PPI-Antifungal Interaction Checker
Check Your Medication Combination
When you're taking a proton pump inhibitor (PPI) for heartburn and suddenly need an antifungal for a stubborn yeast infection, things can get complicated-fast. These two types of medications don’t just sit quietly in your body. They bump into each other in ways that can make one or both of them fail. And it’s not just a theory. Real patients are getting sicker because of it.
Why Your Heartburn Medicine Might Be Killing Your Antifungal
Proton pump inhibitors like omeprazole, pantoprazole, and esomeprazole work by shutting down the acid pumps in your stomach. That’s great if you have acid reflux. But it’s a disaster for some antifungals. Why? Because drugs like itraconazole and ketoconazole need stomach acid to dissolve properly. Without it, they just sit there, undissolved, and never get absorbed. A 2023 study in JAMA Network Open looked at 1,243 patients and found that when PPIs were taken with itraconazole, the amount of drug in the bloodstream dropped by 60%. That’s not a small drop. That’s the difference between a drug working and not working at all. For ketoconazole, the drop is just as bad. At a stomach pH of 6.8 (common with PPI use), ketoconazole’s solubility plummets from 22 mg/mL to just 0.02 mg/mL. In plain terms: your body can’t absorb it.Fluconazole Is the Exception-And Why It Matters
Not all antifungals are affected the same way. Fluconazole doesn’t care about stomach acid. It dissolves easily in water, no matter how alkaline your stomach is. Its bioavailability stays steady at 90%±5%, even with a PPI running interference. That’s why doctors often switch patients from itraconazole to fluconazole when PPIs are needed. But here’s the catch: fluconazole isn’t harmless. It messes with your liver enzymes. Specifically, it blocks CYP2C9 and, at higher doses, CYP3A4. That means if you’re also on warfarin, you could end up with dangerously high blood-thinning levels. A 2023 FDA database shows fluconazole can require a 20-30% reduction in warfarin dose. So even if absorption isn’t an issue, you’re trading one risk for another.Voriconazole: A Trickier Case
Voriconazole doesn’t suffer from poor absorption like itraconazole. But it has its own problem. It’s broken down by liver enzymes CYP2C19 and CYP3A4. And guess what? Some PPIs-especially pantoprazole and omeprazole-are strong inhibitors of CYP2C19. That means voriconazole sticks around longer than it should. A 2015 study in Antimicrobial Agents and Chemotherapy showed that when voriconazole and pantoprazole are taken together, voriconazole clearance drops by 25-35%. That leads to higher blood levels. Too high. And that raises the risk of side effects: vision changes, liver damage, even hallucinations. That’s why the Cleveland Clinic now requires voriconazole blood levels to be checked within 72 hours of starting a PPI. Dose adjustments of 25-50% are common.
The Paradox: PPIs Might Actually Help Antifungals
Here’s where it gets weird. While PPIs wreck absorption of some antifungals, new research suggests they might make them stronger inside the body. A 2024 study in PMC10831725 found that omeprazole can block a fungal enzyme called Pam1p-a pump that Candida uses to push antifungals out of its cells. In lab tests, omeprazole made fluconazole 4 to 8 times more effective against drug-resistant Candida glabrata. That’s not a lab curiosity. It’s a potential game-changer. Dr. Mahmoud Ghannoum from Case Western Reserve University called it a "new therapeutic possibility." Imagine using a cheap, widely available heartburn drug to boost the power of antifungals in resistant infections. A Phase II trial at Johns Hopkins is now testing omeprazole 40mg daily with fluconazole for stubborn candidiasis. Results are due in late 2025.What Doctors Actually Do in Real Life
In practice, most infectious disease specialists avoid the whole mess. A 2023 survey of 217 pharmacists found that 87% prefer switching to echinocandins-drugs like caspofungin-when a patient needs both a PPI and an antifungal. Why? Because echinocandins don’t rely on stomach acid or liver enzymes. They’re given intravenously. No absorption issues. No enzyme conflicts. But that’s not always possible. For outpatients, IV drugs aren’t practical. So what’s the next best thing? Timing. The UCSF protocol says: give itraconazole at least two hours before the PPI. Mayo Clinic recommends four to six hours. It helps-reducing the absorption drop from 60% to 45%-but it’s not a fix. And even then, therapeutic drug monitoring is required. You need blood tests to confirm the drug is working.
