Every year, over 1.5 million people in the U.S. are harmed by mistakes in their prescriptions. Many of these errors happen before the medicine even leaves the doctor’s office. You might think your doctor or pharmacist catches everything-but that’s not always true. The truth is, prescription writing errors are more common than you think, and you have more power to stop them than you realize.
What Are Prescription Writing Errors?
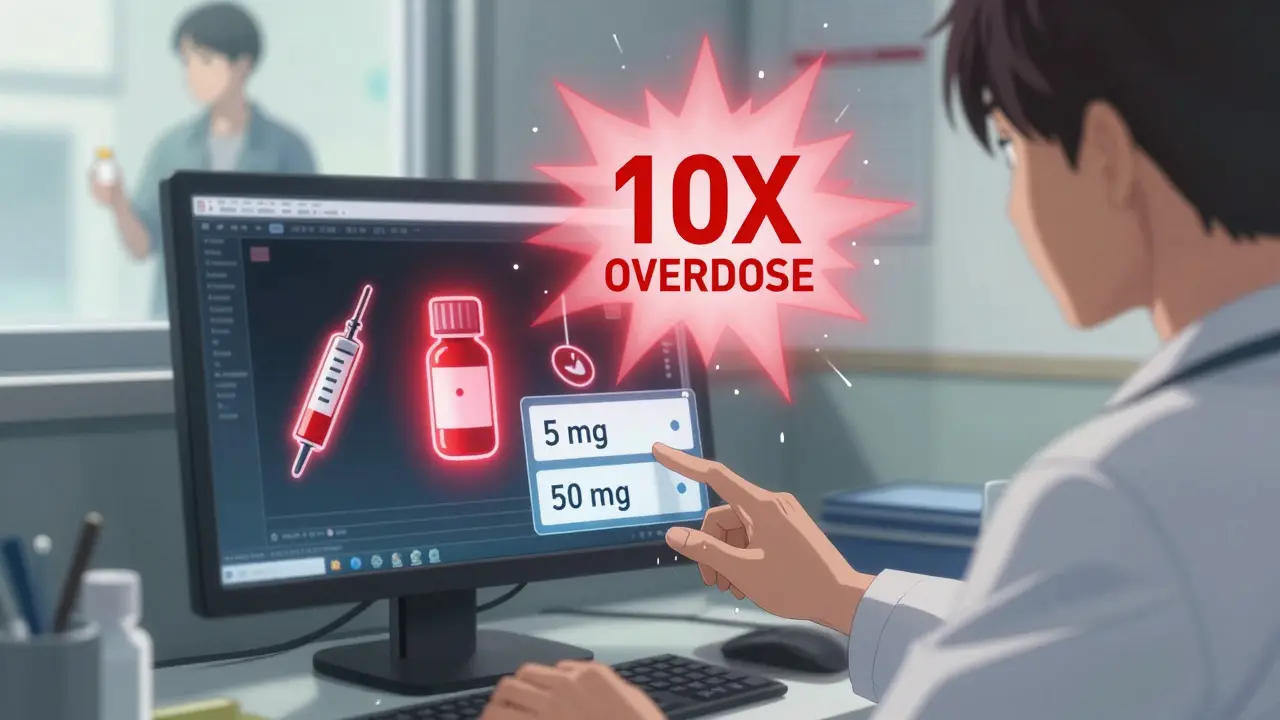
Prescription writing errors are mistakes made when a provider writes or enters a medication order. These aren’t pharmacy mistakes. They’re errors in the original order-wrong drug, wrong dose, wrong instructions. The most dangerous ones involve high-alert drugs like insulin, blood thinners, and opioids. A simple typo can turn a safe dose into a deadly one.Take the example of a decimal point. If a doctor writes ".5 mg" without the leading zero, a pharmacist might read it as "5 mg"-ten times the intended dose. The FDA says these kinds of errors caused 128 deaths between 2010 and 2020. Or consider "U" for units. That’s often mistaken for "0," leading to a tenfold overdose. That’s why experts now say: never write "U." Always spell out "units."
