For people with severe asthma who still struggle to breathe despite using high-dose inhalers, standard treatments often feel like fighting a fire with a squirt gun. That’s where biologics come in - not as magic bullets, but as precise tools that target the exact inflammation driving their asthma. Two of the most established classes are anti-IgE and anti-IL-5 therapies, each designed for different types of severe asthma. These aren’t new, but they’re still misunderstood. Many patients don’t know if they’re candidates, how long it takes to work, or why one drug might help them while another doesn’t.
What Makes a Biologic Different?
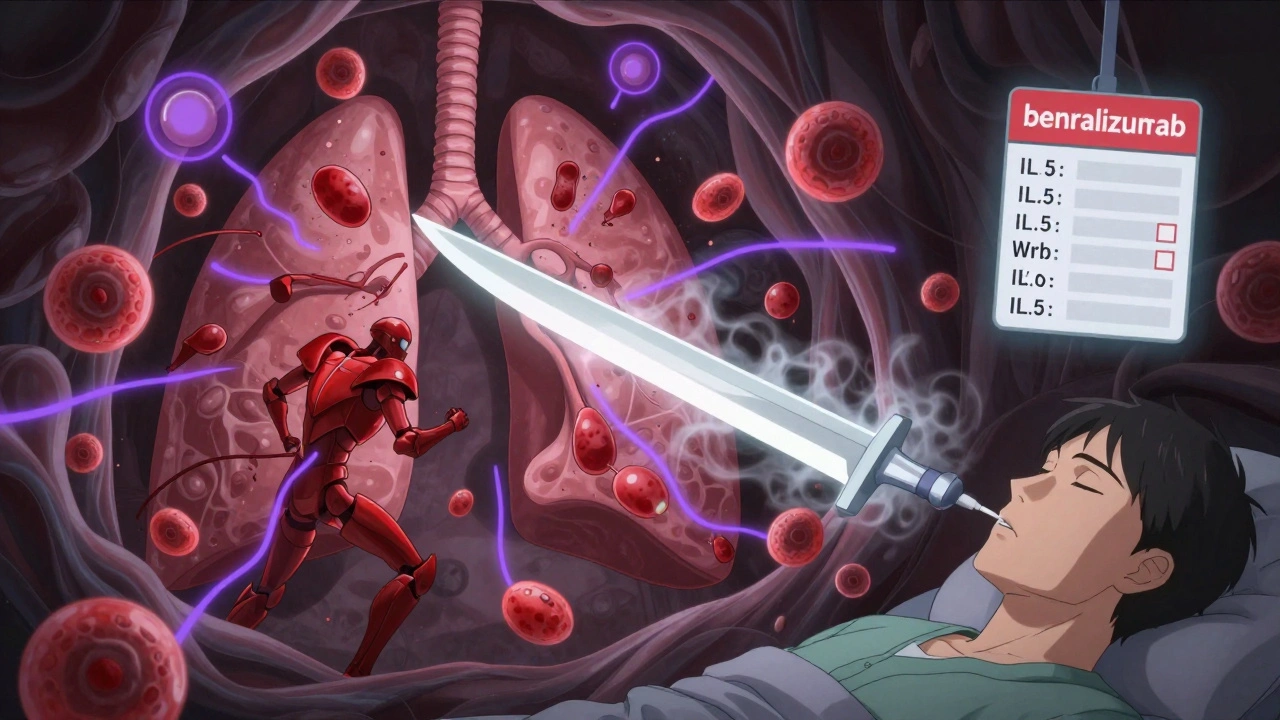
Unlike inhalers that open airways or steroids that broadly suppress inflammation, biologics are lab-made antibodies. They’re designed to lock onto one specific molecule in your immune system and shut it down. Think of them like sniper rifles instead of shotguns. Omalizumab (Xolair) targets IgE, the antibody that triggers allergic reactions. Mepolizumab (Nucala), reslizumab (Cinqair), and benralizumab (Fasenra) all block IL-5, a chemical that tells eosinophils - a type of white blood cell - to swarm the lungs and cause swelling. These drugs don’t cure asthma. They don’t replace your inhalers. But for the right person, they can cut flare-ups in half.
Anti-IgE: For Allergic Asthma
Omalizumab was the first biologic approved for asthma back in 2003, and it’s still used today. It works by binding to IgE before it can attach to mast cells and basophils. When IgE can’t trigger those cells, they don’t release histamine, leukotrienes, or other chemicals that cause wheezing, coughing, and tightness in the chest. This makes omalizumab ideal for people whose asthma flares up with pollen, dust mites, or pet dander. You need to have a positive allergy test and a total IgE level between 30 and 1500 IU/mL to qualify. It’s given as a shot under the skin every 2 to 4 weeks, based on your weight and IgE level. Most people start feeling better after 12 to 16 weeks, though some notice small improvements as early as 4 weeks. In clinical trials, patients on omalizumab had about a 50% drop in severe asthma attacks. But if your asthma isn’t allergic - if you don’t react to common allergens - this drug won’t help. And it doesn’t work during an active attack. It’s a preventive tool, not an emergency fix.
