What Is Ankylosing Spondylitis?
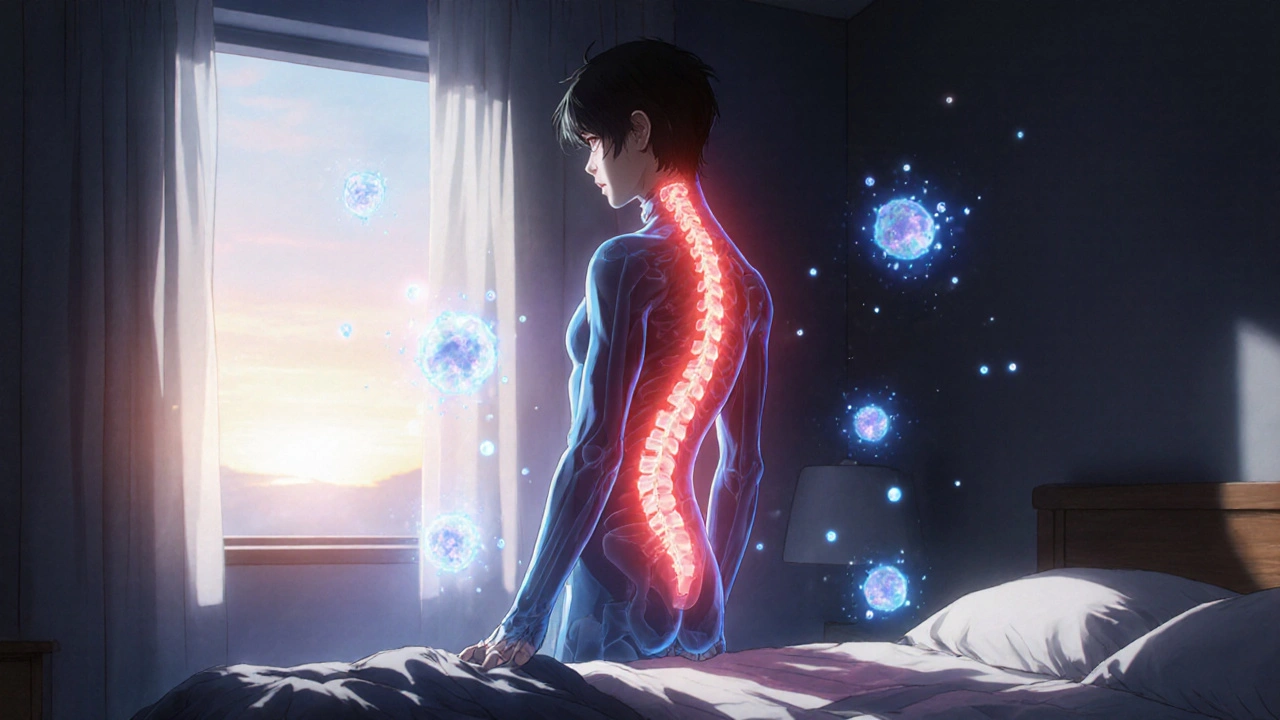
Ankylosing spondylitis (AS) isn’t just back pain. It’s a chronic autoimmune disease that attacks the spine and sacroiliac joints, causing inflammation so severe it can fuse bones together over time. Unlike regular back pain from strain or injury, AS pain is worse in the morning and improves with movement. Stiffness can last for hours, not minutes. People often describe it as feeling like their spine is locked in place.
This disease doesn’t just affect the spine. It can also inflame tendons where they attach to bone - called entheses - leading to pain in the heels, hips, and even ribs. In advanced cases, the spine can become rigid, making it hard to bend, twist, or even look up. It usually starts in early adulthood, with men being more commonly affected than women. About 1 in 200 people have it, and if you carry the HLA-B27 gene, your risk jumps significantly.
Doctors used to think AS was just a slow, inevitable decline. But that changed with the arrival of targeted treatments. Today, the goal isn’t just to manage pain - it’s to stop the disease from destroying your spine.
