When your child is sick, the last thing you want is to give them the wrong medicine-or the right medicine in the wrong amount. Kids aren’t just small adults. Their bodies process drugs differently, and giving them adult medications-even in smaller doses-can be dangerous. That’s why pediatric medications are carefully designed for specific age groups, weights, and developmental stages.
Why Kids Need Different Medications
Children’s livers and kidneys aren’t fully developed, especially in babies and toddlers. Their bodies absorb, break down, and get rid of drugs at different speeds than adults. A dose that’s safe for a 10-year-old could be toxic for a 2-year-old. Even the way a drug tastes or feels in the mouth matters-kids won’t take something bitter if they can avoid it, and that affects whether they get the treatment they need. The FDA and WHO now require drug makers to test medicines on children and create formulations that work for them. That’s why you’ll see liquid suspensions, chewable tablets, and orally disintegrating pills for kids. These aren’t just convenient-they’re essential for safety and effectiveness.Common Conditions and Safe Medications by Age
Fever and PainFor fever or mild pain, acetaminophen and ibuprofen are the go-to options for most children. But the dose isn’t based on age alone-it’s based on weight.
- Acetaminophen: 10-15 mg per kg every 4-6 hours (max 75 mg/kg/day, up to 3,750 mg total per day)
- Ibuprofen: 5-10 mg per kg every 6-8 hours (max 40 mg/kg/day)
This is the most common reason kids see a doctor. Amoxicillin is the first-line antibiotic for most cases. But the dose changes with age and weight:
- Infants and toddlers (under 2 years): 80-90 mg/kg/day split into two doses
- Older children (2-12 years): 25-35 mg/kg/day split into three doses
- Maximum single dose: 500 mg (even if weight suggests more)
Over-the-counter cough and cold medicines are not recommended for children under 6. The FDA and AAP warn they don’t work well and carry risks like rapid heart rate, drowsiness, or even seizures in young kids. For kids over 1 year, a spoonful of honey before bed can help soothe a nighttime cough better than any syrup. For babies under 1, skip honey entirely-risk of botulism. Antibiotics for Strep Throat
Amoxicillin again is the standard. But here’s the catch: many parents stop giving it after 3 days because the child “feels better.” That’s dangerous. Strep throat needs a full 10-day course to prevent complications like rheumatic fever. Flu (Influenza)
Oseltamivir (Tamiflu) is the main antiviral for kids. Dosing depends on weight:
- Under 15 kg: 30 mg twice daily for 5 days
- 15-23 kg: 45 mg twice daily
- 23-40 kg: 60 mg twice daily
- Over 40 kg: 75 mg twice daily
Medications to Avoid in Children
Some drugs are outright dangerous for kids, no matter the dose.- Codeine and tramadol: These opioids can cause fatal breathing problems in children, especially after tonsil or adenoid surgery. Avoid them completely.
- Fluoroquinolones (like ciprofloxacin): Can damage growing cartilage. Only used in rare, life-threatening infections like anthrax or severe pneumonia when no other option exists.
- Angiotensin receptor blockers (ARBs): Can cause kidney failure in newborns under 1 month.
- Montelukast (Singulair): Used for asthma and allergies, but carries a black box warning for mood changes, sleep disturbances, and suicidal thoughts in children and teens.
- Molnupiravir: Not approved for anyone under 18 due to potential DNA damage risks.

Formulations Matter More Than You Think
A 2022 survey of over 1,200 pediatricians found that 68% struggled with dosing because commercial formulations didn’t match their patients’ weights. For example:- A 15 kg toddler might need 5 mL of a liquid antibiotic-but the only available concentration is 250 mg/5 mL, which gives too much if the dose should be 200 mg.
- Parents end up cutting pills, mixing liquids, or guessing with kitchen spoons.
