Using steroid eye drops can be a game-changer for serious eye inflammation-but only if you know exactly what you're getting into. These powerful medications, like prednisolone acetate and a corticosteroid used to treat inflammation in the eye, including uveitis and allergic conjunctivitis, can stop swelling and pain fast. But they’re not harmless. Left unchecked, they can silently damage your vision-sometimes before you even notice something’s wrong.
Why Doctors Prescribe Steroid Eye Drops
Steroid eye drops work by shutting down the body’s inflammatory response. When your eye is swollen from uveitis, severe allergies, or even a chemical burn, your immune system goes into overdrive. That’s helpful for healing-but too much inflammation can scar your cornea, damage your retina, or even cause permanent vision loss. That’s where these drops come in.
They’re not for everyday red eyes or mild irritation. They’re reserved for serious, non-infectious conditions. For example, if you have anterior uveitis-an inflammation deep inside the eye-steroid drops are often the fastest way to protect your sight. Studies show patients respond well when used correctly, with inflammation clearing up in days to weeks. The goal isn’t to use them forever. It’s to get the inflammation under control as quickly as possible, then taper off.
Drugs like loteprednol etabonate and a steroid designed to break down quickly in the eye, reducing systemic side effects were developed to lower risks, but even these aren’t risk-free. The key is matching the right drug to the right condition-and using it for the shortest time possible.
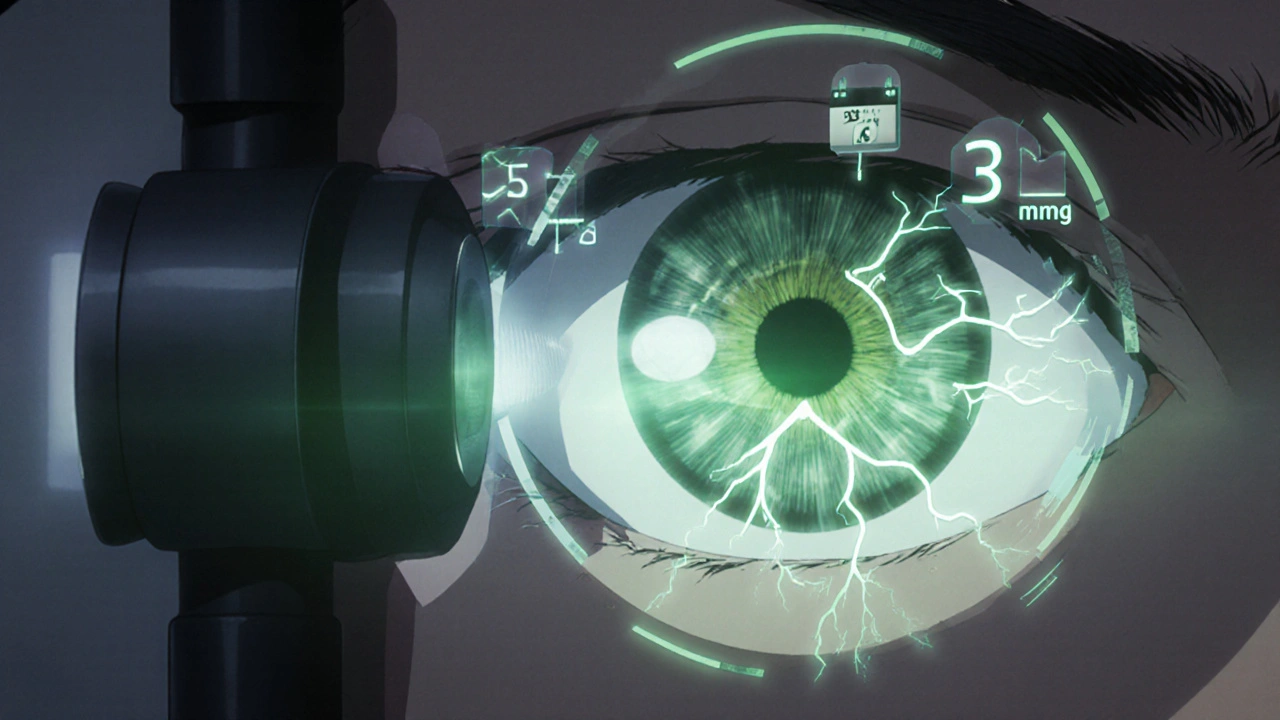
The Hidden Dangers: Steroid-Induced Glaucoma
One of the scariest side effects? Elevated eye pressure. It doesn’t hurt. It doesn’t cause redness or blurry vision at first. That’s why it’s so dangerous.
