Medication Sexual Side Effects Checker
Check Your Medication Risk
Enter your current medication to see the percentage risk of sexual side effects.
Your Risk Assessment
0%
Important Note: This information is based on clinical studies and should not replace professional medical advice. Always discuss your symptoms with your healthcare provider.
It’s not rare to hear someone say, "I’m taking my pills, but I’m not myself anymore." For many, that change isn’t just about mood or energy-it’s about sex. Sexual side effects from common medications are one of the most under-discussed, yet deeply impactful, consequences of long-term drug use. Whether you’re on antidepressants, blood pressure meds, or even acid reflux pills, your sex life might be quietly affected-and you’re not alone. Up to 73% of people taking SSRIs report sexual problems. That’s more than two out of three. Yet, most never tell their doctor.
Why This Happens (And Why It’s Not Just "In Your Head")
Your brain, hormones, and blood flow all play a role in sexual function. Many medications interfere with one or more of these systems. For example, antidepressants that boost serotonin-like fluoxetine or sertraline-can shut down arousal, delay orgasm, or kill desire entirely. It’s not weakness. It’s chemistry. Beta blockers, used for high blood pressure and heart conditions, reduce blood flow to the genitals. Thiazide diuretics, often prescribed for fluid retention, lower zinc levels, which are critical for testosterone production. Even proton pump inhibitors (PPIs) like omeprazole, taken daily for heartburn, have been linked to lower libido in some users, though the exact mechanism is still being studied. The truth? You don’t need to have a mental health condition to experience this. Even healthy people on routine meds report changes in sexual function. A 2023 study in Australian Prescriber found that 41% of women on antihypertensives lost interest in sex, and 34% felt less pleasure during intimacy. These aren’t side effects you should ignore-they’re signals.Which Medications Are Most Likely to Cause Problems?
Not all drugs affect sex the same way. Some have a higher risk. Here’s what the data shows:Antidepressants: The Biggest Culprits
SSRIs are the most common cause of drug-induced sexual dysfunction. Among them:- Paroxetine (Paxil): 65% risk of sexual side effects
- Fluvoxamine (Luvox): 59%
- Sertraline (Zoloft): 56%
- Fluoxetine (Prozac): 54%
Heart and Blood Pressure Medications
High blood pressure itself can reduce sexual function. But the meds? They make it worse.- Thiazide diuretics (like hydrochlorothiazide): Most common cause of erectile dysfunction among antihypertensives
- Beta blockers (like atenolol): Reduce blood flow and lower testosterone
- Spironolactone and digoxin: Linked to low libido and erectile issues in heart failure patients
Prostate and Hormone Medications
Men taking 5-alpha reductase inhibitors (like finasteride or dutasteride) for enlarged prostates or hair loss face:- 5.9-15.8% chance of lower libido
- 5.1-9.0% chance of erectile dysfunction
- 0.8-21.4% chance of ejaculation problems
Other Surprising Offenders
- Gabapentin and pregabalin (for nerve pain or seizures): Linked to erectile dysfunction via increased sex hormone binding globulin, which lowers free testosterone.
- Opioids (oxycodone, morphine): Bind to brain receptors and shut down the hypothalamic-pituitary-gonadal axis, causing low testosterone and erectile dysfunction.
- H2 blockers and PPIs: Some users report reduced desire, though data is still emerging.
