Theophylline Drug Interaction Checker
Assess Risk of Theophylline Interactions
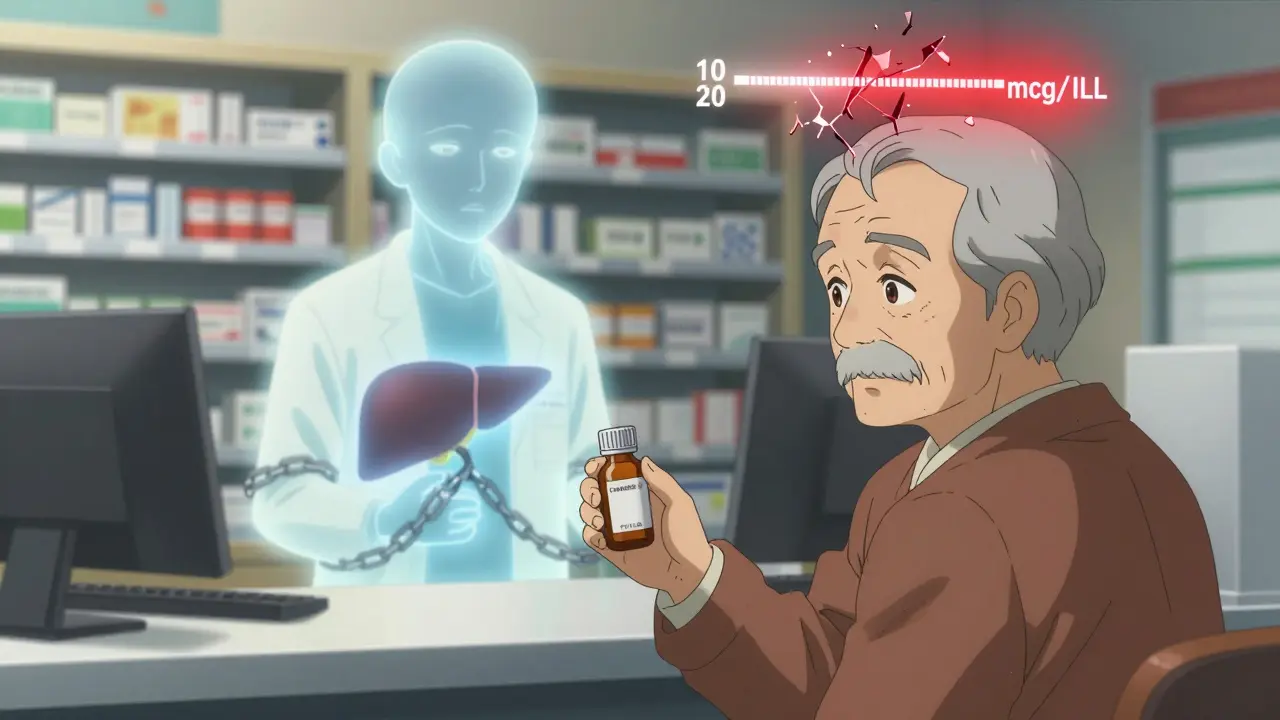
Theophylline has a narrow therapeutic window (10-20 mcg/mL). Some common medications can reduce its clearance by up to 50%, increasing risk of toxicity. This tool helps identify dangerous combinations.
Select Medications
Risk Assessment
Select medications to see interaction risks and recommended actions
Fluvoxamine Interaction
Clearance reduction: 40-50%
Theophylline toxicity risk: 12.7x higher
Recommended action: Avoid combination. If unavoidable, reduce theophylline dose by 50% and monitor levels within 48 hours.
Cimetidine Interaction
Clearance reduction: 25-30%
Toxicity risk: Significant increase (up to 29% of hospital cases)
Recommended action: Reduce theophylline dose by 25-50% before starting cimetidine. Check levels within 48-72 hours.
Allopurinol Interaction
Clearance reduction: 20% (at high dose)
Toxicity risk: 15% of cases linked to allopurinol
Recommended action: Monitor levels closely if taking high-dose allopurinol. Consider dose reduction.
Antibiotic Interaction
Clearance reduction: 15-25%
Toxicity risk: Moderate increase
Recommended action: Monitor levels after starting antibiotics. Consider dose adjustment if needed.