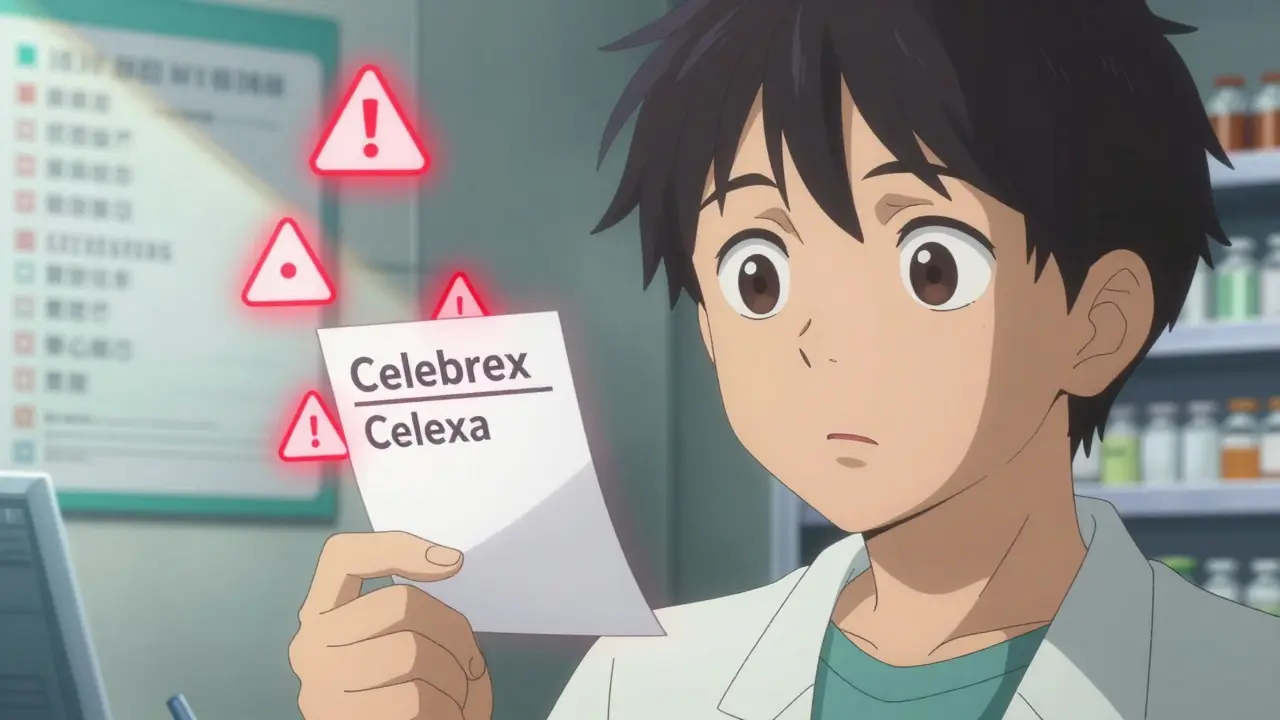
Another big issue is look-alike, sound-alike drug names. Celebrex and Celexa. Zyprexa and Zyrtec. They sound almost the same. A quick slip in typing or handwriting can send you home with the wrong pill. One study found these mix-ups account for 25% of all prescribing errors.
How Common Are These Errors?
You might think electronic prescribing fixed this problem. It helped-but it didn’t solve it. A 2019 study in JAMA Internal Medicine found that while handwriting errors dropped by 55%, e-prescribing created 34% new types of mistakes. Why? Dropdown menus. If you’re rushing and click "50 mg" instead of "5 mg" because it’s right next to it on the screen, you’ve just made a dangerous mistake.Doctors are under pressure. On average, they spend just 17 seconds per prescription in busy clinics. That’s not enough time to double-check everything. A 2022 survey found 68% of primary care doctors make at least one prescribing error every month. Internists average 2.3 errors per month. That’s not negligence-it’s system overload.
And it’s expensive. Medication errors cost the U.S. healthcare system $42 billion a year. Pharmacies now spend nearly 19 minutes per prescription just trying to fix errors that came from the doctor’s office. That’s up from under 7 minutes in 2015.
The 9 Most Common Prescription Errors
Based on analysis of over 12,500 malpractice claims, here are the top nine errors:- Unclear or illegible handwriting (22%)
- Wrong dosage or quantity (19%)
- Prescribing drugs that interact badly (15%)
- Incorrect instructions (e.g., "take once daily" written as "take four times daily") (12%)
- Wrong rate of use (e.g., "take every 6 hours" vs. "take every 12 hours") (9%)
- Wrong diagnosis leading to wrong drug (8%)
- Incorrect drug name (7%)
- Wrong format (e.g., missing expiration date or prescriber info) (5%)
- Missing medication you actually need (3%)
And here’s the kicker: the most frequent type of error overall? Improper dose. That’s 37.8% of all prescribing mistakes. That’s not a small risk. That’s the biggest danger you face.
How to Catch Errors Before You Take the Medicine
You don’t have to wait for a pharmacist to catch a mistake. You can catch it yourself-right when you get the prescription. Here’s how:Check the seven critical elements on every prescription:
- Full drug name-No abbreviations. "Lamotrigine," not "Lamictal." "Metformin," not "Glucophage."
