Medication Safety Plan: What It Is and How It Saves Lives
When you take more than one medication, a medication safety plan, a personalized strategy to prevent harmful drug interactions, side effects, and storage errors. Also known as a drug management plan, it’s not just for seniors or people with chronic illness—it’s for anyone who takes pills, injections, or eye drops regularly. Think of it like a checklist you build with your pharmacist, doctor, or even yourself. It answers simple but critical questions: Are these drugs safe together? Is my insulin still good after being left in the car? Did I forget to tell my doctor I’m taking that herbal supplement?
The real power of a medication safety plan, a personalized strategy to prevent harmful drug interactions, side effects, and storage errors. Also known as a drug management plan, it’s not just for seniors or people with chronic illness—it’s for anyone who takes pills, injections, or eye drops regularly. comes from connecting it to other key health practices. For example, knowing how drug interactions, when two or more medications affect each other’s absorption, metabolism, or effect in the body. Also known as medication interactions, they can turn a safe treatment into a life-threatening situation. works helps you spot red flags—like mixing statins with grapefruit juice or taking PPIs with antifungals. Then there’s generic drug safety, the misconception that generic medications are less effective or riskier than brand-name drugs, despite FDA-equivalent standards. Also known as generic medication trust, this fear leads people to skip doses or pay more than they need to. And let’s not forget pharmacy consultation, a free service where pharmacists review your full list of meds to catch hidden risks and suggest cheaper alternatives. Also known as medication review, this is often overlooked but one of the most underused tools in healthcare. Most people don’t realize their pharmacist can spot a dangerous combo between their heart pill and their new supplement—before it hurts them.
A good medication safety plan doesn’t just list what you take. It tracks where you store it (heat and humidity destroy pills faster than you think), when you take it (missing a dose or doubling up can be deadly), and what to do if something goes wrong (itching after opioids? Nausea from GLP-1 drugs? Know the signs). It’s not about memorizing every side effect. It’s about having a simple system: keep a current list, ask your pharmacist every time you pick up a new prescription, and never assume a drug is safe just because it’s over-the-counter. The posts below show real cases—how humidity ruins insulin, how citrus fruits interfere with blood pressure meds, how counterfeit pills contain fentanyl, and how a 5-minute chat with your pharmacist prevented a hospital visit. These aren’t theoretical risks. They’re daily realities. And you don’t need a medical degree to protect yourself. Just a plan, and the willingness to ask questions.
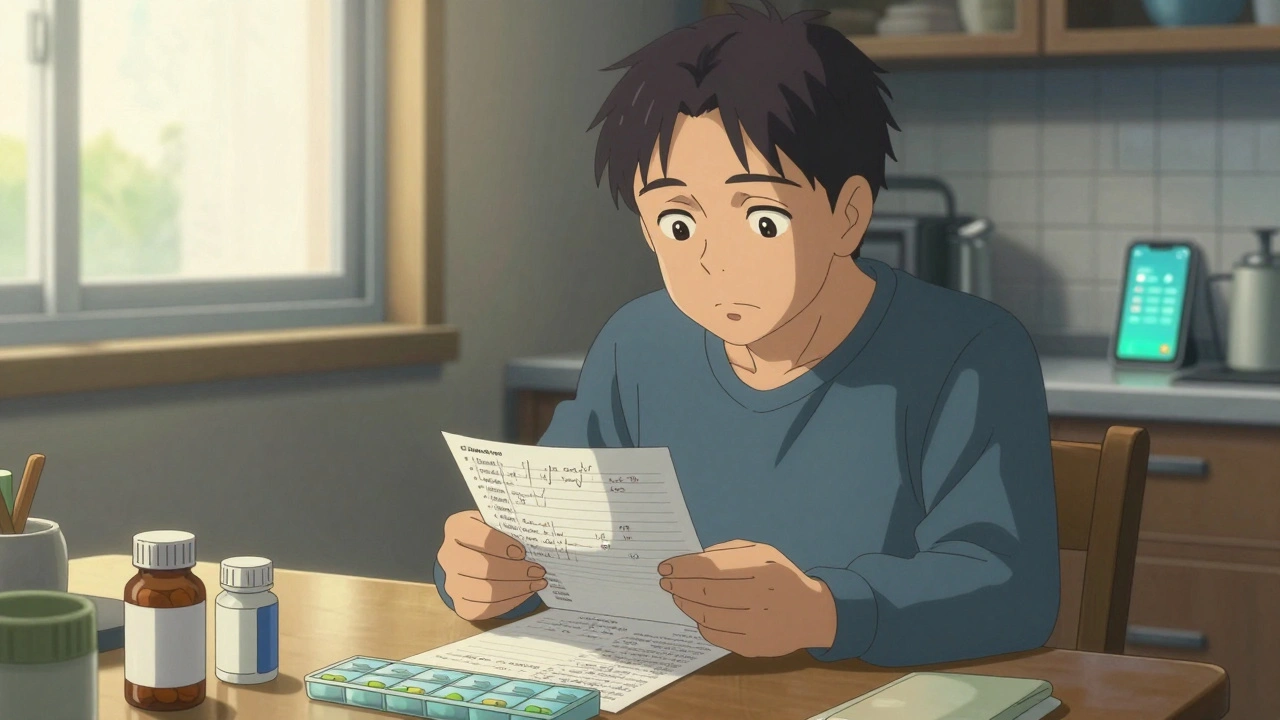
How to Build a Personal Medication Safety Plan with Your Care Team
Build a personal medication safety plan with your care team to prevent dangerous drug interactions, reduce side effects, and avoid hospital visits. Start with a full list of all medications, store them safely, use a pill organizer, and check in regularly.