Every year, thousands of people end up in hospitals because of medication mistakes-some because they took the wrong dose, others because two pills clashed in their body without anyone noticing. It’s not always a doctor’s error. Often, it’s a gap in communication, a forgotten supplement, or a pill bottle left out in the open. The good news? You don’t have to wait for something to go wrong. You can build a personal medication safety plan with your care team-and it’s simpler than you think.
Start with a complete list of everything you take
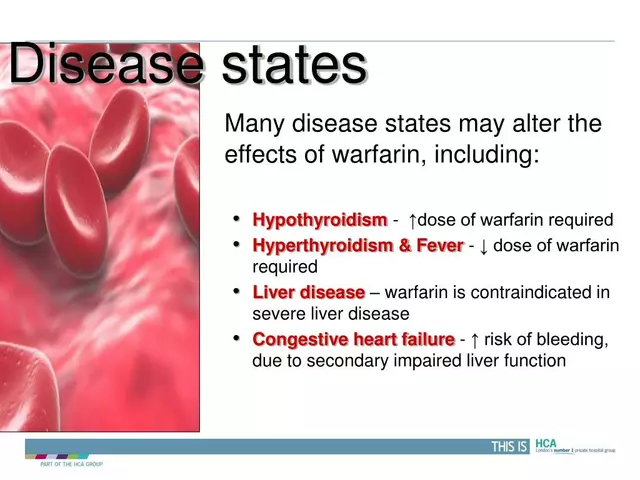
Don’t just list your prescriptions. Include every pill, patch, liquid, or capsule you use. That means over-the-counter painkillers, sleep aids, herbal teas, vitamins, and even supplements like fish oil or turmeric. Many people forget these, but they can cause serious reactions. For example, St. John’s Wort can make blood pressure meds useless. Garlic supplements can thin your blood too much when paired with warfarin. Write it all down. Use a notebook, a phone note, or a printed sheet. Include:- The exact name of the medication (brand and generic if you know it)
- The dose (like 10 mg, 500 mg)
- How often you take it (once daily, twice a day, as needed)
- Why you take it (for high blood pressure, for arthritis pain)
- Who prescribed it (Dr. Lee, your pharmacist, your GP)
- The start date (when you began taking it)
Ask your doctor and pharmacist to review it together
Don’t assume your doctor knows everything on your list. Many patients don’t mention supplements because they think they’re "not real medicine." But your pharmacist does. Ask both to sit down with your list and check for interactions. You can say: "Can you tell me if any of these could react badly with each other?" or "Is there anything here that might make me dizzy or drowsy?" Pharmacists are trained to spot hidden risks. A common mix is NSAIDs (like ibuprofen) with blood pressure pills-it can make the blood pressure meds stop working. Or mixing antidepressants with migraine meds can trigger serotonin syndrome, a dangerous condition. You don’t need to be an expert. Just ask.Store your meds safely-out of sight, out of reach
Medications shouldn’t sit on your bathroom counter, next to your toothpaste, or in a drawer with your socks. Heat, moisture, and easy access increase the risk of mistakes-or worse, accidental overdose. Use a locked cabinet or a small lockbox. This is especially important if you live with kids, teens, or someone with memory issues. One caregiver in Sydney told me her mother kept her heart medication in a jar next to her bed. She confused it with her blood