Anti-IL-5: For Eosinophilic Asthma
If your asthma is driven by too many eosinophils in your blood or lungs, anti-IL-5 drugs are the go-to. These include mepolizumab, reslizumab, and benralizumab. They all target IL-5, but in slightly different ways. Mepolizumab and reslizumab bind directly to IL-5, stopping it from activating eosinophils. Benralizumab goes one step further - it attaches to the IL-5 receptor on eosinophils and signals your immune system to destroy them outright. This means benralizumab can drop eosinophil counts to nearly zero within a day. That’s faster than the others. All three require blood tests to confirm you have at least 150-300 eosinophils per microliter in the past year. Mepolizumab and benralizumab are injected under the skin every 4 weeks (benralizumab switches to every 8 weeks after three doses). Reslizumab is given as an IV infusion every 4 weeks, which means you have to go to a clinic. In the MENSA trial, mepolizumab reduced exacerbations by 52%. Benralizumab’s ZONDA trial showed a 51% drop. These aren’t small gains. For someone who used to end up in the ER four times a year, that means zero visits.
How Do They Compare?
| Feature | Anti-IgE (Omalizumab) | Anti-IL-5 (Mepolizumab, Benralizumab, Reslizumab) |
|---|---|---|
| Target | IgE antibody | IL-5 or IL-5 receptor |
| Best For | Allergic asthma with confirmed allergens | Eosinophilic asthma (high blood eosinophils) |
| Required Test | Serum IgE level, allergy skin test | Blood eosinophil count ≥150-300/μL |
| Dosing | Every 2-4 weeks, subcutaneous | Every 4 weeks (subcutaneous) or every 4 weeks IV (reslizumab) |
| Onset of Effect | 4-16 weeks | 4-12 weeks (benralizumab acts fastest on eosinophils) |
| Reduction in Exacerbations | ~50% | 51-52% |
| Oral Steroid Reduction | Up to 50% | Up to 60% |
The big difference? Anti-IgE works best if your asthma is tied to allergies. Anti-IL-5 works if your asthma is tied to high eosinophils - even if you’re not allergic. Some people have both, and that’s when things get complicated. Doctors now use tools like fractional exhaled nitric oxide (FeNO) and blood tests to figure out which pathway is dominant. If you’re allergic and have high eosinophils, you might be eligible for both, but you can’t take them together. You have to pick one.
What to Expect When You Start
Starting a biologic isn’t like switching inhalers. It’s a commitment. You’ll need to get blood tests before you begin, and often again after 3-6 months. Insurance approval can take 2 to 3 weeks. Many patients hit roadblocks here. Even if your doctor prescribes it, the pharmacy might say no until you prove you’ve tried everything else. That means documenting your inhaler use, showing you’ve been to asthma education classes, and proving you’re not just skipping doses. Once you’re approved, you’ll get training on how to inject yourself. Most people get comfortable after two or three tries. Side effects are usually mild - redness or soreness at the injection site, headache, or sore throat. About 1 in 10 people get these. Anaphylaxis is rare - about 1 in 1,000 doses - but it’s why you’re asked to wait 30 minutes after your first injection. If you’ve had severe allergic reactions before, your risk is higher. Some patients report joint pain or fatigue after starting benralizumab, and a few have had to stop. It’s not common, but it happens.
Real Results, Real Stories
People who respond well often describe it as life-changing. One Reddit user, u/AsthmaWarrior2020, said after six months on mepolizumab, they went from three to four ER visits a year to zero. They also cut their daily prednisone from 10mg to occasional bursts. Another patient, u/BreathlessInSeattle, tried benralizumab and saw their asthma improve - but developed severe joint pain after three shots and had to quit. That’s the trade-off. Not everyone benefits. Studies show 30-40% of patients don’t respond at all. That’s why biomarkers matter. If your eosinophils are low and your IgE is normal, you’re unlikely to benefit from either class. And if you stop your inhalers because you feel better? That’s a mistake. Biologics are add-ons, not replacements. You still need your controller and rescue inhalers. The Global Initiative for Asthma (GINA) says this clearly: biologics are only for people who’ve already optimized everything else.
Cost and Access
These drugs aren’t cheap. Annual costs range from $25,000 to $40,000 USD. In Australia, Medicare covers them under the Pharmaceutical Benefits Scheme (PBS) for eligible patients, but strict criteria apply. You need to be referred by a respiratory specialist or allergist, and you must meet the biomarker thresholds. Even then, you might pay a co-payment. In the U.S., most insurers require prior authorization and step therapy - meaning you have to try cheaper drugs first. Some manufacturers offer co-pay cards that reduce out-of-pocket costs to under $5 a month. But if you’re uninsured or underinsured, access is a real barrier. Globally, only 1-2% of eligible patients are on biologics. The reason? Cost, complexity, and lack of awareness. Even doctors sometimes miss the signs of eosinophilic asthma.