Furosemide Interaction
Clearance reduction: 10-15%
Toxicity risk: Minimal but possible in vulnerable patients
Recommended action: Monitor levels if patient has heart failure or liver disease.
Based on the selected medications, theophylline appears to be safely used without major interaction risks. However, always consult your healthcare provider.
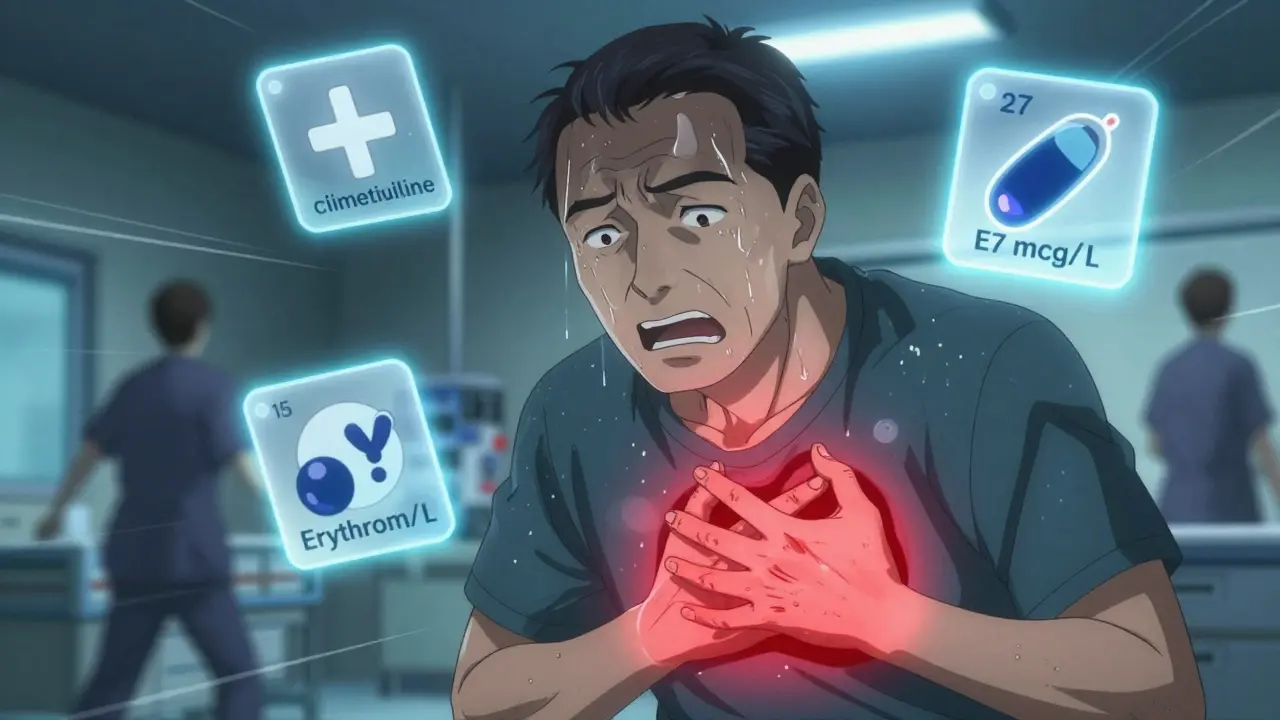
Most people don’t realize that a simple, old-school asthma medication like theophylline can turn deadly if taken with something as common as heartburn medicine or an antibiotic. The problem isn’t the drug itself-it’s how easily other medications can slow down its breakdown in the body. When that happens, theophylline builds up to toxic levels, and patients can end up in the emergency room with nausea, rapid heartbeat, or even seizures. This isn’t rare. In the U.S. alone, about 2,000 emergency visits each year are tied to theophylline toxicity, and more than a third of those cases come from drug interactions that reduce clearance.