pressure pill and took a double dose. She ended up in the ER. Label every container clearly. If the original bottle is faded or the label is peeling, write the details in big, bold ink: your name, the drug name, the dose, and the time to take it. Use a permanent marker. If you’re unsure, ask your pharmacist to re-label it for you. Most will do it for free.Create a daily routine with a pill organizer
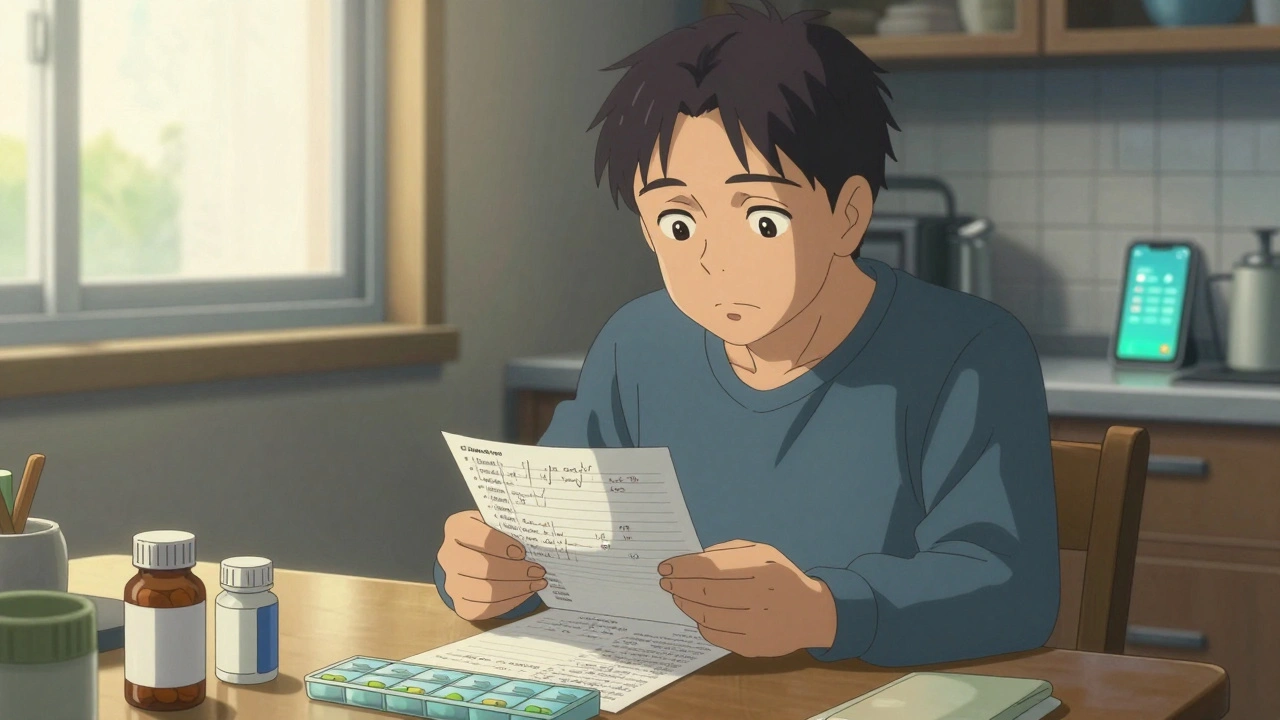
If you take more than three pills a day, a pill organizer isn’t optional-it’s essential. Buy a simple one with compartments for morning, afternoon, evening, and night. Fill it once a week. Set a phone alarm for each dose. Put the organizer next to your toothbrush or coffee maker so you see it daily. For people with memory problems, use simple language. Instead of "take 10 mg of lisinopril once daily," write: "Take this pill for your blood pressure. Do it every morning after brushing your teeth." You can even stick a photo of the pill next to the label. Some people use apps or smart pill dispensers, but studies show the most reliable system is still human routine + visual cues. Don’t overcomplicate it. Consistency matters more than tech.
Know the warning signs of trouble
Medications can cause side effects that look like aging-confusion, dizziness, fatigue, loss of appetite. Don’t brush them off. If you start feeling off after starting a new drug, write it down. Note when it happened, what you were taking, and how you felt. Common red flags:- Sudden dizziness or fainting
- Unexplained bruising or bleeding
- Severe nausea or vomiting
- Swelling in your face, lips, or throat
- Confusion or memory loss that’s new
Plan for emergencies
Keep a printed copy of your medication list in your wallet, purse, or car. Also, leave one with a trusted family member or neighbor. In an emergency, paramedics don’t have time to guess what you’re taking. They need to know fast. If you live alone or have memory issues, consider giving a key to a neighbor or friend so they can access your meds if you can’t answer the door. Some people even give a copy to their local pharmacy-they can flag dangerous interactions before you even pick up a new prescription.Check in regularly with your care team
Medication needs change. Your kidney function slows as you age. A new condition pops up. A drug stops working. You might need less-or more. Schedule a medication review at least once a year. If you’ve had a hospital stay, surgery, or a big change in health, do it sooner. Bring your list. Ask:- Is this still necessary?
- Can any be stopped?
- Are there cheaper or safer options?
- What should I watch for next?
