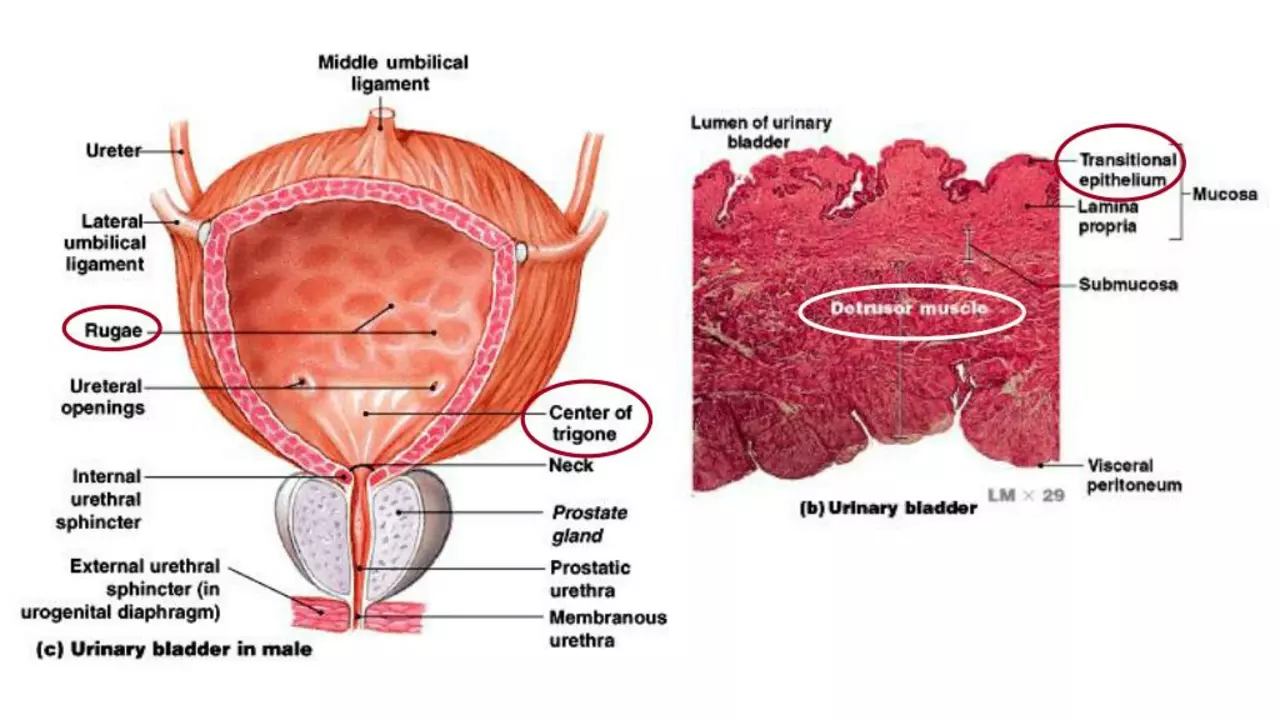
Understanding the Prostate and Its Role in the Urinary System
As a blogger and health enthusiast, I've often seen the confusion around the role of the prostate in the urinary system. The prostate is a small, walnut-shaped gland in men that produces seminal fluid, which nourishes and transports sperm. It is located just below the bladder and surrounds part of the urethra, the tube that carries urine and semen out of the body. This strategic location means any change in the size or health of the prostate can have direct implications on urinary functions. When the prostate is in good health, you may not even notice it's there. But when things go wrong, urinary symptoms can quickly become a major concern.
Linking Prostate Health to Urinary Incontinence
As I've learned through my research and speaking with medical professionals, there's a strong link between prostate health and urinary incontinence. An enlarged prostate, for instance, can press against the urethra, causing difficulties in urination. This condition is common in older men and is known as Benign Prostatic Hyperplasia (BPH). It often results in symptoms like frequent urination, difficulty starting and stopping urination, and urinary incontinence. It's important to be aware of these symptoms, as they can significantly impact your quality of life and could potentially signal more serious prostate conditions, such as prostate cancer.
Prostate Cancer: A Silent Contributor to Urinary Symptoms
One of the most alarming things I've discovered is the connection between prostate cancer and urinary incontinence. Prostate cancer is the second most common cancer in men worldwide. The scary part is that it often doesn't present any symptoms in its early stages. However, as the disease progresses, symptoms similar to BPH might start to appear, including urinary incontinence. Therefore, it's crucial for men, especially those over the age of 50, to get regular prostate check-ups. Early detection often results in better outcomes.
Diagnosing and Treating Prostate-Related Urinary Incontinence
The diagnosis of prostate-related urinary incontinence often involves a number of tests, including a digital rectal exam, prostate-specific antigen (PSA) test, and possibly a biopsy. Treatment options can range from medication to surgery, depending on the severity of the condition. I've found it reassuring to know that many men with BPH or prostate cancer can regain control over their urinary function with the right treatment. Managing these symptoms can greatly improve one's quality of life.