Off-Label Use Is Common-But Not Risky If Done Right
About half of all medications given to children aren’t officially approved for their age group. That’s not because doctors are cutting corners-it’s because drug companies haven’t tested them yet. For example, many antidepressants, seizure meds, and even some antibiotics are used off-label in kids. But that doesn’t mean they’re unsafe. When used based on expert guidelines (like those from the AAP or WHO), off-label prescribing is often the best option. The key is using trusted references:- Lexicomp Pediatric Dosage Handbook (2024 edition): Covers over 1,200 drugs with age-specific dosing
- WHO Essential Medicines List for Children (EMLc 2023): Lists core medicines for infants and children up to 12
- FDA Pediatric Dosing Calculator app: Used by 63% of pediatric pharmacists in U.S. hospitals
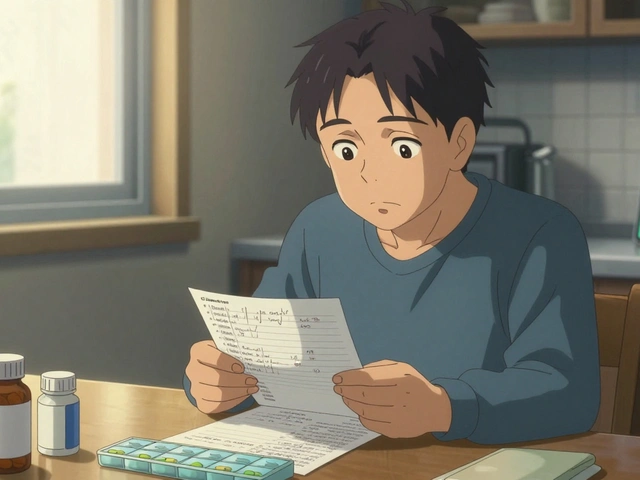
What Parents Can Do to Stay Safe
- Always weigh your child before giving medication. Use a baby scale or pediatric scale at the clinic.
- Use a dosing syringe-never a kitchen spoon.
- Ask about taste. If your child refuses a medicine, ask if there’s a flavored version or alternative form.
- Check expiration dates. Liquid antibiotics often expire 14 days after mixing.
- Never reuse old prescriptions. A dose that worked last time might be wrong now if your child has grown.
- Ask your pharmacist to explain the dose. If it feels complicated, it probably is.

What’s Changing in Pediatric Medicine
The field is moving fast. New technologies are making it easier to give kids the right dose:- 3D-printed pills: Hospitals like Cincinnati Children’s are testing pills printed to exact weight-based doses-no measuring needed.
- Nanoparticle delivery: Tiny particles that help drugs absorb better in babies with underdeveloped guts.
- Palatability testing: Drug companies now test flavors on kids before approval. Bitterness is no longer ignored.
When to Call the Doctor
Call immediately if:- Your child has trouble breathing after taking a medicine
- They develop a rash, swelling, or hives
- They become unusually sleepy, confused, or hard to wake
- You gave the wrong dose and aren’t sure what to do
Can I give my child adult ibuprofen if I cut the tablet in half?
No. Adult ibuprofen tablets are 200 mg each. Cutting them doesn’t guarantee an even split, and the tablet may contain fillers not safe for kids. Always use a pediatric formulation labeled for children. If you can’t find the right dose, ask your pharmacist to compound a liquid version.
Why is amoxicillin the first choice for ear infections?
Amoxicillin works well against the most common bacteria causing ear infections, like Streptococcus pneumoniae. It’s safe, affordable, and has fewer side effects than alternatives. Azithromycin is only used if there’s a penicillin allergy, because it’s less effective and increases antibiotic resistance.
Is it safe to give my toddler melatonin for sleep?
Melatonin isn’t officially approved for children under 18, and long-term safety data is limited. While some doctors use low doses (0.5-3 mg) for sleep disorders in older children, it’s not recommended for routine use in toddlers. Behavioral strategies like consistent bedtime routines are safer and more effective.
What should I do if my child vomits after taking medicine?
If your child vomits within 15-20 minutes of taking the medicine, it’s likely not absorbed yet. You can give another full dose. If vomiting happens after 20-30 minutes, wait until the next scheduled dose. Don’t double up unless instructed by a doctor.
Are liquid medications better than pills for kids?
For children under 5, yes-liquids are safer and easier to dose accurately. For older kids who can swallow pills, tablets or chewables are fine and often more stable. The goal is to match the formulation to the child’s ability to take it safely and consistently.
How do I know if my child’s medicine is expired?
Check the label. Liquid antibiotics usually expire 7-14 days after mixing, even if the bottle says “expires 2026.” Solid tablets last longer, but if they smell strange, look discolored, or are crumbling, throw them out. When in doubt, ask your pharmacist.