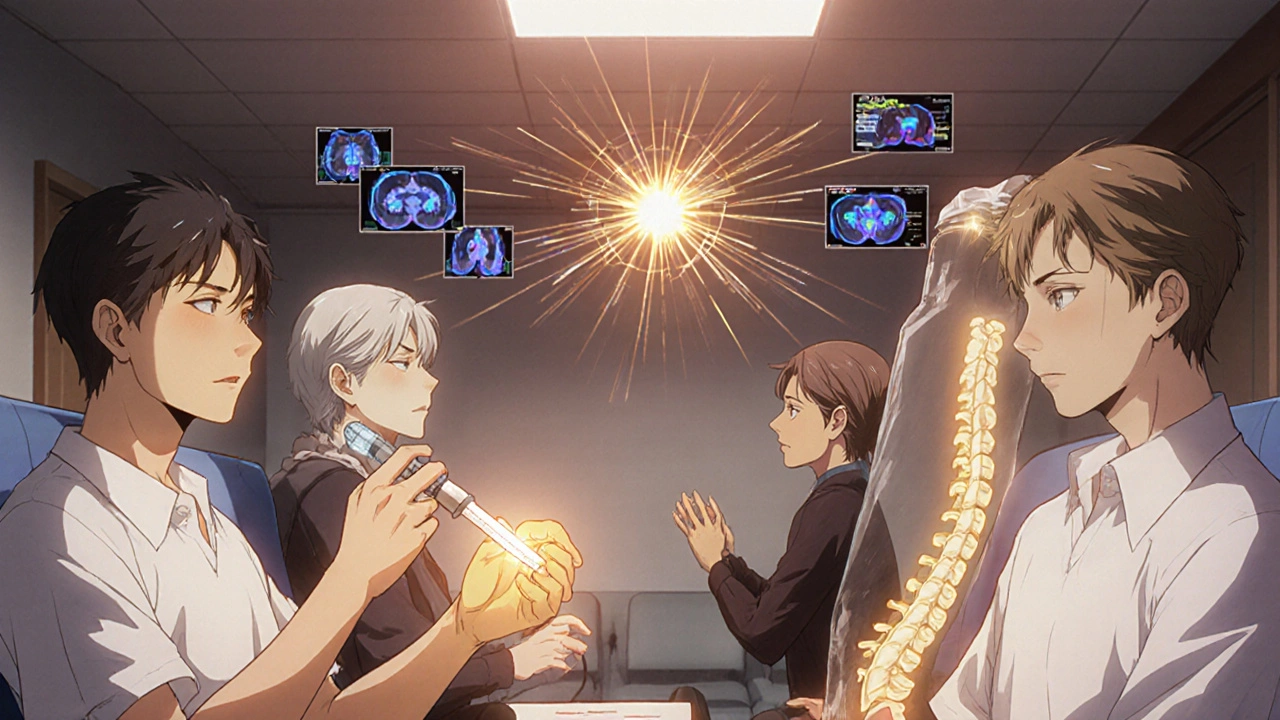
How TNF Inhibitors Work Against Spine Inflammation
TNF inhibitors are not painkillers. They don’t numb the pain. Instead, they shut down the root cause: inflammation driven by a protein called tumor necrosis factor-alpha (TNF-α).
In AS, your immune system goes rogue. It floods the sacroiliac joints and spine with TNF-α, a chemical that signals other immune cells to attack healthy tissue. This constant inflammation erodes bone, then triggers abnormal bone growth - leading to fusion. TNF inhibitors block this signal like turning off a fire alarm. Without TNF-α, the immune system calms down. Inflammation drops. Pain eases. And over time, the damage slows.
Studies using MRI scans show clear proof: after 6 months of TNF inhibitor treatment, inflammation in the spine and sacroiliac joints drops by nearly 60%. That’s not just feeling better - that’s actual healing at the tissue level. The same drugs that work for rheumatoid arthritis and Crohn’s disease are now the gold standard for AS.
The Five TNF Inhibitors Approved for AS
Five TNF inhibitors are FDA-approved for ankylosing spondylitis. Each works the same way but comes in different forms:
- Infliximab (Remicade): Given through an IV infusion every 4 to 8 weeks. Requires a clinic visit. First approved for AS in 2003.
- Etanercept (Enbrel): Injected under the skin twice a week. One of the most prescribed. Known for long-term use.
- Adalimumab (Humira): Injected under the skin every other week. Popular for its convenience and strong results.
- Certolizumab pegol (Cimzia): Injected under the skin every other week or weekly. Unique because it doesn’t cross the placenta - often chosen for patients planning pregnancy.
- Golimumab (Simponi): Injected under the skin once a month. Lowest dosing frequency of the group.
Each has different side effect profiles and costs. Etanercept has the longest track record for staying in use - many patients stay on it for over a decade. Adalimumab works fast for most people, with noticeable relief in as little as two weeks. Infliximab often works best for those with very high inflammation markers, but requires more time and trips to the clinic.