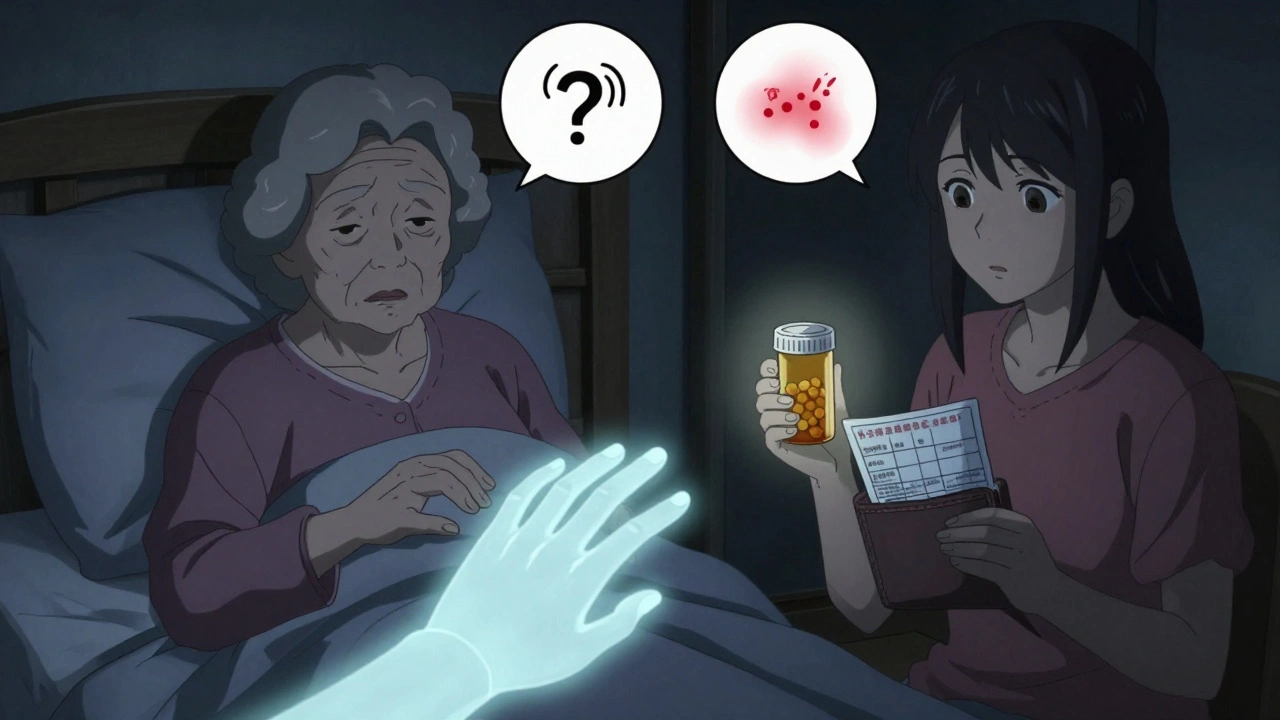
What if you’re helping someone else?
If you’re caring for a parent, partner, or friend with memory loss or chronic illness, your role is even more critical. You’re the bridge between them and the system. Take charge of the list. Fill the pill organizer. Set reminders. Go to appointments with them. Ask questions they’re too shy or confused to ask. Don’t assume they remember what the doctor said. Repeat it back to them in simple terms: "The doctor said take this blue pill after breakfast for your heart. Not before. Not at night. Just after breakfast." And don’t feel guilty about stepping in. Many families wait too long to help-until something goes wrong. Getting involved early saves lives.It’s not about perfection-it’s about awareness
You don’t need to memorize every drug interaction. You don’t need to be a pharmacist. You just need to be the one who asks the questions, writes things down, and speaks up when something feels off. Medication safety isn’t a one-time task. It’s a habit. A daily check. A conversation. A list you keep updated. A pill box you fill. A question you ask at every visit. The system isn’t perfect. But you can make it work for you.What if I forget to take my medication?
If you miss a dose, don’t double up unless your doctor says it’s safe. Most medications have clear instructions for missed doses-check the label or call your pharmacist. If you’re often forgetting, use a pill organizer with alarms, or ask a family member to remind you. Apps like Medisafe or MyTherapy can help, but simple routines often work better for older adults.
Should I stop a medication if I feel side effects?
Never stop a prescription drug suddenly without talking to your doctor. Some medications, like blood pressure pills or antidepressants, can cause serious withdrawal symptoms if stopped cold. Instead, write down what you’re feeling and bring it to your next appointment. Your doctor may adjust the dose or switch you to something safer.
Do I need to tell my doctor about vitamins and supplements?
Yes. Vitamins, herbal teas, and supplements aren’t harmless. They can interfere with prescription drugs. For example, vitamin K can make blood thinners like warfarin less effective. Ginkgo biloba can increase bleeding risk during surgery. Always list them-no matter how "natural" they seem.
How often should I update my medication list?
Update it every time you start, stop, or change a medication-even if it’s temporary. Also review it at least once a year. If you’ve been hospitalized, had surgery, or changed doctors, update it immediately. Keep the most recent version with you at all times.
Can I use a digital app instead of a paper list?
Apps can help, but they’re not foolproof. If you’re in an emergency and your phone is dead, no one can access your list. Always carry a printed copy too. Use apps as a backup, not your only tool. The most reliable system combines digital reminders with a physical list you can hand to a nurse or paramedic.