Up to 40% of people using steroid eye drops will see some rise in intraocular pressure (IOP). Most of those cases are mild and go away when the drops stop. But 4-6% of users are "steroid responders"-their pressure spikes dangerously high, often above 30 mmHg. That’s the threshold where optic nerve damage begins.
Once the nerve is damaged, vision loss is permanent. And because glaucoma from steroids often shows no symptoms until it’s advanced, you can’t rely on how your eye feels. You need regular pressure checks. The standard is every 2-4 weeks if you’re on drops longer than 10 days. If you have a family history of glaucoma, diabetes, or already have high eye pressure, your doctor may want to check you every week.
Goldmann applanation tonometry is the gold standard for measuring this pressure. It’s not a quick poke-it’s a precise test done with a special instrument after numbing your eye. Skipping these appointments is one of the biggest mistakes people make.
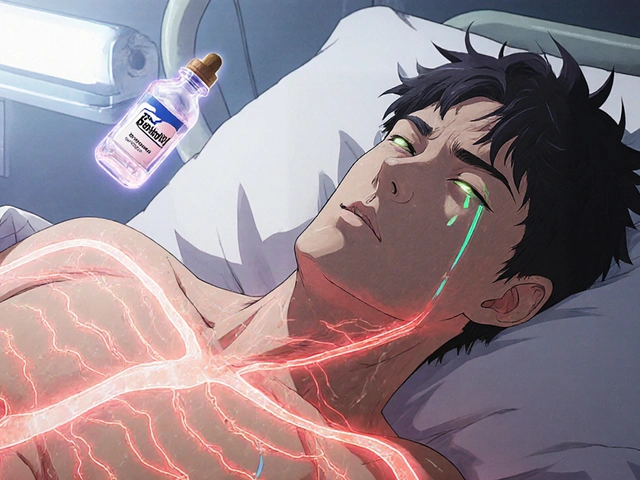
Cataracts: The Slow-Moving Threat
Another major risk? Cataracts. Not the kind you get with age-these are posterior subcapsular cataracts. They form right in the center of your lens, where light passes through. That means even small clouding can blur your vision significantly.
Using steroid drops for more than 10 days increases the risk. After three to six months of continuous use, the chance of developing them jumps sharply. In some cases, steroid use can bring cataract surgery forward by five to ten years.
Unlike glaucoma, cataracts usually cause noticeable symptoms: glare from headlights, faded colors, double vision in one eye, or trouble reading in low light. But even then, many patients delay treatment, thinking it’s just "getting older." The truth? If steroids caused it, it’s not normal aging-it’s preventable damage.
Cataract surgery is highly successful-95% of patients regain clear vision. But it’s still surgery. There’s a small risk of infection, bleeding, or a cloudy membrane forming behind the new lens (posterior capsule opacification). Avoiding the cataract in the first place is always better than fixing it later.
When Steroids Make Infections Worse
Steroids don’t just calm inflammation-they suppress your eye’s immune defenses. That means bacteria, viruses, and fungi can take over unchecked.
The most dangerous infections linked to steroid use include herpes simplex keratitis (a viral infection that can scar the cornea) and fungal keratitis (often from contaminated drops or contact lens use). These can destroy your cornea in days if not caught early.
That’s why doctors always check for infection before prescribing steroids. If you have a history of cold sores near your eye, you may need antiviral medication alongside the steroid. Never use steroid drops if your eye is infected-you’re just feeding the problem.
Also, never share your eye drops. A single drop can carry pathogens from one person to another. Always close the bottle tightly after use, and throw it out after four weeks, even if there’s liquid left. Bacteria grow fast in open bottles.
How Long Is Too Long?
There’s no one-size-fits-all answer, but general guidelines exist.
- Less than two weeks: Low risk for most people. Side effects are rare.
- Two to four weeks: Moderate risk. Monitor pressure at least once.
- More than four weeks: High risk. Glaucoma and cataracts become likely without close monitoring.
For acute conditions like uveitis, most patients use steroid drops for one to two months. After that, doctors try to taper the dose or switch to non-steroidal alternatives like ketorolac and a nonsteroidal anti-inflammatory drug (NSAID) used for eye inflammation, with fewer side effects than steroids. These don’t pack the same punch, but they’re safer for long-term use.