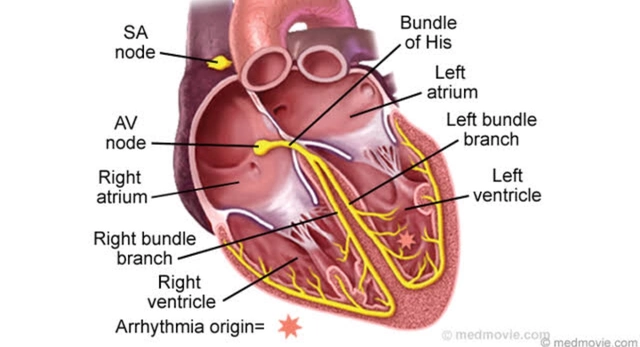
Why theophylline is so sensitive to other drugs
Theophylline has been around since the 1920s. It’s not flashy, it’s not new, and it’s not the first choice for most doctors anymore. But it’s still used-especially in places where newer inhalers are too expensive or hard to get. The trouble is, theophylline has a razor-thin safety margin. The difference between a helpful dose and a dangerous one is small: 10 to 20 micrograms per milliliter in the blood. Go over that, and you risk serious side effects. Go under, and the drug doesn’t work.What makes it so tricky is how the body handles it. About 90% of theophylline is broken down in the liver by an enzyme called CYP1A2. This enzyme is like a gatekeeper. If something blocks it, theophylline can’t leave the body fast enough. Even a 15% drop in clearance can push someone from a safe level to a toxic one-especially if they’re already near the top of the therapeutic range.
And here’s the kicker: theophylline doesn’t clear the body in a straight line. At therapeutic doses, its metabolism becomes nonlinear. That means a small increase in drug levels can cause a huge spike in concentration. A 20% reduction in clearance doesn’t mean a 20% rise in blood levels-it could mean a 40% or 50% rise. That’s why even minor interactions can be dangerous.
Medications that slow down theophylline clearance
Not all drugs affect theophylline the same way. Some are silent killers. Others are well-known red flags. Here are the biggest offenders, backed by clinical data:
- Fluvoxamine (an antidepressant): This SSRI is one of the strongest CYP1A2 inhibitors out there. It can slash theophylline clearance by 40-50%. The European Respiratory Society says to avoid combining them entirely. If a patient is on fluvoxamine and starts theophylline, they’re at a 12.7-times higher risk of toxicity.
- Cimetidine (Tagamet, for heartburn): Once a staple for acid reflux, cimetidine reduces theophylline clearance by 25-30%. A 2021 study found it was involved in nearly 29% of theophylline toxicity cases in hospitals. Patients on stable doses have been known to go from 15 mcg/mL to over 24 mcg/mL within just 72 hours after starting cimetidine.
- Allopurinol (for gout): Many assume this is harmless, but high doses (600 mg daily) cut theophylline clearance by about 20%. Lower doses (300 mg) don’t have the same effect, but doctors often don’t know that. In one survey, 15% of toxicity cases were linked to allopurinol.
- Erythromycin and clarithromycin (antibiotics): These macrolides don’t directly block CYP1A2, but they interfere with CYP3A4, which plays a backup role in theophylline metabolism. Clearance drops by 15-25%. A patient on theophylline who gets pneumonia and is prescribed clarithromycin might not realize they’re walking into a risk zone.
- Furosemide (water pill): Evidence is mixed, but some studies show it can reduce clearance by 10-15%. If a patient has heart failure and is on both drugs, this could be the tipping point.
On the flip side, some drugs speed up clearance-like rifampicin, phenytoin, and phenobarbital. But those are less common in daily practice. The real danger lies in the quiet, everyday meds that patients take without thinking.
Who’s most at risk?
It’s not just about the drugs. The patient’s body matters too. Elderly patients with heart failure or liver disease clear theophylline slower to begin with. Smokers? They clear it faster-CYP1A2 gets turned on by cigarette smoke. But if they quit smoking while on theophylline, their clearance can drop by 30-50% in just two weeks. That’s a double whammy: they’re losing a natural metabolic boost while possibly starting a new medication that further slows breakdown.
And here’s the overlooked group: patients in low-resource settings. Theophylline is still used in 12% of COPD cases in Africa and 8% in Asia, compared to under 2% in North America. In these areas, patients often see multiple providers, get prescriptions from pharmacies without full records, and don’t have access to regular blood tests. A patient might get cimetidine from a local clinic, start it with their theophylline, and never get a follow-up. No one checks their levels. No one connects the dots.