What’s Next?
The field is moving fast. Tezepelumab (Tezspire), approved in 2021, targets TSLP - an earlier trigger in the inflammation chain. It works even if your eosinophils are low, making it the first biologic that doesn’t require a specific biomarker. It’s promising, but it’s even more expensive. Trials are underway for biologics that only need to be injected twice a year. That could change everything for people who struggle with frequent clinic visits. For now, the best advice is simple: if you’re still struggling with asthma despite your current meds, talk to your specialist. Get tested for IgE and eosinophils. Don’t assume you’re not a candidate. These drugs aren’t for everyone - but for the right person, they can mean the difference between constant flares and a normal life.
Can I stop my inhalers if I start a biologic?
No. Biologics are add-on therapies. You must continue using your inhaled corticosteroids and rescue inhalers as prescribed. Stopping them can lead to dangerous flare-ups, even if you feel better. Biologics reduce inflammation over time, but they don’t provide immediate relief like a rescue inhaler.
How long does it take to see results from anti-IgE or anti-IL-5 biologics?
Most people notice improvements in asthma control within 4 to 12 weeks, but full benefits can take up to 16 weeks. Some patients report fewer nighttime symptoms or less reliance on rescue inhalers earlier. Don’t give up if you don’t feel better right away - these drugs work slowly by changing underlying inflammation, not by opening airways immediately.
Are biologics safe for children?
Yes, omalizumab is approved for children as young as 6 years old with severe allergic asthma. Anti-IL-5 biologics like mepolizumab and benralizumab are approved for children 6 and older as well, but only for eosinophilic asthma. Reslizumab is only approved for adults 18 and older. Pediatric use requires close monitoring by a specialist.
What if I don’t respond to the first biologic I try?
It’s not uncommon. About 30-40% of patients don’t respond to their first biologic. If that happens, your doctor may switch you to another class - for example, from an anti-IgE to an anti-IL-5 drug, or vice versa - based on your biomarkers. Some patients respond better to one mechanism than another. Switching is safe and often effective.
Do I need to get blood tests every time I get a shot?
No. Blood tests for IgE or eosinophils are only needed before starting and occasionally during treatment - usually every 6 to 12 months. Your doctor will let you know if repeat testing is needed. If your asthma stays stable and your symptoms improve, frequent testing isn’t required.





This is sooo true 😭 I was on Xolair for 8 months and still ended up in the ER twice. Like... what's the point if it doesn't even work? 😑
Anyone else notice how these drugs are basically just fancy placebos with a $40k price tag? 🤔 The real fix is cleaning your air, not injecting antibodies. Big Pharma doesn't want you to know that.
I’ve been on benralizumab for a year now. My ER visits dropped from 5/year to zero. I still use my inhalers-don’t stop them-but I can finally sleep through the night. It’s not magic, but it’s life-changing for people who’ve tried everything else. Don’t give up if the first one doesn’t click.
They’re tracking your eosinophils but not your soul. Who’s really controlling the data? The FDA? The insurance bots? Or just the algorithm that decided you’re worth $25k to keep alive?
Y’all need to stop giving up after one try. I switched from omalizumab to mepolizumab after 6 months and my lungs finally stopped screaming. It’s not instant. It’s not easy. But if you’ve got the biomarkers? It’s worth fighting for. Keep pushing your doc. 💪
It is not merely a medical issue but a metaphysical one: the body as a battlefield of molecular signals, and we, the unwitting soldiers, are told to pay for our own liberation. The true enemy is not IgE-it is the commodification of healing.
So we spend 40k a year to get back to where a 1990s inhaler could’ve taken us? Cool. I’m just glad my dog doesn’t need a prescription to breathe.
You think this is about asthma? It’s about control. Who gets to decide who gets access? Who gets to say your inflammation is ‘severe enough’? This isn’t medicine-it’s gatekeeping with a syringe.
Hey I just started mepolizumab last month and already my nighttime cough is gone 🥹 I know it takes time but you’re not alone. Keep going. You got this. 💕
One must consider the ontological implications of antibody-based therapeutics. If we are reducing inflammation through exogenous immunoglobulins, are we not altering the very essence of our immunological identity? The self becomes a vessel for corporate biologics.
They say you need 150 eosinophils to qualify but what if your numbers are low because the lab messed up? Or because they’re lying to get you off the drug? I’ve seen it happen. This whole system is rigged.
As a physician practicing in rural India, I have witnessed patients travel over 300 kilometers for biologic access. The cost is prohibitive, the infrastructure is lacking, yet the clinical benefit, when available, is undeniable. This is not a luxury-it is a necessity, and its inequity is a moral failure.
Wow. So after all this, the answer is… just keep taking your inhalers? And pay $40k? And hope you’re in the 60% who respond? That’s it? That’s the whole thing? I feel like I just watched a 10,000-word ad for Big Pharma.