- Precise dosage-Look for leading zeros. "0.5 mg," not ".5 mg." No trailing zeros. "5 mg," not "5.0 mg."
- Clear frequency-Avoid "QD," "BID," "TID." They’re outdated and confusing. It should say "once daily," "twice daily," etc.
- Total quantity-If you’re taking a pill once a day for 30 days, you should get 30 pills. If you get 100, ask why.
- Purpose-The prescription should say why you’re taking it. "For high blood pressure," not just "Take one daily."
- Prescriber info-Full name, phone number, NPI number. If it’s missing, the prescription isn’t valid.
- Expiration date-Prescriptions expire. If it’s older than a year, don’t fill it.
Use this checklist every single time. A 2022 University of Michigan study showed patients who used it caught 63% of errors before even getting to the pharmacy. Without it, only 22% caught anything.
Red Flags You Must Never Ignore
Some mistakes are easy to spot if you know what to look for:- "U" for units → Always spell out "units."
- "MS" or "MSO4" → Could mean morphine sulfate or magnesium sulfate. One kills, the other treats seizures. Ask which one it is.
- "HC" for hydrocortisone → Could be mistaken for heparin (a blood thinner). That’s a deadly mix-up.
- "QD" or "QID" → These abbreviations are banned for good reason. Replace them with "daily" or "four times daily."
- High-alert drugs → Insulin, warfarin, morphine, heparin. If you’re on one, double-check everything. Even small mistakes can kill.
Use the Institute for Safe Medication Practices list of error-prone drug pairs. If your drug is on it, be extra careful.
Use the Teach-Back Method
When the doctor or nurse explains how to take your medicine, don’t just nod. Repeat it back in your own words. "So you’re saying I take one pill every morning with food, not at night?" This is called the teach-back method. Johns Hopkins found it reduces misunderstandings by 81%.Don’t be shy. Say: "I want to make sure I got this right. Can I repeat it back to you?" Most providers will appreciate it. They’ve seen what happens when patients don’t understand.
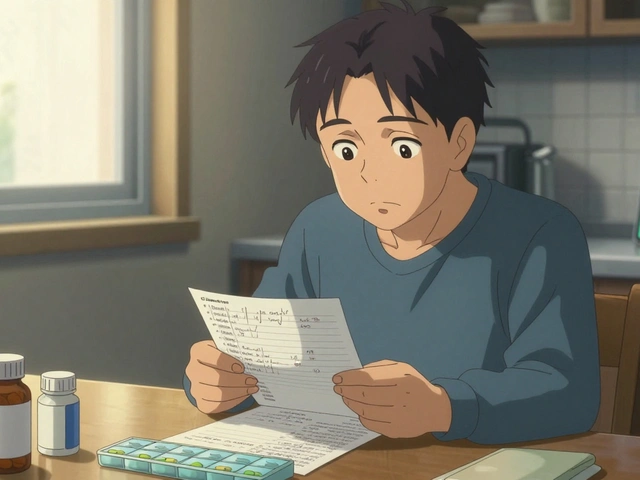
Verify Electronic Prescriptions
If your doctor sends your prescription electronically, you still need to check. When you get to the pharmacy, compare the label to what you were told. Is the name right? The dose? The instructions?For example: If you have diabetes and your prescription says "insulin," but the label says "amlodipine" (a blood pressure drug), stop. Don’t take it. Call your doctor’s office immediately.
Ask the "Ask Me 3" Questions
The National Patient Safety Foundation created a simple three-question rule:- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
Ask these at every visit. A 2021 study in JAMA Network Open found patients who asked these questions reduced medication errors by 44%.
Use Technology to Your Advantage
There are apps now that scan your prescription and check for errors. One called MedSafety has been used by over 2 million people. In a 2023 pilot study, it caught 68% of errors patients missed on their own.Also, if your provider uses an online portal, check your prescription there before you go to the pharmacy. Many systems now let you see your e-prescription details before it’s sent. If something looks wrong, message your doctor right away.
Starting in 2025, all electronic health records will be required to give patients real-time access to their prescription data through secure apps. That means you’ll be able to see exactly what was sent-before the pharmacy even gets it.
What If You Spot an Error?
Don’t panic. Don’t argue. Just say:"I think there might be a mistake. Can we double-check this?"
Pharmacists are trained to catch errors. They’ll thank you. In fact, they’re now spending almost 20 minutes per prescription just fixing prescriber mistakes. You’re helping them do their job.
If the pharmacy says it’s correct but you still feel off, call your doctor’s office. Ask for the original prescription to be reviewed. Most offices have a nurse or pharmacist on staff who can verify it.