If you need ongoing treatment-for example, because you have chronic uveitis-your doctor should refer you to an ophthalmologist. They’ll track your pressure, check your lens, and monitor your optic nerve with visual field tests. This isn’t optional. It’s standard care.
What Symptoms Should You Watch For?
Don’t wait for your next appointment if you notice any of these:
- Blurry vision that doesn’t improve
- Eye pain or pressure behind the eye
- Seeing halos around lights
- Loss of peripheral vision (tunnel vision)
- Nausea or vomiting with eye pain
- Redness returning after it had cleared
These aren’t normal side effects. They’re warning signs. Call your eye doctor immediately. Delaying care can mean the difference between saving your vision and losing it.
Stopping Steroid Drops: Don’t Quit Cold Turkey
Many people stop steroid drops as soon as their eye feels better. That’s a mistake.
Stopping suddenly can trigger rebound inflammation-your eye gets worse than before. That’s why doctors always taper the dose. You might go from four times a day, to twice a day, to every other day, over a week or two. Follow the schedule exactly. If you miss a dose, don’t double up. Just go back to your regular schedule.
Also, never reuse old bottles. Steroid drops don’t last forever. Once opened, they should be discarded after 28 days. Even if they look fine, they can harbor bacteria.
Who’s at Highest Risk?
Not everyone reacts the same way. You’re more likely to have serious side effects if you:
- Have glaucoma or a family history of it
- Have diabetes
- Are over 40
- Have had cataract surgery before
- Use high-potency steroids like prednisolone acetate
- Use drops for more than four weeks
If any of these apply to you, your doctor should be extra cautious. They may start you on a lower-potency steroid, limit the duration, or combine treatment with pressure-lowering drops.
Alternatives to Steroids
For chronic inflammation, steroids aren’t the only option. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ketorolac or diclofenac can help manage mild to moderate inflammation without raising eye pressure or causing cataracts. They’re not as strong, but they’re safer for long-term use.
In some cases, immunosuppressants like cyclosporine eye drops (Restasis) or tacrolimus are used for autoimmune-related eye inflammation. These take longer to work but avoid the risks of steroids entirely.
For severe, persistent cases, doctors may recommend injections around the eye or oral medications. The goal is always the same: control inflammation with the least risky tool possible.
Can steroid eye drops cause blindness?
Yes, if used improperly or without monitoring. Steroid-induced glaucoma can damage the optic nerve permanently, leading to irreversible vision loss. Cataracts caused by steroids can also severely impair vision. Both conditions progress silently, so regular eye pressure checks and exams are critical to prevent blindness.
How often should I get my eye pressure checked while using steroid drops?
If you’re using steroid eye drops for more than 10 days, you should have your eye pressure checked every 2 to 4 weeks. If you’re at high risk-due to diabetes, glaucoma, or family history-your doctor may want checks every week. Never skip these appointments.
Are steroid eye drops safe for children?
They can be, but only under strict supervision. Children are more sensitive to steroid side effects, especially increased eye pressure and cataract formation. Use is typically limited to short courses for severe inflammation, and pressure monitoring is even more critical. Always follow your pediatric ophthalmologist’s instructions.
What’s the difference between prednisolone and loteprednol eye drops?
Prednisolone is a potent steroid that stays active longer in the eye, making it very effective but also higher risk for side effects. Loteprednol is designed to break down quickly after use, reducing the chance of pressure spikes and cataracts. It’s often preferred for longer-term treatment or for patients at higher risk.
Can I use steroid eye drops with contact lenses?
Generally, no. Steroid drops can increase the risk of infection, and wearing contacts while using them makes that risk much higher. Remove your lenses before applying drops and wait at least 15 minutes before putting them back in. Your doctor may advise you to stop wearing contacts entirely during treatment.
What should I do if I run out of steroid drops before my next appointment?
Don’t refill them without talking to your doctor. Using them longer than prescribed increases your risk of serious side effects. If you’re still experiencing symptoms, contact your eye care provider immediately. They may need to adjust your treatment plan or schedule an urgent checkup.
Final Thoughts: Use Wisely, Monitor Religiously
Steroid eye drops are powerful tools. They can save vision in moments of crisis. But they’re not a quick fix. They’re a medical intervention that demands responsibility.
If you’re prescribed them, ask your doctor: How long should I use them? What symptoms mean I need to call? When’s my next pressure check? Write it down. Don’t assume you’ll remember.
