diagnosis, and treatment options. I will also discuss the importance of being aware of this potential side effect if you or a loved one is taking Warfarin.
Understanding Warfarin as an Anticoagulant
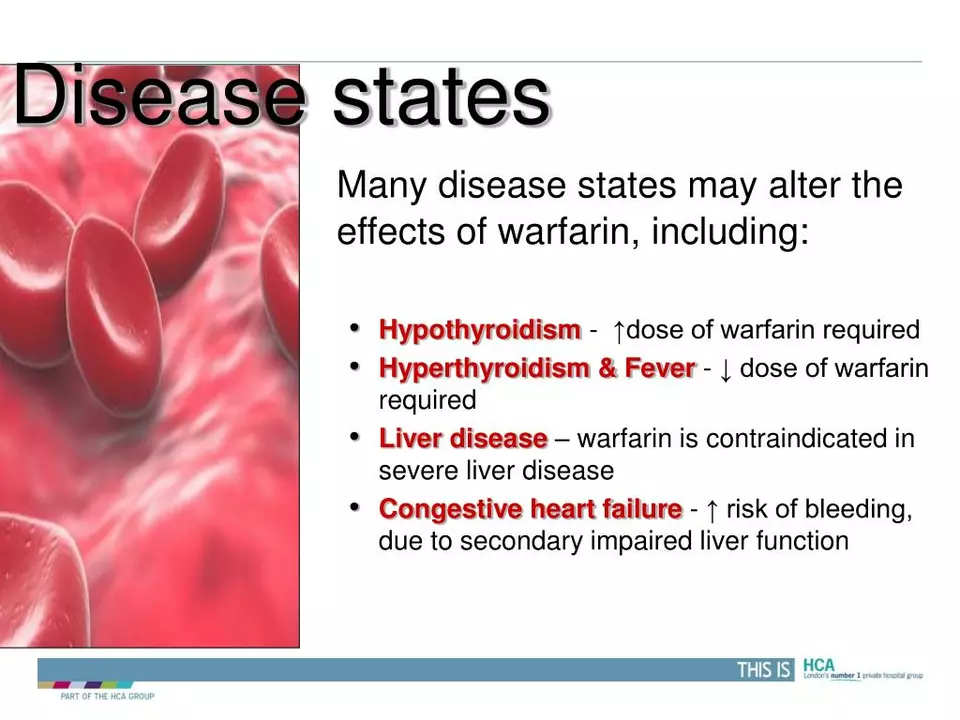
Warfarin is a widely prescribed anticoagulant medication that is commonly used to treat and prevent blood clots in patients with various medical conditions, such as deep vein thrombosis (DVT), pulmonary embolism (PE), and atrial fibrillation. It works by blocking the action of vitamin K, which is essential for the synthesis of clotting factors in the liver. By doing so, Warfarin helps to reduce the risk of blood clots forming and causing serious health complications.
What is Drug-Induced Lupus?
Drug-induced lupus is a rare autoimmune condition that occurs as a result of taking certain medications, including Warfarin. It is characterized by the production of autoantibodies that attack the body's own healthy tissues, causing inflammation and damage to various organs and systems. The symptoms of drug-induced lupus can vary widely and often mimic those of systemic lupus erythematosus (SLE), a more common form of lupus.
Drug-Induced Lupus vs. Systemic Lupus Erythematosus
While both drug-induced lupus and systemic lupus erythematosus share many similarities, there are some key differences between the two conditions. Drug-induced lupus is specifically caused by the use of certain medications, whereas the cause of SLE is not well understood. Additionally, drug-induced lupus typically resolves once the offending medication is discontinued, while SLE is a chronic condition that requires long-term management.
Symptoms of Drug-Induced Lupus
As mentioned earlier, the symptoms of drug-induced lupus can vary significantly from one individual to another. Some of the most common symptoms include joint pain and swelling, muscle pain, fatigue, fever, skin rash, and sensitivity to sunlight. In more severe cases, drug-induced lupus can also affect the kidneys, lungs, heart, and nervous system, leading to more serious complications.
Diagnosing Drug-Induced Lupus
Diagnosing drug-induced lupus can be challenging due to its variable symptoms and the fact that it mimics other autoimmune conditions, such as SLE. A thorough medical history, including a detailed review of medications, is essential in the diagnostic process. Blood tests to check for the presence of specific autoantibodies, such as antihistone antibodies, can also help to confirm the diagnosis. In some cases, a biopsy of affected tissue may be necessary to rule out other potential causes of the symptoms.