Next steps: Start today
Here’s what to do right now:- Grab a pen and paper. Write down every medication you take-prescription, over-the-counter, supplements.
- Call your pharmacist or doctor. Ask them to review it with you in your next visit.
- Buy a pill organizer and fill it for the week.
- Find a locked cabinet or box to store all your meds.
- Print two copies of your list. Keep one in your wallet, give one to a trusted person.


THIS. I just got my mom’s meds organized last week after she nearly mixed up her blood thinner with her arthritis pill. I cried. Then I bought a lockbox. Now she has a color-coded pill organizer, alarms on her tablet, and I print her list every time she sees a new doctor. It’s not glamorous, but it’s keeping her alive. 🙌
People act like this is revolutionary, but it’s just basic hygiene for your body. You brush your teeth, you don’t leave your meds next to the toilet like they’re part of the decor. I keep mine in a locked tin under my bed with a sticky note that says ‘DO NOT TOUCH’ in all caps. My cat tried. He learned.
Wow. A whole article about not dying from your own medicine. Who knew? Next up: ‘How to Not Set Your House on Fire With a Toaster.’
i just started using a pill box and its a game changer!! i used to forget if i took my bp pill or not and now i just look at the box and go ‘oh yea i already took it’ lol thanks for the reminder!! 🙏💖
Most of this is common sense, but the real issue is the healthcare system’s complete failure to integrate medication reconciliation into routine care. I’ve had pharmacists refuse to review my list because ‘it’s not in the EHR.’ You’re telling me a 78-year-old woman with 12 meds can’t get a simple review because some software vendor didn’t prioritize interoperability? Pathetic.
they want you to write everything down so they can track you. i dont trust big pharma or the doctors. i take only herbs and apple cider vinegar. the pills are for mind control. also, why do they make you take so many? its the chemicals. they dont want you healthy. they want you addicted. i stopped all meds. still alive. 68. no heart issues. just turmeric and sunshine.
OMG YES!! I’ve been doing this for my dad since his stroke. I even made him a little photo chart with pics of each pill next to the time. He smiles every morning when he sees it. We’re not perfect, but we’re trying. 💕🩷🩵 You’re doing amazing, everyone who’s taking this seriously. You’re saving lives. 🌟
My grandma used to keep all her meds in a cereal box on the counter. I found it when she was in the hospital after mixing her heart med with her sleeping pill. She didn’t even know she took two. Now I fill her organizer every Sunday. She calls me ‘the pill fairy.’ I don’t mind. It’s better than the alternative.
I’m a nurse and I see this every day. People think ‘natural’ means safe. I had a patient take ginkgo biloba before surgery and bled out internally. No one told the surgeon. Just… please, tell your providers everything. Even the tea you drink at 2 a.m. That chamomile? It can thin your blood. We’re not judging. We just want you to live.
Look, I used to think this was overkill. Then my uncle died from a drug interaction nobody checked. He was on statins, ibuprofen, and a supplement called ‘Energy Boost’-which had hidden stimulants. He didn’t even know what was in it. I’m now the family pill police. I carry the list. I ask the questions. I don’t care if I’m annoying. I’d rather be annoying than bury someone.
This isn’t just about safety-it’s about autonomy. When you control your medication narrative, you reclaim agency over your body. The system wants you passive, compliant, forgetful. Writing it down? Asking questions? That’s resistance. That’s dignity. That’s how you survive in a world that treats your health like a transaction.
The advice here is fundamentally sound, but the execution is amateurish. You're recommending a pill organizer without addressing polypharmacy risk stratification or the need for deprescribing protocols. Also, ‘print two copies’? That’s not HIPAA-compliant. You’re creating PHI exposure vectors. A secure digital vault with encrypted QR code access, synced to EHRs via FHIR API, is the only acceptable standard. Everything else is a Band-Aid on a hemorrhage.
so like… i just started taking 7 pills a day and i thought i was doing great until i realized i was taking my blood pressure med at night and my sleep pill in the morning… whoops. now i have a neon pink pill box and i yell ‘PILL TIME!’ like a game show host. my dog now sits by the box. i think he’s proud.
Just did this today. Made a list, bought a box, locked my meds. Felt like a superhero. My mom texted me ‘you’re turning into a pharmacist’ and I said ‘yep, and I’m good at it.’ 💪💊 We’re gonna be okay.
You’re all just doing this because you’re scared. You don’t need lists. You need to stop taking so many pills. Everyone’s on too many drugs. Just quit. Let your body heal itself. You’re not sick. You’re addicted to the system.