And if you’ve been on them for weeks-don’t just wait for your next appointment. Take charge. Ask for a tonometry test. Ask about your lens. Ask if you’re at risk. Your eyes can’t tell you when something’s wrong. You have to speak up.




People think these drops are candy. They’re not. I’ve seen patients go blind because they didn’t get their IOP checked. If your doctor doesn’t schedule follow-ups, find a new one. Period.
Bro, I used these for my allergies and thought I was fine 😅 Then I got a 38mmHg reading and nearly lost my sight. Don’t be me. Get checked. 🙏
Man, I appreciate how detailed this is. I’ve been on loteprednol for 6 weeks now for uveitis, and my doc has me on weekly pressure checks. It’s a pain, but way better than losing vision. Also, never share drops-my cousin did that and got a fungal infection. Yikes.
And yeah, the bottle expires after 28 days. Even if it looks clear. Bacteria don’t care how clean you think you are.
I switched from prednisolone to loteprednol after my first scare. Big difference. Less scary, still works. My doc says it’s like swapping a flamethrower for a blowtorch.
Also, if you wear contacts? Just don’t. Seriously. I threw mine out for the whole course. My eyes thanked me.
And don’t stop the drops cold turkey. I did that once-rebound inflammation hit like a truck. Took two weeks to get back under control. Tapering isn’t optional. It’s survival.
NSAIDs? Yeah, they’re weaker, but if you’re on long-term, they’re the smart play. I’m on ketorolac now, and my pressure’s stable. No cataracts yet, knock on wood.
And if you’ve got diabetes? You’re already on the high-risk list. Don’t play games. Get checked every week. No excuses.
My mom had steroid-induced cataracts at 52. She needed surgery. She’s fine now, but it was scary. Don’t wait until you’re seeing halos.
Also, if you’ve had cold sores near your eye? Tell your doctor. You might need antivirals on deck. Herpes doesn’t wait for permission to wreck your cornea.
And yes, kids can use these-but only under a pediatric ophthalmologist. My nephew got them for severe allergic conjunctivitis. Weekly checks. No exceptions.
Bottom line: steroids save sight. But they’ll take it if you’re lazy. Stay vigilant.
They’re hiding the truth. The FDA knows steroid drops cause blindness. They let pharma push them because they make billions. Your doctor? They’re paid by Big Pharma too. Check the PAC donations. Look up the reps who visit clinics. It’s all connected.
And why do they say ‘taper off’? Because if you stop cold, your body goes into shock. That’s not medicine-that’s addiction. They’re creating dependency.
And don’t even get me started on tonometry. It’s invasive. They’re numbing your eye, then poking it with a machine that’s been used on 50 people before you. No sterilization logs. No proof. You’re a lab rat.
Use natural remedies. Cold tea bags. Turmeric. Don’t trust the system.
You think 40% of people get IOP spikes? That’s lowballing. I’ve seen 60% in my clinic. And 4-6% are steroid responders? Try 12%. You’re not special. You’re not immune. You’re just lucky so far.
And don’t tell me ‘my doctor said it’s fine.’ Your doctor doesn’t know your genetics. Your family history? That’s your real risk factor. If your grandpa had glaucoma, you’re already on borrowed time.
NSAIDs? They’re for people who want to feel better but don’t want to actually fix anything. You want results? Use the steroid. But get checked. Every. Single. Week.
And if you think cataracts are ‘just aging’-you’re an idiot. I’ve seen 35-year-olds with steroid cataracts. You’re not old. You’re reckless.
Stop making excuses. This isn’t a suggestion. It’s a warning. Your eyes don’t have a ‘undo’ button.
Oh wow, a whole essay on steroid drops. Let me guess-you’re the guy who reads the insert before taking Advil?
Look, I’ve been using prednisolone for chronic uveitis for 18 months. I’m on a taper. I get checked every 10 days. I throw out bottles at 28 days. I don’t wear contacts. I know the risks.
And yet, here you all are, acting like this is the first time anyone’s ever heard of glaucoma.
Maybe stop treating ophthalmology like a TikTok trend and just… follow the damn protocol?
Also, loteprednol isn’t ‘safer’-it’s just less likely to turn you into a human pressure cooker. But it’s still a steroid. Don’t get cocky.
Hey everyone, I just want to say-this is so important. I’m a type 2 diabetic, and I was on steroid drops after a corneal abrasion. I thought I was fine. Then my pressure hit 32. I panicked.