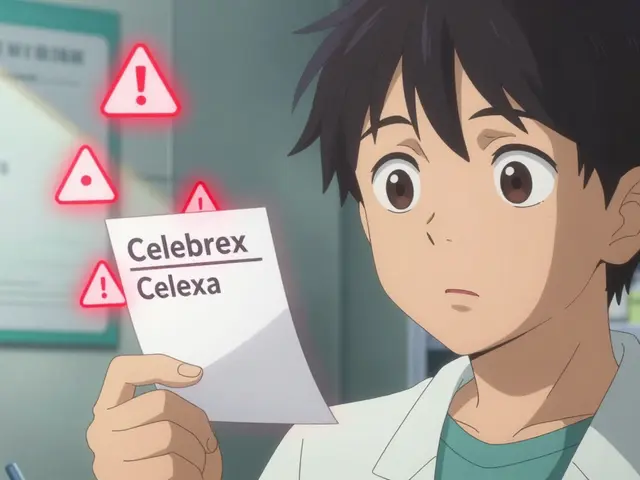
Regulations and Reality Don’t Match
The FDA added a black box warning to itraconazole in June 2023: "Concomitant use with PPIs is contraindicated." The EMA followed in September. That’s the strongest possible warning. Yet a 2024 audit by the Institute for Safe Medication Practices found that over 22% of itraconazole prescriptions in pharmacies were still being paired with PPIs. Why? Because many prescribers don’t know. Or they think "it’s just a little heartburn medicine." Or they assume the patient will figure it out. The cost of this ignorance? A 2024 JAMA Internal Medicine study estimated $327 million a year in extra hospital stays, failed treatments, and emergency visits-all because of a simple drug interaction that’s been known for over a decade.What’s Coming Next
The future might solve this problem. The FDA is funding research into new formulations of itraconazole that don’t need acid to work. One submicron particle version (SUBA-itraconazole) showed 92% bioavailability even with high stomach pH in a 2023 trial. That means you could take it with your PPI and still get full effect. Dr. Thomas J. Walsh from Weill Cornell Medicine predicts these pH-independent formulations will be common within five years. Until then, the rules are simple:- Avoid itraconazole and ketoconazole with PPIs. Period.
- If you must use voriconazole, check blood levels after 72 hours of starting the PPI.
- Fluconazole is safe for absorption-but watch for interactions with blood thinners.
- When in doubt, switch to an echinocandin.
Drug interactions aren’t just academic. They’re life-or-death. A missed interaction can turn a treatable infection into a fatal one. And in a world where PPIs are among the most prescribed drugs in the U.S.-over 124 million prescriptions a year-it’s not a rare edge case. It’s a daily risk.
Can I take fluconazole with a proton pump inhibitor?
Yes, fluconazole can be safely taken with proton pump inhibitors. Unlike itraconazole or ketoconazole, fluconazole doesn’t need stomach acid to be absorbed. Its bioavailability stays high (90%±5%) regardless of gastric pH. However, fluconazole can interfere with other medications like warfarin by blocking liver enzymes (CYP2C9), so your doctor may need to adjust your warfarin dose if you’re taking both.
Why is itraconazole so sensitive to PPIs?
Itraconazole is highly fat-soluble and needs an acidic environment to dissolve in the stomach. Proton pump inhibitors raise stomach pH from around 1.5-2.5 to 4-6, which makes itraconazole practically insoluble. Studies show this cuts its absorption by up to 60%, leading to blood levels too low to fight infection. That’s why it’s now contraindicated with PPIs by the FDA and EMA.
What should I do if I’m on a PPI and need an antifungal?
Talk to your doctor or pharmacist immediately. Avoid itraconazole and ketoconazole completely. Fluconazole is usually safe for absorption, but check for interactions with other meds like blood thinners. If you need a stronger antifungal, ask about echinocandins like caspofungin, which are given by IV and don’t interact with stomach acid or liver enzymes. If you must use voriconazole, expect blood tests within 72 hours of starting the PPI.
Do all proton pump inhibitors affect antifungals the same way?
No. All PPIs raise stomach pH similarly, so they all reduce absorption of acid-dependent antifungals like itraconazole. But when it comes to liver enzyme effects, some PPIs are stronger than others. Omeprazole and pantoprazole are potent inhibitors of CYP2C19, which affects voriconazole levels. Esomeprazole and dexlansoprazole have less effect on liver enzymes. So while absorption issues are the same across all PPIs, metabolic interactions vary.
Is there any benefit to taking PPIs with antifungals?
Emerging research suggests yes-but only in specific cases. A 2024 study found that omeprazole can block a fungal pump (Pam1p) that Candida uses to expel fluconazole. This makes the antifungal 4-8 times more effective against resistant strains in lab tests. A clinical trial is now testing whether adding omeprazole to fluconazole can treat stubborn yeast infections. This is still experimental, but it could one day turn a heartburn drug into an antifungal booster.