Why This Matters More Than You Think
Prescription errors are the most preventable type of medical mistake. Yet, since 2000, we’ve only reduced them by 15%. That’s not progress. That’s failure.You’re not just a passive recipient of care. You’re the last line of defense. When you check your prescription, you’re not being difficult. You’re saving your life.
And you’re not alone. Programs like "Script Check" in 37 states train volunteers to help elderly patients verify prescriptions. In its first year, it found over 8,000 dangerous errors.
The future of medication safety isn’t just better technology. It’s empowered patients. By 2027, experts predict patient-led error detection will cut prescribing mistakes by 60%. That’s not science fiction. It’s the next step.
Final Checklist: Your Prescription Safety Plan
Before you leave the office or pick up your meds, ask yourself:- Is the drug name spelled out fully, with no abbreviations?
- Is the dose written with a leading zero (0.5 mg), not a trailing one (5.0 mg)?
- Are instructions in plain language ("twice daily")?
- Is the quantity right for how long I’m supposed to take it?
- Does it say why I’m taking this?
- Does the prescriber’s info look complete?
- Is this a high-alert drug? If yes, did I double-check everything?
- Did I use the teach-back method to confirm instructions?
If you answered yes to all eight, you’ve done more than most people ever do. You’ve taken control. And that’s how you stop a mistake before it hurts you.
Can I get a copy of my prescription before going to the pharmacy?
Yes. If your provider uses an electronic health record system, you can usually access your prescription through their patient portal. Many systems now let you view the exact medication, dose, and instructions before it’s sent to the pharmacy. If you don’t have access, ask your doctor’s office to email or print a copy for you.
What should I do if the pharmacy says my prescription is correct but I still feel unsure?
Call your doctor’s office directly. Ask to speak with the nurse or pharmacist who handles prescriptions. Say: "I’m concerned about this prescription. Can you confirm the medication, dose, and instructions match what you intended?" Most offices will verify it immediately. Don’t wait to take the medicine until you’re certain.
Are handwritten prescriptions still common?
They’re rare now-less than 5% of prescriptions are handwritten. But they still happen, especially in urgent care or rural clinics. Always check for illegible writing, unclear numbers, or abbreviations like "U" or "QD." If you can’t read it, don’t take it. Ask for a typed copy.
Do all pharmacies check prescriptions for errors?
Pharmacists are trained to catch errors, and they do check every prescription. But they’re not mind readers. If your doctor wrote "0.5 mg" as ".5 mg," the pharmacist might miss it. That’s why your review is so important. You’re the only person who knows your body and your history.
Can I report a prescription error?
Yes. You can report it to the FDA’s MedWatch program or to the Institute for Safe Medication Practices (ISMP). Even if no harm was done, reporting helps improve systems. Your report could prevent someone else from being hurt.



This post saved my life last year. I caught a 10x insulin dose error because I noticed the missing zero. I didn't know what to look for until I read this. Now I check every script like it's a bomb detonator. Everyone should print this out and tape it to their fridge.
Doctors are drowning in paperwork and time pressure. I get it. But this is why we need better systems not just patient vigilance. I've seen my dad nearly die from a typo. We need tech that auto-checks high-alert meds before the script even leaves the computer. Not more checklists for exhausted people.
Big Pharma and EHR companies are in cahoots. They want you to check your own scripts so they don't have to fix broken software. They profit from errors because it keeps you coming back. The FDA knows this. They just don't care. Your life is a revenue stream.
It is not merely inconvenient-it is a systemic failure of American medical infrastructure. The fact that a citizen must become a pharmacologist to avoid lethal misadministration speaks volumes about the decay of professional standards. This is not a patient problem. This is a national disgrace. We have outsourced competence to the public. This is not empowerment. This is abandonment.
In India, we still have handwritten scripts sometimes-but we also have community health workers who sit with elders and read the labels aloud. No tech needed. Just human connection. Maybe the solution isn't more apps but more people trained to care enough to double-check. I’ve seen my aunt survive a warfarin mix-up because her neighbor asked, ‘Why is this blue pill here?’ Simple. Powerful. Human.
Let’s be honest: if you can’t spell ‘metformin’ correctly, you shouldn’t be prescribing. And if you think ‘QD’ is acceptable, you’re not a doctor-you’re a liability with a medical degree. I’m not being harsh. I’m being accurate. This isn’t about being ‘difficult.’ It’s about demanding the baseline competence that should be non-negotiable.
You got this. Don’t let anyone make you feel weird for asking questions. I used to feel guilty for double-checking-until my sister ended up in the ER because the pharmacy gave her the wrong antibiotic. Now I say, ‘I’m not being difficult. I’m being alive.’ And I’ve saved three people so far. You’re not annoying. You’re essential.
You're not safe. Not even close.