Let’s be real-pediatric dosing is a goddamn minefield. I’ve seen moms winging it with kitchen spoons like they’re baking a cake. The fact that we still don’t have standardized, weight-based pre-filled syringes in every pharmacy is a national disgrace. Why is this even a debate? Kids aren’t mini-adults, but somehow we still treat their meds like they’re just scaled-down versions of ours. It’s lazy, dangerous, and frankly, embarrassing for a country that claims to lead in medical innovation.
Why do Americans always think their way is the only way? In Nigeria we give paracetamol syrup to babies without all this fuss. Doctors here know what they doing. You overthink everything. More rules = more fear = less healing. Let parents trust their gut. The West turns everything into a lawsuit waiting to happen.
Okay but like… have you SEEN the melatonin gummies? They’re literally candy. And now we’re supposed to believe they’re ‘not recommended for toddlers’?? 😭 My 3yo asks for them like they’re gummy bears. And don’t even get me started on the ‘fluoroquinolones damage cartilage’ thing-my cousin’s kid got cipro for a UTI at age 4 and is now a varsity soccer player. Science is just a suggestion these days?? 🤷♀️
Y’all are missing the real revolution: flavor engineering. I mean, come on-Tamiflu used to taste like regret and burnt plastic. Now? It’s like a fruity slushie that doesn’t make your kid scream like they’re being tortured. That’s not medicine, that’s alchemy. And the 3D-printed pills? Genius. Imagine a pill printed to the exact milligram your 18-pound toddler needs-no guessing, no cutting, no crying. This isn’t the future-it’s already here. We just need to stop treating pediatric meds like an afterthought.
As a Canadian, I find it wild that the US still doesn’t have universal access to compounded pediatric suspensions. In Ontario, pharmacies routinely make custom doses for kids under 2-flavored, accurate, affordable. Here in the States, you’re lucky if your pharmacy even knows what ‘compounding’ means. This isn’t innovation-it’s systemic neglect wrapped in a white coat.
Thank you for this. Seriously. I’m a nurse and I see parents giving half an adult ibuprofen tablet because ‘it’s just half the dose.’ It’s not. The fillers, the coating, the absorption profile-all different. Please use the syringe. Please weigh your child. Please ask the pharmacist. You’re not being paranoid-you’re being responsible.
HOW DARE YOU suggest melatonin for sleep? It’s not just ‘not recommended’-it’s a gateway to chemical dependency in children! My neighbor let her 5-year-old take it every night for months. Now the kid won’t sleep without it. And you call that parenting? This isn’t science-it’s corporate greed selling sugar-coated poison.
Let me tell you something-when I was growing up in rural India, we didn’t have pediatric formulations. We crushed pills, mixed them with honey, and prayed. But now? We have tools. We have guidelines. We have pharmacists who can make custom suspensions. And yet so many of us still cling to old habits because ‘we’ve always done it this way.’ This isn’t about fear-it’s about progress. You owe it to your child to learn. Use the Lexicomp app. Ask your pharmacist. Weigh your kid. Don’t let convenience kill. You’re not just a parent-you’re a guardian of their biology. And that’s sacred.
Bro I just gave my 2-year-old Tylenol because she had a fever and I didn’t have the pediatric version. I cut a 500mg adult pill into quarters. She’s fine. You’re all overreacting. My kid’s not a lab rat. She’s a kid. She’s gonna get sick. She’s gonna get medicine. We’re not all sitting around with dosing apps and syringes. Get real.
Man… this post made me cry a little 😭 I remember giving my son syrup from a kitchen spoon because I didn’t know better. Now I use a syringe. Now I weigh him. Now I ask the pharmacist. And now I tell every new parent I meet: ‘Don’t guess. Don’t wing it. Ask.’ You’re not weak for asking. You’re strong for caring. 🙏❤️
While the article is commendably thorough, one must acknowledge the epistemological limitations inherent in the current pediatric pharmacovigilance framework. The reliance on weight-based dosing, while statistically pragmatic, fails to account for inter-individual pharmacokinetic variance mediated by genetic polymorphisms in CYP450 enzymes-a factor conspicuously absent from the discussion. One wonders whether the FDA’s current paradigm is sufficiently granular to address the emerging field of pediatric pharmacogenomics. Without integrating genomic stratification into dosing protocols, we risk perpetuating a one-size-fits-all model that, while marginally safer than prior approaches, remains fundamentally inadequate.