A 2021 study of 1,247 patients over 65 found that 28% were on at least one drug that reduced theophylline clearance-and only 37% had their dose adjusted. That’s a massive gap between knowing the risk and acting on it.
What doctors and pharmacists should do
There’s no excuse for missing these interactions. The data is clear. The guidelines exist. The tools are available.
When a patient is on theophylline:
- Always check their full medication list-prescription, OTC, and supplements. Even antacids can interfere.
- If starting a new drug, assume it might affect theophylline until proven otherwise.
- For strong inhibitors like fluvoxamine or cimetidine, reduce the theophylline dose by 25-50% before starting the new drug.
- Check serum levels within 48-72 hours after adding or removing an interacting drug.
- Never assume the patient knows what they’re taking. Many take cimetidine over the counter for “indigestion” and never tell their doctor.
The University of Michigan’s 2023 guidelines say it plainly: When in doubt, check the level. That’s the golden rule.
What patients need to know
If you’re taking theophylline, here’s what you need to do:
- Keep a written list of every medication you take-including vitamins, herbal products, and painkillers.
- Ask your pharmacist: “Could this new medicine interfere with my theophylline?”
- Know the signs of toxicity: nausea, vomiting, fast heartbeat, tremors, confusion, or trouble sleeping. If you feel worse after starting a new drug, get your levels checked.
- Don’t stop smoking suddenly without telling your doctor. That alone can raise your theophylline levels dangerously.
- If you’re on allopurinol for gout, make sure your doctor knows you’re on theophylline. Don’t assume it’s safe just because it’s for a different condition.
One patient in Sydney, Australia, was on theophylline for COPD for five years. She started taking cimetidine for heartburn after a friend recommended it. Three days later, she was vomiting and her heart was racing. Her serum level was 27.3 mcg/mL-well into the toxic range. She didn’t know the two could interact. She didn’t think to ask.

Why this still matters today
Theophylline use has dropped by 62% in the U.S. since 2000. But that doesn’t mean the risk is gone. In fact, it’s growing. The remaining patients are often older, sicker, and on more medications. The FDA reported a 5.3% yearly increase in interaction-related adverse events from 2021 to 2022-even as overall use declined.
Why? Because the people still taking it are the ones most vulnerable. They’re the ones with multiple chronic conditions. They’re the ones with limited access to specialists. They’re the ones whose prescriptions come from different doctors, different pharmacies, different systems.
And here’s the sad truth: most electronic health records still don’t flag theophylline interactions well. A 2023 survey of 412 pulmonologists found that 62% said their systems didn’t give strong enough alerts. That means human judgment is still the last line of defense.
Bottom line
Theophylline isn’t going away. Not yet. It’s still used in millions of people worldwide. But it’s a drug that demands respect. A small mistake in prescribing or taking other meds can turn it from a lifesaver into a silent killer.
There’s no magic solution. No app, no AI, no automated alert can replace a clinician who asks the right questions. But if you’re a patient, a pharmacist, or a doctor-know this: if you’re on theophylline, check every new medication. Ask about interactions. Don’t assume it’s safe. And if you’re unsure, check the blood level. It’s the only way to be sure.
Can I take ibuprofen with theophylline?
Yes, ibuprofen does not significantly affect theophylline metabolism. Unlike cimetidine or fluvoxamine, it doesn’t inhibit CYP1A2. However, if you’re taking high doses of ibuprofen long-term or have kidney issues, your doctor may still want to monitor your theophylline levels as a precaution. Always inform your provider about all medications you’re using.
What happens if I stop smoking while on theophylline?
Stopping smoking can reduce theophylline clearance by 30-50% within two weeks because your liver stops producing extra CYP1A2 enzyme. This can cause theophylline levels to rise dangerously-even if your dose hasn’t changed. Always tell your doctor if you quit smoking. They’ll likely lower your dose and check your blood level within a week.
Is theophylline still prescribed today?