Who Benefits Most From TNF Inhibitors?
Not everyone with AS responds the same way. Doctors use clear guidelines to decide who gets these drugs:
- You’ve tried at least 4 weeks of maximum-dose NSAIDs (like naproxen or celecoxib) and still have pain.
- Your BASDAI score (a patient-reported measure of disease activity) is 4 or higher out of 10.
- Your spinal pain is rated 4 or higher.
- Your blood tests show high inflammation - CRP over 5 mg/L or ESR over 20 mm/h.
Patients who respond best tend to be younger (under 40), have had symptoms for less than 10 years, and have high CRP levels at diagnosis. One study found that 81% of patients with both elevated CRP and SAA (another inflammation marker) had a strong response to TNF inhibitors.
If you’ve had AS for over 15 years and your spine is already fused, TNF inhibitors won’t reverse that. But they can still stop further damage and reduce pain from active inflammation in remaining mobile joints.
Real Results: What Patients Experience
Patients report life-changing improvements. A survey of over 1,200 people with AS found that 78% saw “substantial improvement” after starting a TNF inhibitor. Morning stiffness dropped from over an hour to under 30 minutes for most. Many return to work, exercise, or even play with their kids again.
One patient shared: “I couldn’t tie my shoes without help. After six weeks on adalimumab, I could bend over again. I cried.”
But results aren’t instant. Most people notice changes in 2-3 weeks, but full benefits take 12 weeks. Some patients need to try more than one TNF inhibitor before finding the right one. About 30-40% of those who don’t respond to the first TNF inhibitor do respond to the second.
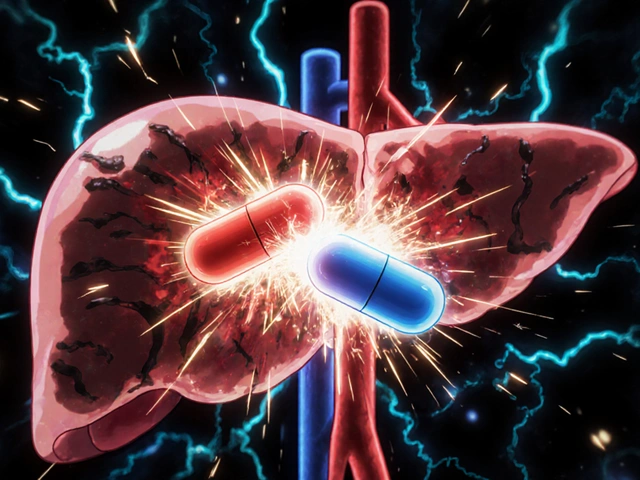
Side Effects and Risks
TNF inhibitors are powerful - and come with serious risks. The biggest concern: infections. These drugs suppress part of your immune system. That means:
- Higher risk of tuberculosis (TB). All patients get screened before starting.
- Increased chance of serious bacterial infections like pneumonia or sepsis.
- Reactivation of old hepatitis B infections.
- Rare but dangerous cases of nervous system disorders like multiple sclerosis.
Minor side effects are common: injection site redness (19% of users), headaches (12%), and upper respiratory infections (16%). Some patients develop psoriasis or worsening of existing psoriasis - especially with etanercept.
The FDA requires a black box warning on all TNF inhibitors for these risks. But for most people, the benefits far outweigh the dangers - especially when monitored properly.

Cost, Access, and Biosimilars
TNF inhibitors are expensive. Brand-name drugs like Humira cost over $20,000 a year in the U.S. But biosimilars - highly similar versions - have cut prices by 15-20%. Amjevita, a biosimilar to adalimumab, now makes up over a third of the adalimumab market.
Insurance coverage varies. In countries with universal healthcare like Germany and the UK, 65-70% of eligible patients get TNF inhibitors within two years of diagnosis. In the U.S., only 45-50% do - often because of prior authorization delays or high co-pays.
Many specialty pharmacies offer support: free training on self-injection, 24/7 nursing help, and even financial assistance programs. The Spondylitis Association of America’s “TNF Inhibitor Starter Kit” has helped over 12,000 patients navigate the process.
What Comes After TNF Inhibitors?
While TNF inhibitors are still the top choice, new options are here. IL-17 inhibitors like secukinumab and ixekizumab work differently - blocking a different inflammatory pathway. In head-to-head trials, they’re just as effective as TNF inhibitors for AS.
