Scar Management Plan Calculator
Create Your Personalized Scar Management Plan
Your Personalized Scar Management Plan
Recommended Techniques
Note: Consult with your physical therapist before starting any new scar management techniques.
Treatment Schedule
Special Considerations
When a wound closes, the body doesn’t just stitch the skin back together - it builds a patch of Scar Tissue is fibrous tissue that replaces normal skin after an injury, often appearing raised, discolored, or less flexible. Left unattended, that patch can tighten, restrict movement, or turn into an unsightly keloid. This is where physical therapy scar healing steps in, using movement, pressure, and targeted manual techniques to guide the tissue toward a smoother, more functional outcome.
How scar tissue forms and why it matters
After the skin’s outer layer repairs, fibroblasts lay down collagen to give the wound strength. The first collagen fibers are laid down in a random, haphazard pattern. Over weeks to months, the body remodels this matrix, aligning fibers along lines of tension. If the remodeling process is interrupted - by immobility, poor circulation, or excessive tension - the scar can become thick, raised, and painful.
Two common types of excessive scarring are:
- Hypertrophic Scar is a raised, red scar that stays within the boundaries of the original wound and may improve over time.
- Keloid is a firm, often itchy growth that extends beyond the wound edges and rarely regresses without intervention.
Why physical therapy matters for scar management
Physical therapy (PT) isn’t just for back pain or sports injuries; it’s a science‑based approach to tissue health. PT addresses three key factors that drive scar problems:
- Mobility: Gentle movement keeps collagen fibers oriented correctly, preventing the “tight rope” effect.
- Blood flow: Manual techniques and active exercises boost circulation, delivering nutrients and clearing metabolic waste.
- Mechanical stress: Controlled pressure and stretch signal fibroblasts to produce a more organized collagen matrix.
When these elements are combined, the scar remodels faster, becomes softer, and is less likely to turn into a keloid.
Core PT techniques for scar management
Below are the most evidence‑backed interventions that PTs use. Each technique has a clear goal and a typical frequency.
- Myofascial Release is a hands‑on method that applies sustained pressure to fascia to release restrictions and improve tissue glide. 2‑3 sessions per week for the first month, then weekly maintenance.
- Massage Therapy is a soft‑tissue technique that uses rhythmic strokes to increase perfusion and break down adhesions. Ideal for larger surface‑area scars; 10‑15 minute sessions daily at home.