What You Can Do: Practical Steps to Take
You don’t have to suffer in silence. Here’s what works:1. Talk to Your Doctor-Without Shame
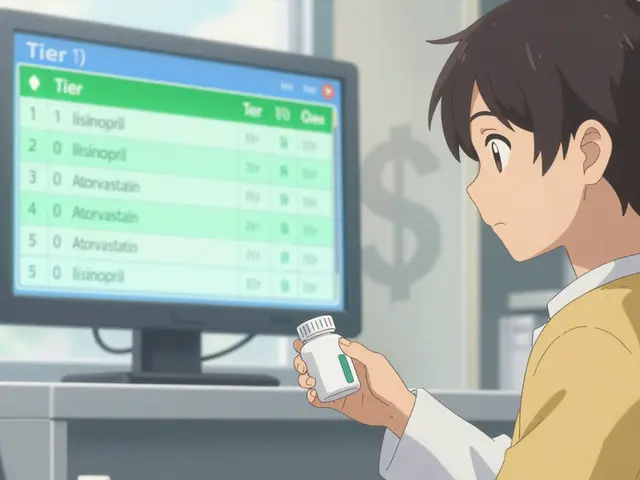
This is the most important step. Many patients avoid bringing it up because they think it’s embarrassing or that their doctor won’t care. That’s false. A 2023 American Urological Association guideline recommends routinely screening for sexual side effects in patients on long-term meds. Say it plainly: "I’ve noticed my sex drive has dropped since I started this med. Is there another option?"2. Consider Switching Medications
Not all drugs in a class are equal. If you’re on paroxetine and struggling, switching to bupropion could improve your sex life without worsening your depression. If you’re on a beta blocker, ask about switching to valsartan or another ARB. For men on finasteride, stopping the drug often reverses sexual side effects within months. But don’t quit cold turkey-work with your doctor.3. Try a "Drug Holiday" (Only With Medical Approval)
Some patients on SSRIs take a short break on weekends-skipping doses Friday night to Sunday morning-to allow sexual function to recover. This isn’t for everyone, and it can trigger withdrawal symptoms. But under supervision, it’s helped many.4. Add a Medication to Fix the Side Effect
Sometimes, the fix is another pill. For SSRI-induced erectile dysfunction, adding sildenafil (Viagra) works in 74-95% of cases. Tadalafil (Cialis) is another option. This isn’t a band-aid-it’s a valid treatment strategy.5. Lifestyle Changes That Help
Exercise isn’t just good for your heart-it helps your sex life. Regular physical activity boosts blood flow, improves mood, and increases testosterone. Even 30 minutes of brisk walking five days a week can make a difference. Sleep matters too. Low testosterone often links to poor sleep. Stress management and reducing alcohol can also help.When It’s Not the Medication
It’s easy to blame the pill. But sometimes, the problem is deeper. Up to 70% of people with depression already have sexual dysfunction before starting meds. Same with schizophrenia-30-80% of patients report sexual issues regardless of drugs. If your libido dropped after starting a new med, it’s likely related. But if it’s been months and you’ve switched meds with no improvement, it might be the condition itself-or something else: low testosterone, thyroid issues, or even relationship stress. A simple blood test for testosterone, thyroid, and prolactin can rule out other causes.


i literally thought i was broken until i read this. took sertraline for 3 years and just assumed my lack of interest was me being "adulting too hard". turned out it was the pill. switched to wellbutrin and suddenly i want to touch my partner again. also my skin cleared up. weird side bonus.
so meds kill sex. shocker. next you’ll tell me sugar makes you fat.
This is an exceptionally well-researched and clinically relevant overview. The inclusion of specific percentages and drug comparisons elevates it beyond typical patient forums. I appreciate the emphasis on actionable alternatives rather than alarmism.
have you ever felt like your body is a rented apartment and the landlord keeps changing the locks? i took fluoxetine for anxiety and suddenly i couldn’t feel anything-not joy, not touch, not the warmth of my partner’s hand. it wasn’t depression, it was chemical amnesia. i cried for three days after stopping it because i forgot what pleasure felt like. and no one warned me. not the doctor, not the pamphlet, not the damn app that told me to "take one daily and feel better."
THIS. THIS IS SO IMPORTANT. i’m a nurse and i see this every week. patients nodding along like it’s normal to lose their sex drive. no it’s not. it’s a side effect and you deserve better. tell your doc. bring this article. they’ll thank you later.
take viagra to fix your ssri? brilliant. next you’ll prescribe caffeine to fix your diabetes.
That’s a really good point, and I think it’s worth noting that while sildenafil can help with function, it doesn’t always restore desire-which is often the deeper issue. The body might respond, but the mind still feels numb. That’s why switching meds or adding therapy sometimes works better than just adding another pill.
oh sweet mercy, i took omeprazole for years thinking it was just "heartburn"-turns out i was also slowly turning into a human who didn’t care if their partner touched them. now i drink apple cider vinegar like it’s my job. and yes, i still miss the days when i could get hard without a script.
Thank you for sharing this with such care. Many of us in other countries don’t have access to these options, but knowing this exists helps us advocate for better care. I’ve seen women in my community suffer silently-this could change that.
Ah, the modern condition: pharmaceutical ennui. We pharmacologically optimize our neurochemistry, only to realize we’ve optimized away the very thing that gives meaning to existence-desire, the spark, the erotic friction of being alive. We are not merely bodies with receptors-we are mythic creatures who once worshipped the body as temple. Now we take a pill to fix the temple… and then another pill to fix the temple’s inability to worship.