One advantage: they don’t carry the same TB risk. They’re now approved as first-line biologics in Europe and are gaining ground in the U.S.
But TNF inhibitors aren’t going away. They’ve been used for over 20 years. We know their long-term safety better than any newer drug. Studies show they reduce spinal damage by 50-60% if started early. That’s why the American College of Rheumatology predicts they’ll still be used in 60-65% of AS cases through 2030.
What You Can Do Today
If you have AS and still struggle with pain or stiffness despite NSAIDs, talk to your rheumatologist. Ask about:
- Your BASDAI score and CRP levels
- Whether you’re a candidate for a TNF inhibitor
- Which one might fit your lifestyle (injections vs. infusions, frequency, cost)
- Getting screened for TB and hepatitis before starting
Don’t wait until your spine fuses. Early treatment changes outcomes. You don’t have to live with constant pain. These drugs don’t cure AS - but they give you back your life.


So let me get this straight - we’re giving people biologics that suppress their entire immune system just so they can tie their shoes again? 🤡 I’d rather just live in a foam pit and call it a day.
The body is not a machine to be fixed. It is a process. To suppress TNF-alpha is to deny the intelligence of inflammation - it is not an error, but a signal.
TNF-alpha is a pro-inflammatory cytokine, but its pleiotropic nature means it also regulates tissue repair and immune homeostasis. Blocking it systemically is like deleting the entire OS because one app crashes. We need targeted delivery - not shotgun immunosuppression.
Big Pharma pushed these drugs because they knew the government would pay for them. You think this is medicine? It’s a $$$ pipeline. And they’re hiding the fact that these drugs make you more likely to get cancer. Read the FDA black box warning - it’s not a suggestion.
We live in an age where we pharmacologically silence the voice of our own biology. TNF-alpha isn’t the enemy - it’s the messenger. We’ve outsourced our suffering to a vial of monoclonal antibodies and called it progress. But what have we become? A society that fears discomfort more than death?
I’ve been on adalimumab for 3 years. It’s not perfect, but I can now play with my daughter without wincing. That’s worth the monthly blood tests and the scary injection site redness. I’m not blind to the risks, but I’m grateful for the trade-off.
Stop pretending this is science. This is just fancy placebo with a $20k price tag. Most people don’t even need biologics - they need physical therapy, sleep, and to stop eating gluten. But no, let’s pump full-body immunosuppressants into everyone who complains about back pain.
I just want to say - I know how hard it is. I’ve been living with AS for 18 years. The mornings are the worst. I used to cry just getting out of bed. When I started etanercept, it didn’t fix everything - but it gave me back the ability to breathe without thinking about pain. That’s not a miracle. It’s dignity. And I’m so glad I didn’t give up.
TNF inhibitors? More like TNF *inhibitors* 😒💸 I mean, if I could just pay $20k to stop being stiff, why don’t I just buy a robot to bend for me? 🤖😂
Honestly, I was scared to start Humira. But after 6 weeks, I could turn my head without my neck screaming. I started hiking again. My dog noticed. He’s been following me around like I’m a superhero now 🐶❤️ So yeah, it’s expensive. But it’s worth it.
This post made me cry. Not because I’m sad - because I finally feel seen. I’ve been told I’m just ‘getting older’ or ‘lazy’. But this? This is real. Thank you for writing this. I’m going to show my doctor tomorrow.
There is a metaphysical dimension to chronic pain that modern medicine refuses to acknowledge. The spine is not merely bone and cartilage - it is the axis of the soul’s expression. To chemically silence its cry is to sever the body’s dialogue with the self. We have replaced wisdom with dosage schedules. And in doing so, we have forgotten how to listen.
I’ve read through this twice, and I think it’s incredibly well-researched - especially the part about MRI evidence showing 60% inflammation reduction. But I wonder: what about long-term data beyond 10 years? Are we seeing increased rates of lymphoma? Are there epigenetic consequences? And why is there such a stark disparity in access between the U.S. and Canada/Europe? The systemic inequities here are alarming.
The use of biologics for ankylosing spondylitis is a medically justified intervention. However, the cost structure is indefensible. A drug that costs $20,000 annually in the United States while costing $3,000 in Germany is not a medical issue - it is a moral failure.
I tried all five. Only Cimzia didn’t make me break out in hives. And yes, I cried when I could finally put on socks again. 💅😭 But also - who approved this as a ‘lifestyle drug’? We’re treating autoimmune disease like it’s a subscription box.