Treatment Options for Drug-Induced Lupus
The primary treatment for drug-induced lupus is discontinuation of the offending medication, such as Warfarin. In most cases, symptoms will begin to improve within a few weeks of stopping the medication, and complete resolution is usually seen within several months. During this time, symptomatic treatment with nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or other immunosuppressive medications may be necessary to control inflammation and alleviate symptoms. It is important to work closely with your healthcare provider to develop an appropriate treatment plan.
Preventing Drug-Induced Lupus
While it may not be possible to completely prevent drug-induced lupus, being aware of the potential risk associated with certain medications, such as Warfarin, can help to minimize the chances of developing this rare condition. If you are prescribed Warfarin or any other medication associated with drug-induced lupus, make sure to discuss the potential risks with your healthcare provider and be vigilant about monitoring for any signs or symptoms of the condition.
Conclusion: The Importance of Awareness and Monitoring
In conclusion, while drug-induced lupus is a rare side effect of Warfarin, it is essential for both patients and healthcare providers to be aware of this potential risk. By closely monitoring for any signs or symptoms of drug-induced lupus and working together to develop an appropriate treatment plan, patients can minimize the risk of serious complications and maintain their overall health and well-being.



Hey folks, just wanted to point out that warfarin’s benefits usually far outweigh rare side effects. If you’re on it, keep your INR in range and stay in touch with your doc. Monitoring labs regularly can catch weird immune responses early. And remember, not every rash means lupus – stay calm and get checked properly.
Do you really think it’s just a simple medication? The pharma giants hide the truth about warfarin’s autoimmune triggers. It’s a deliberate experiment to weaken our immune defenses. Wake up before they turn us into lab rats for their secret agendas!
The moral imperative here is crystal clear; physicians must disclose every obscure risk; patients deserve full transparency. Ignoring rare events, such as drug‑induced lupus, is an ethical violation. It is not merely a "side effect"-it is a breach of trust. One must demand rigorous informed‑consent protocols. Moreover, the literature is replete with overlooked cases, and yet they remain under‑reported. This negligence cannot be tolerated.
Just stop chattin, u gotta check ur meds.
From a pharmacovigilance perspective, the mechanistic underpinnings of warfarin‑associated autoimmunity warrant a comprehensive ontological mapping. The inhibition of vitamin K‑dependent gamma‑carboxylation pathways may inadvertently modulate epitope presentation, thereby fostering autoreactive T‑cell clones. This hypothesis aligns with the broader immunometabolic paradigm wherein coagulation cascades intersect with innate immune signaling networks. Moreover, the temporal latency observed in drug‑induced lupus suggests a cumulative immunogenic threshold, implicating epigenetic reprogramming of hematopoietic progenitors. Clinically, the phenotypic heterogeneity-ranging from cutaneous photosensitivity to nephritic manifestations-reflects divergent organ‑specific autoantibody repertoires. Serological assays consistently reveal antihistone IgG dominance, yet cross‑reactivity with anti‑double‑strand DNA antibodies is not unprecedented. Therapeutically, cessation of the offending agent remains the cornerstone, but adjunctive immunomodulation with low‑dose corticosteroids may accelerate resolution of systemic inflammation. Long‑term follow‑up studies indicate a favorable prognosis, provided that drug withdrawal is prompt and comorbidities are optimally managed. Therefore, it is incumbent upon clinicians to integrate routine autoantibody screening into the monitoring protocol for patients on long‑term warfarin therapy, especially those with pre‑existing autoimmune predispositions. By adopting a precision‑medicine framework, we can mitigate the iatrogenic burden of drug‑induced lupus while preserving the antithrombotic efficacy of warfarin.
Patriotic Americans must ask why a medication, once a staple of our war‑fighters, is now laced with hidden immunological traps. The deep‑state colludes with Big Pharma to sabotage our health sovereignty. Wake up, brothers and sisters, before they turn our blood thinners into weapons of silent oppression!
I hear the concerns and appreciate the passion. It’s essential to balance vigilance with evidence‑based practice, especially when navigating complex autoimmune phenomena. Let’s foster a compassionate dialogue that supports patients while scrutinizing the data responsibly.
Dear community, I respectfully advise maintaining professional decorum when discussing pharmacological risks. It is prudent to consult peer‑reviewed literature and adhere to established clinical guidelines. Thank you for your attention to this matter.
Happy to help! If you or someone you know is on warfarin and notices any new joint pain, rash, or unusual fatigue, schedule an appointment to get antibody testing done. Regular INR checks combined with a symptom log can catch issues early. And don’t hesitate to ask your provider about alternative anticoagulants if concerns persist.