Antifungals: What They Are, How They Work, and What You Need to Know
When you hear antifungals, medications designed to kill or stop the growth of fungi that cause infections in humans. Also known as antimycotics, they’re not just for athlete’s foot—they’re critical for treating everything from vaginal yeast infections to life-threatening systemic fungal diseases. Unlike antibiotics that target bacteria, antifungals go after fungi—organisms like Candida, Aspergillus, and dermatophytes—that thrive in warm, moist areas of the body. These aren’t rare problems: over 75% of women will get at least one yeast infection in their lifetime, and many of those cases happen after taking antibiotics.
Antibiotics wipe out good bacteria that normally keep fungi in check, which is why yeast infection, a common fungal overgrowth caused mainly by Candida albicans is one of the most frequent side effects of antibiotic use. That’s why antifungal treatment, the use of drugs like fluconazole, clotrimazole, or nystatin to restore microbial balance is often prescribed alongside or right after antibiotics. But antifungals aren’t one-size-fits-all. Topical creams work for skin and vaginal infections, while oral or IV versions are needed for deeper infections like oral thrush or invasive candidiasis. And they’re not harmless—some can strain your liver or interact with heart meds, which is why you shouldn’t self-treat without knowing what you’re dealing with.
What you might not realize is that fungal infections can be sneaky. A persistent rash that won’t quit, recurring itching, or even digestive issues after antibiotics could be signs of an underlying fungal imbalance. The fungal infections, conditions caused by fungi invading skin, nails, mucous membranes, or internal organs we treat aren’t always obvious. Some people think if it’s not a visible rash, it’s not fungal—but that’s not true. Oral thrush, nail fungus, and even some chronic sinus issues are fungal in origin and need targeted antifungals, not just steroids or antihistamines.
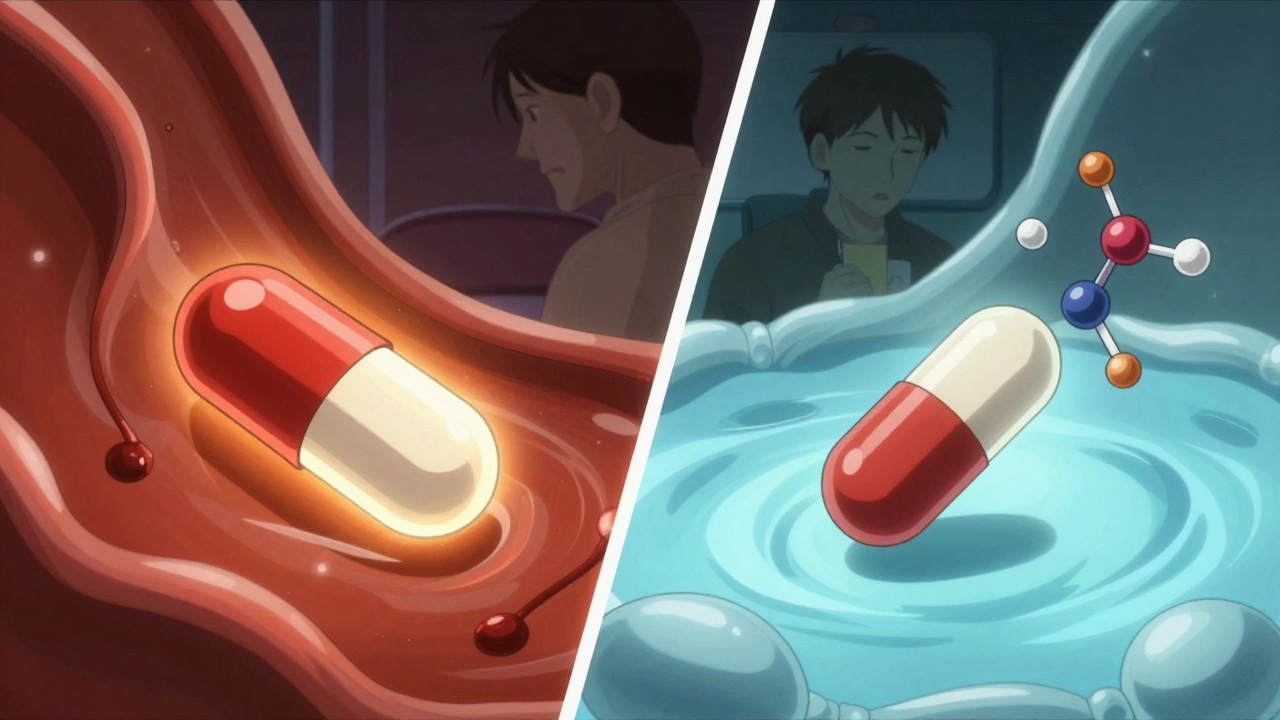
And here’s the thing: not every antifungal works the same way. Some stop fungi from building cell walls, others disrupt their membranes, and a few even interfere with their DNA. That’s why some treatments fail—not because the infection is resistant, but because the wrong drug was picked. That’s also why you’ll see posts here about how antibiotics trigger yeast infections, how to prevent them, and what actually works when over-the-counter creams don’t cut it. You’ll find real advice on probiotics, dosing, and how to spot when you need more than a cream. No fluff. No marketing. Just what you need to know to protect yourself—and know when to ask for help.
Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption and Effectiveness
Proton pump inhibitors can severely reduce absorption of key antifungals like itraconazole and ketoconazole, leading to treatment failure. Fluconazole is safer, but interactions with liver enzymes still matter. New research hints PPIs might even boost antifungal power in resistant infections.