Maintaining Prostate Health for Better Urinary Function
As with many health issues, prevention is often the best cure. Maintaining prostate health can help to prevent urinary incontinence and other urinary symptoms. This can include a healthy diet, regular exercise, and avoiding certain risk factors like smoking and excessive alcohol. Regular check-ups are also vital, especially as you get older. Remember, your prostate health directly affects your urinary function, so take care of it to ensure a good quality of life.
As someone who believes in the power of knowledge for better health, I hope this information proves helpful. Stay informed, stay healthy, and remember to pay attention to your body's signals.



Keep up the habit of regular check‑ups; they’re the simplest safeguard.
Your post glosses over the fact that many men ignore symptoms until the disease is advanced, a dangerous neglect that the healthcare system seems to tolerate. It also downplays the financial incentives driving over‑diagnosis. The aggressive tone about medication sidesteps the real issue of profit‑driven prescriptions. In short, the narrative needs a harsher critique of systemic complacency.
Reading this reminded me of the countless friends who thought a few extra trips to the bathroom were just "getting older." The truth is, early detection can spare them months of anxiety and invasive treatments. A simple PSA test and a digital exam can flag issues before they become debilitating. Also, lifestyle tweaks like a Mediterranean diet can markedly improve prostate health. Keep sharing this info – it empowers men to take charge of their bodies.
What most people don’t realize is that the push for widespread PSA screening is part of a larger agenda to keep populations dependent on pharmaceutical solutions. Governments profit from the chronic management of prostate issues, while the real cure lies in natural prevention. The statistics cited are often cherry‑picked to sell a narrative that keeps us in a state of fear. It’s time we question who really benefits from the alarmist tone.
Big Pharma’s shadow looms over every ‘health tip’ we see online. They sprinkle fear about prostate cancer to sell endless rounds of expensive drugs. Meanwhile, ancient herbal practices that actually support prostate function are buried beneath glossy ads. Don’t be fooled – the truth is tastier than their glossy brochures.
Hey folks, great rundown! Just a reminder: staying active and staying hydrated can do wonders for bladder control. If you haven’t spoken to a doc in a while, now’s a good time.
It’s chilling how the elite medical circles keep the real causes of prostate woes hidden, pushing us toward invasive surgeries instead of natural solutions. Their glossy journals whisper of “research” while quietly pouring money into risky procedures. The drama isn’t just in the symptoms; it’s in the hidden curricula of profit over health. Wake up, people.
One must acknowledge that moral responsibility extends beyond personal health; societal negligence in promoting preventive screenings is indefensible. It is incumbent upon us to advocate for accessible, evidence‑based education, lest we perpetuate avoidable suffering. Therefore, let us champion policies that prioritize early detection and holistic care.
Yo, you’re right on that – ignoring health is just plain lazy. We gotta stop being complacent and start living responsibly. #NoExcuses
Prostate physiology intersects with urodynamic homeostasis through a cascade of androgen‑mediated signaling pathways, which modulate smooth muscle tone in the peri‑urethral zone.
When hyperplastic growth encroaches upon the prostatic urethra, the resultant increase in intraluminal pressure precipitates frequency and urgency phenotypes.
Clinicians often employ the International Prostate Symptom Score (IPSS) as a quantifiable metric to stratify severity, yet the score fails to capture nuanced neuro‑genic contributions to incontinence.
Emerging literature suggests that chronic inflammation-marked by elevated cytokines such as IL‑6 and TNF‑α-accelerates stromal proliferation, thereby compounding obstructive sequelae.
From a preventive standpoint, dietary phytochemicals like lycopene and epigallocatechin gallate have demonstrated modulatory effects on androgen receptor activity, offering a chemopreventive avenue.
Exercise-induced hormonal balance, particularly the regulation of insulin‑like growth factor 1 (IGF‑1), further attenuates proliferative signaling within prostatic tissue.
On the diagnostic front, multiparametric MRI now provides high‑resolution mapping of zonal anatomy, enabling targeted biopsies and reducing overtreatment.
Therapeutically, alpha‑blockers alleviate dynamic obstruction by relaxing smooth muscle, whereas 5‑alpha‑reductase inhibitors shrink glandular volume through androgen suppression.
In refractory cases, minimally invasive laser ablation or transurethral resection offers symptom relief while preserving sexual function.
Nonetheless, patient counseling must encompass the psychosocial impact of urinary incontinence, as it correlates with diminished quality‑of‑life indices.
Holistic management therefore integrates pharmacologic, behavioral, and lifestyle interventions, each calibrated to the individual's pathophysiology.
Future research avenues include gene‑editing strategies targeting TMPRSS2‑ERG fusion transcripts implicated in oncogenic pathways.
Moreover, microbiome modulation is an emerging field, with preliminary data linking dysbiosis to prostatic inflammation.
In sum, a multidisciplinary approach-bridging urology, endocrinology, and behavioral health-optimizes outcomes for men navigating prostate‑related urinary challenges.
Continued patient education and routine screening remain the cornerstone of early detection and effective intervention.