But my doc didn’t judge me. He just said, ‘Let’s fix this.’ And we did. Now I get checked every 2 weeks. I even set phone reminders.
If you’re scared, you’re not alone. But you’re not powerless. Ask questions. Write them down. Bring them to your next visit.
And if you’re on these drops? You’re not weak. You’re fighting. Just don’t fight alone.
Also, I started using ketorolac after my taper. It’s not magic, but it’s my new best friend. Less scary, still helps.
You got this. Seriously. 💪
Just wanted to say thanks for this. I’ve been on loteprednol for 5 weeks and was about to skip my next tonometry appointment because ‘my eye feels fine.’ Then I read this and realized I was being an idiot.
Got my check today-pressure’s still good. I’m keeping the appointment next week too. Small wins.
Thank you for writing this with such clarity and care. It’s rare to see medical information presented this honestly and accessibly. The distinction between steroid-induced cataracts and age-related ones is critical-so many people don’t realize it’s preventable.
I’ve worked with patients who dismissed early symptoms because they ‘didn’t hurt.’ That’s the tragedy. Vision loss doesn’t announce itself with a scream-it whispers until it’s too late.
Please, if you’re reading this and on steroid drops: schedule your tonometry. Write down your symptoms. Ask for a visual field test. You are your own best advocate.
And if you’re a provider-thank you for not cutting corners. This is the kind of care that saves lives.
So… we’re told to use steroids but warned they’re dangerous… so what’s the real truth? Is life just a series of controlled risks? Are we all just lab rats in a giant pharmaceutical experiment? I mean, if you think about it, everything we do is a gamble. Breathing, eating, driving…
But eye drops? That’s different. That’s your soul peeking out through your pupils. And they’re telling you to trust them? Hah.
Maybe the real cure is not using them at all. Maybe the body knows better than the lab.
…or maybe I’m just overthinking it. Probably.
This article is dangerously misleading. The FDA has known since 1998 that steroid eye drops are linked to optic nerve atrophy. Why are they still on the market? Who benefits? Why aren’t you being told about the class-action lawsuits? Why is your doctor not warning you about the hidden data?
And why is everyone so eager to follow medical advice without questioning the source? You’re being manipulated. This isn’t healthcare. It’s control.
Stop taking these. Go to a holistic optometrist. Try acupuncture. Or better yet-pray.
Okay, so I read this whole thing and… I’m kinda proud of myself for not throwing my drops in the trash.
I was on prednisolone for 3 weeks. Thought I was fine. Then I saw ‘steroid responders’ and thought, ‘oh crap, that’s me.’
Called my doc. Got my pressure checked. It was 22. Normal.
But I’m still getting checked every 2 weeks. Because I’m not taking chances.
Also, I threw out my bottle after 28 days. Even though it had 3 drops left. I’m not a hero. I’m just not blind.
Thanks for the nudge, OP. I needed it.
Let’s be real-steroid drops are the medical equivalent of a sugar rush. You feel amazing for a few days, then your body starts screaming. And no one tells you until it’s too late.
I used them after laser surgery. Thought I was golden. Then I started seeing halos. Thought it was my contacts. Then my vision went foggy. Turned out: steroid cataracts. Surgery at 39.
My surgeon said, ‘You’re lucky it didn’t get worse.’ Lucky? I had to get my lens replaced because I trusted a doctor who said ‘it’s fine.’
Don’t be me. Don’t wait until you’re seeing double to act.
Too long. Don’t care.
Powerful tools. Silent destroyers. The body remembers. The eye does not speak. You must listen.
Imagine your eye is a cathedral. Steroid drops are the architects. They silence the chaos-yes. But they also weaken the pillars. You don’t see the cracks until the ceiling collapses.
And when it does? No one blames the architect. They blame you for not noticing the dust.
Check your pressure. Not because you’re told to. But because your soul is behind your pupils. And it’s begging you to care.
Wait, so you’re telling me I can’t use steroid drops if I’ve had a cold sore? But my cousin used them for months and he’s fine. Also, why do we need tonometry? Can’t we just use a phone app? I saw one on Reddit that claims to measure IOP.
And isn’t loteprednol just a fancy name for the same thing? Marketing. That’s all.
Also, NSAIDs? Those are just anti-inflammatories. Why not just take ibuprofen? Same thing, right?
My eye felt fine. So I stopped the drops. Two days later, it felt worse. Then I read this. I’m back on the taper. Thanks for the wake-up call.