AS Treatment: What You Need to Know About Medications, Side Effects, and Alternatives
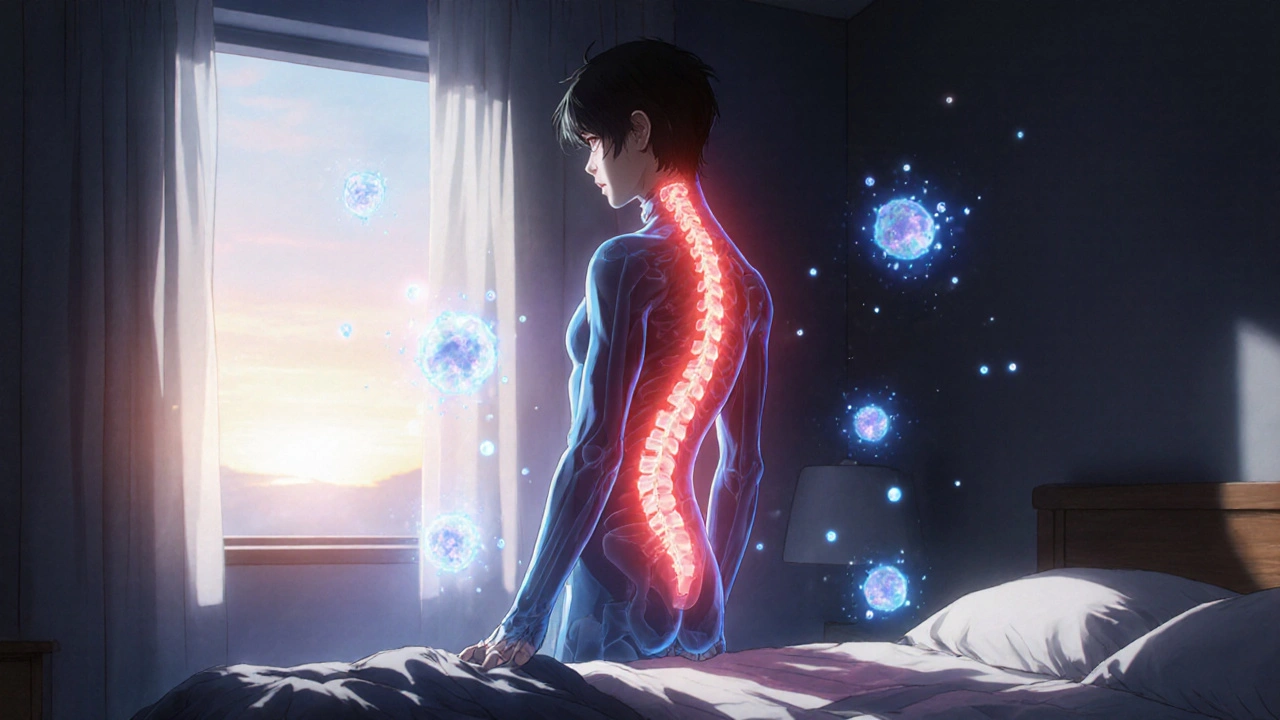
When you’re dealing with AS treatment, the medical approach to managing ankylosing spondylitis, a chronic inflammatory arthritis that primarily affects the spine. Also known as ankylosing spondylitis management, it’s not just about pain relief—it’s about keeping you moving, reducing long-term damage, and avoiding the side effects that come with long-term drug use. Many people assume AS treatment means popping NSAIDs every day and calling it quits. But that’s only the start. The real game changes when you factor in biologics, physical therapy, and how your gut health might be quietly influencing your inflammation levels.
One of the biggest blind spots in AS treatment is the overreliance on NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen, often the first-line option for reducing pain and stiffness. They work—for a while. But long-term use can wreck your stomach, kidneys, and even raise your risk of heart problems. Then there are DMARDs, disease-modifying antirheumatic drugs like sulfasalazine, sometimes used when NSAIDs aren’t enough. They’re slower, less reliable for spinal symptoms, and come with their own list of risks. And then you get to biologics, targeted drugs like adalimumab or etanercept that block specific immune signals driving inflammation. These can be game-changers—but they’re expensive, require injections, and can leave you more vulnerable to infections. Not everyone responds. Not everyone can afford them. And too many doctors skip the basics—like movement, posture, and sleep—before jumping to biologics.
What you won’t find in most brochures? How AS treatment connects to your diet, your stress levels, and even your breathing. People with AS often develop restricted chest expansion over time, making deep breathing harder. That’s where physical therapy isn’t optional—it’s survival. Scar tissue builds up in the spine and joints. Without daily movement, you’re not just losing flexibility—you’re losing independence. And while some turn to supplements like turmeric or omega-3s, the evidence is thin. What works? Consistent exercise. Proper sleep. Monitoring for eye inflammation (uveitis). Knowing when your pain isn’t just stiffness—it’s a flare that needs a different strategy.
Below, you’ll find real-world guides from people who’ve been through the AS treatment maze. You’ll see how some switched from one biologic to another after side effects hit. How others managed to reduce their NSAID use by adjusting their routine. How one person reversed years of stiffness with daily yoga and breathing drills. You’ll also find warnings about drug interactions—like how some AS meds can mess with your liver enzymes or trigger yeast infections when paired with antibiotics. This isn’t theory. It’s what works, what backfires, and what no one tells you until it’s too late.
Ankylosing Spondylitis: How TNF Inhibitors Reduce Spine Inflammation and Improve Daily Life
Ankylosing spondylitis causes chronic spine inflammation and stiffness. TNF inhibitors like Humira and Enbrel target the root cause, reducing pain, slowing bone fusion, and improving mobility for most patients. Learn how they work and who benefits most.