Yo, this is wild. I had a friend on omeprazole for years, then got a nasty fungal infection - doc prescribed itraconazole, and she ended up in the ER. No one told her about the interaction. Like, how is this still happening? 🤯 PPIs are OTC for crying out loud. We need better alerts in pharmacies. Not just "consult your doctor" - that’s lazy. Real warnings. Like, big red flags. This isn’t theoretical. People are dying because of paperwork gaps. 😔
Fluconazole CYP2C9 inhibition > absorption issues. Clinical pharmacokinetics 101. PPIs alter gastric pH but fluconazole is water soluble. No issue. But CYP interactions are real. Warfarin INR spikes = hemorrhage risk. Simple.
It’s not just about pharmacokinetics - it’s about systemic negligence. We’ve turned medicine into a spreadsheet of checkboxes and profit margins. Doctors don’t have time to learn interactions, pharmacists are overworked, and patients are left to Google their own side effects. And now we’re talking about *boosting* antifungals with heartburn meds? This isn’t innovation - it’s a symptom of a broken system where we patch problems with more drugs instead of fixing the root. We need to stop treating symptoms and start treating the culture of carelessness.
One must acknowledge the epistemological dissonance inherent in pharmaceutical policy. The FDA’s black box warning is a performative gesture - a symbolic gesture of regulatory authority that does not alter the ontological reality of clinical practice. The fact that 22% of prescriptions still violate this warning reveals not ignorance, but a deeper epistemic collapse: the medical establishment has surrendered to logistical convenience over epistemic rigor. The patient is not a subject of care, but a variable in a cost-benefit algorithm. This is not malpractice - it is systemic nihilism.
I’m on PPIs for acid reflux and just started fluconazole for a yeast infection. My pharmacist actually flagged it and asked if I was on blood thinners. I wasn’t… but now I’m scared to start. Like, how do I even know what else I’m on that might mess with this? My doctor didn’t even ask. 😩
I’ve seen this play out in the ICU. A patient on pantoprazole for stress ulcers gets candidemia. Prescribed voriconazole. No baseline level checked. By day 3, they’re seeing halos, liver enzymes spiking. We had to pull the PPI, hold the antifungal, wait 48 hours, then re-dose. It’s not complicated. But in the chaos of a busy floor? It gets missed. Again and again. We need protocols. Not just guidelines. Mandatory checks. Like a checklist. Like seatbelts. Because people die when we assume.
So now we’re supposed to trust that some guy in a lab found that omeprazole makes fluconazole work better? Like, what’s next? Taking aspirin to cure cancer? This country’s gone mad. We’re turning medicine into a sci-fi novel. And now we’re gonna give healthy people heartburn pills just to make antifungals "stronger"? No. Just no. This is dangerous nonsense.
Oh wow. So the solution to PPIs killing antifungals is… to use MORE PPIs to make the antifungals work better? Genius. Absolute genius. The same drug that breaks absorption now fixes resistance? That’s not science - that’s magic. Or maybe just bad math. I’m starting to think the FDA just rubber-stamps whatever Big Pharma pays for. 🤡
Wait so if fluconazole + omeprazole = 8x stronger against resistant Candida… does that mean I could lower my fluconazole dose? Like, 50mg instead of 150mg? That’d be huge. Less liver stress, cheaper, fewer side effects. Is anyone testing that? 😮
bro i took itraconazole with omeprazole for like 3 weeks and thought i was fine… then my skin started peeling and i thought i had eczema. turns out the drug just wasn’t working and i got a full body fungal rash. like… why does no one tell you this stuff? i had to google it myself. rip my skin 😭
Fluconazole works. Echinocandins cost too much. PPIs are everywhere. Simple fix: switch to fluconazole. No drama. No IV. No chaos. Done.
in india we dont have much choice. fluconazole is cheap. voriconazole is rare. echinocandins? only in big hospitals. so we use itraconazole with PPI and hope. its not ideal but its what we have. no one checks levels. no one has time. its just… life.
So let me get this straight. The FDA says "don’t mix" but 22% of prescriptions still do… and now we’re gonna turn PPIs into antifungal enhancers? 😏 Congrats, we’ve turned pharmacology into a Russian nesting doll of contradictions. Next up: Add Adderall to antibiotics for better bioavailability. Because why not?
Pharmacokinetics is a western obsession. In traditional medicine, we use turmeric, neem, garlic. No PPIs needed. No CYP450 nonsense. Just nature. You want to kill fungus? Burn it out. Not confuse it with chemical cocktails. This is overengineered. Overpriced. Overrated.