- Range of Motion (ROM) Exercises is active joint movements that stretch the surrounding skin and connective tissue. Perform 5-10 repetitions, 3-4 times daily.
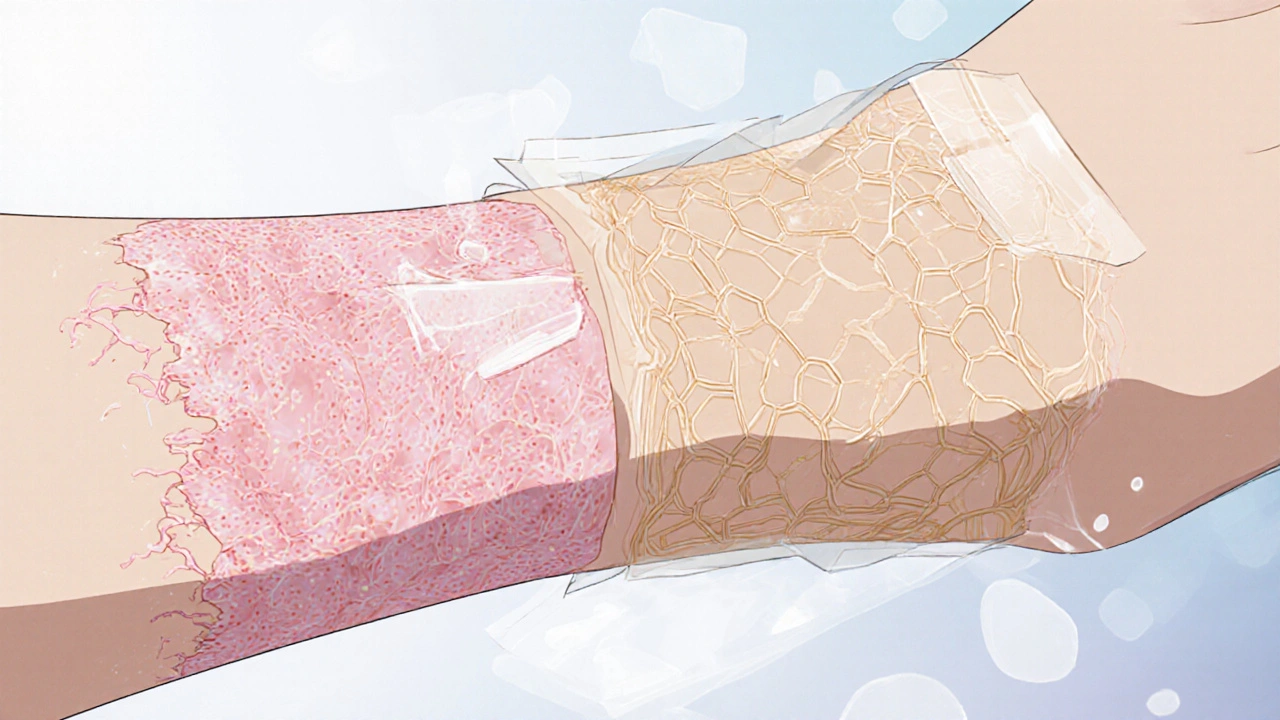
- Compression Therapy is the use of elastic garments or specialized silicone sheets to apply constant, low‑level pressure. Wear 12-24 hours a day for 2-6 months, depending on scar severity.
- Scar Massage with Silicone Gel is a hybrid approach that combines manual massage with the occlusive benefits of silicone. Apply silicone gel for 20‑30 minutes, then massage for 5 minutes.

Integrating PT with other scar‑care modalities
Physical therapy works best when paired with dermatologic treatments. A typical multimodal plan looks like this:
| Modality | Purpose | Timing |
|---|---|---|
| Physical Therapy (ROM, Myofascial Release) | Align collagen, improve flexibility | Start within 1‑2 weeks post‑closure |
| Silicone Gel or Sheet | Hydrate scar, reduce height | 24‑48 h after wound closure, continue 3‑6 months |
| Laser Therapy (optional) | Depigment, soften tissue | After 3 months if scar persists |
| Massage Therapy | Increase perfusion, break adhesions | Weekly for 4‑6 weeks, then as needed |
Coordinating these steps prevents overlap-e.g., you wouldn’t apply a compression garment during a vigorous ROM session because it limits stretch.
Creating a personalized scar rehab plan
Every scar is unique. Here’s a quick checklist PTs use to tailor treatment:
- Location & depth: Is the scar over a joint, muscle, or superficial skin?
- Age of scar: Acute (≤6 weeks), early remodeling (6 weeks‑6 months), mature (>6 months).
- Skin type & tendency: Darker skin tones have higher keloid risk; adjust pressure levels accordingly.
- Functional impact: Does the scar limit range of motion, cause pain, or affect daily activities?
- Patient goals: Cosmetic appearance vs. functional mobility - prioritize techniques that match the goal.
Based on the answers, a PT might schedule daily ROM, twice‑weekly myofascial release, and prescribe a custom compression sleeve worn overnight.
Common pitfalls and how to avoid them
Even with the best plan, mistakes can set back progress:
- Too much force: Aggressive stretching can tear fresh tissue. Start with light tension and increase gradually.
- Inconsistent practice: Scar remodeling is a weeks‑long process; missing daily ROM or compression reduces benefits.
- Ignoring skin health: Dry, cracked skin hampers massage. Keep the area moisturized with hypoallergenic creams.
- Wrong timing: Beginning high‑pressure compression before the wound is fully epithelialized can cause maceration.
Regular follow‑ups with your therapist let you tweak intensity before problems arise.
Quick reference: Scar‑Healing Checklist
- Start gentle ROM within 7‑10 days of wound closure.