Yes, but less often. It’s mainly used for severe asthma or COPD when newer inhalers don’t work, or in areas where they’re too expensive. Globally, it’s still part of maintenance therapy for 3.2% of COPD patients, with higher use in Asia and Africa. In North America, it’s used in under 2% of cases. Its role is shrinking, but it’s not obsolete.
How often should theophylline levels be checked?
When starting theophylline, levels should be checked after 3-5 days. After that, check every 6-12 months if stable. But if you start or stop any new medication-especially antibiotics, antidepressants, or heartburn drugs-check your level within 48-72 hours. The same goes for quitting smoking or developing liver or heart problems.
Can herbal supplements affect theophylline?
Yes. St. John’s wort can increase theophylline clearance, lowering its effectiveness. Other herbs like echinacea or black cohosh may inhibit CYP enzymes, though data is limited. Always tell your doctor about any supplements you take. Many patients don’t realize herbs can interact with prescription drugs.



This is wild. I took Tagamet for years and never knew it could kill you if you're on theophylline. My grandpa almost died and no one told him. How is this not on every prescription label??
It’s not just about the drug-it’s about how we treat medicine like a vending machine. You grab a pill for heartburn, you grab a pill for asthma, you grab a pill for gout… and somehow we think the body’s gonna sort it out. But the liver? It’s not a traffic cop. It’s a janitor trying to clean up a hurricane. Theophylline’s like a glass of water on a tightrope. One gust-and it’s gone. We need to stop pretending biology is optional.
Wow. This is such an important post. I’m a pharmacist in Ohio, and I’ve seen this exact scenario-elderly patient, on theophylline, starts cimetidine for ‘just a little heartburn,’ no follow-up. We have to do better. Even simple meds can be silent killers. I now always ask: ‘Are you on theophylline?’ before dispensing anything. It’s saved lives. 🙏
OMG I just realized my mom is on ALL of these!! Theophylline + cimetidine + allopurinol 😱 I’m calling her right now. She thinks ‘natural’ means safe-st. john’s wort, ginkgo, garlic pills… she’s a walking drug cocktail! Thanks for the wake-up call!! 💊🩺🔥
In India, we still use theophylline because salbutamol inhalers cost more than a week’s groceries. We don’t have EHRs, we don’t have pharmacists in every clinic, and patients get meds from five different shops. This isn’t a ‘medical error’-it’s a systemic failure. The real toxicity here isn’t the drug-it’s the inequality. Someone in Delhi doesn’t get a 48-hour lab check. They get a prayer and a hope.
Let’s talk about the elephant in the room: we treat patients like machines with input/output models. But the human body? It’s a symphony. One wrong note-CYP1A2 gets muffled-and the whole thing collapses. Fluvoxamine doesn’t just ‘interfere’-it drowns the enzyme. And we wonder why people crash. We need to stop prescribing like we’re coding a spreadsheet. This isn’t math. It’s biology with consequences.
Okay, but let’s be real-how many of these ‘toxic’ interactions are just pharmaceutical fear-mongering? I mean, if you’re on theophylline and you take cimetidine, sure, maybe your levels go up-but how many people actually die? Like, 2,000 ER visits a year? That’s 0.0006% of the U.S. population. Meanwhile, people are dying from opioids, statins, and antidepressants every single day. Why is this getting a whole essay? Is it because it’s an old drug? Because it’s cheap? Because it doesn’t make Big Pharma money? Someone’s got an agenda here.
So let me get this straight… we’re still using a 1920s drug that’s basically a chemical landmine, because it’s cheaper than inhalers? And now we’re gonna blame patients for not knowing their meds? 😂 Meanwhile, doctors still write scripts like they’re texting their ex. ‘Take one, call me if you die.’ The real toxicity isn’t theophylline-it’s the medical system’s laziness. Check levels? Nah. Just hope the patient doesn’t Google it.
Incorrect. Theophylline clearance is primarily mediated by CYP1A2, not CYP3A4. Clarithromycin’s effect is indirect via CYP3A4 inhibition, which is minor compared to direct CYP1A2 inhibitors. Also, furosemide has no clinically significant interaction per FDA labeling. This post is riddled with overinterpretation and anecdotal data. The 2,000 ER visits? Likely inflated by poor coding. Evidence-based medicine requires precision-not fear-based generalizations.