- Schedule myofascial release 2-3 times weekly for the first month.
- Apply silicone gel or sheet for at least 12 hours daily, extending to 24 hours as tolerated.
- Massage the scar for 5 minutes after silicone application.
- Re‑evaluate scar height, color, and flexibility every 4 weeks.
Frequently Asked Questions
When should I begin physical therapy after a surgery?
Most surgeons clear patients for gentle ROM and scar‑focused PT as soon as the incision is closed and the dressing is removed, usually within a week. The exact start date depends on wound tension and any post‑op restrictions.
Can I do scar massage at home?
Yes. Use a hypoallergenic oil or silicone gel, apply gentle pressure in circular motions for 5‑10 minutes, twice a day. Avoid deep pressure on fresh wounds.
Is compression therapy necessary for every scar?
Compression is most helpful for large, hypertrophic, or keloid‑prone scars, especially on the torso or extremities. Small linear scars usually heal fine with ROM and massage alone.
What if my scar becomes painful during therapy?
Pain signals that the tissue may be overstressed. Reduce stretch intensity, switch to a gentler technique (e.g., light massage), and check with your therapist for possible underlying inflammation.
Can physical therapy prevent keloids entirely?
It can dramatically lower the risk by controlling tension and promoting proper collagen remodeling, but genetics still play a role. Combining PT with silicone compression offers the best protection.


Physical therapy isn’t just about fixing a torn hamstring; it’s a philosophy of movement that can rewrite the story a scar tells. When we treat a wound as a living tissue that still wants to move, we’re giving it permission to heal on its own terms. Gentle ROM within the first week keeps collagen fibers from locking into a random mess. My experience with post‑surgical patients shows that even five minutes of mindful stretch each day can mean the difference between a flexible line and a restrictive band. Think of the scar as a rope that needs regular tension checks, not a permanent fence.
Totally agree, I’ve seen that early mobility can prevent that ‘tight rope’ feeling you mentioned. I usually start patients on light pendulum swings before the incision is fully closed, which feels safe and still engages the tissue. The key is listening to pain signals and scaling back intensity as needed. Consistency beats intensity any day.
Picture a scar as a scarred battlefield, where collagen soldiers march in chaotic rows, unaware of the harmony they could achieve. The moment you introduce a skilled physical therapist into this arena, the chaos begins to dissolve into disciplined formation. Each myofascial release is a diplomatic treaty, coaxing stubborn fibers to surrender their rigidity. The rhythmic massage acts like a gentle rain, washing away the debris of inflammation that clouds the healing horizon. Compression sleeves become silent sentinels, applying just enough pressure to remind the tissue of its boundaries without crushing its spirit. Range of motion exercises are the marching orders, commanding the scar to move, stretch, and adapt rather than remain static and hostile. When patients obey these commands daily, the scar’s appearance transforms from a raised, angry hillock into a sleek, compliant ridge. Scientific studies have shown that properly timed mechanical stress can down‑regulate fibroblast overactivity, curbing the dreaded keloid surge. Yet the true miracle lies not only in numbers but in the patient’s belief that their body is capable of rewriting its own narrative. The synergy between silicone sheets and manual therapy creates a micro‑environment that locks in moisture while the therapist’s hands sculpt the collagen architecture. Even the smallest gesture- a five‑minute circular massage- sends signals that echo through the extracellular matrix, telling it to calm down. Over weeks, the scar loses its fiery hue, its texture softens, and movement returns with a subtle confidence. In the grand theater of rehabilitation, every session is a scene where the protagonist- the patient- reclaims agency over their own skin. Ultimately, the scar becomes a badge of resilience rather than a mark of defeat. So, when you see a smoother line where there once was a stubborn knot, remember it is the result of disciplined movement and patient perseverance.
Your description captures the drama beautifully, but let me add a practical framework. First, schedule myofascial release twice per week for the initial four weeks, then taper to weekly maintenance. Second, integrate silicone compression for at least twelve hours daily once the epithelium is intact. Third, prescribe ROM sets of five repetitions, three times per day, focusing on the axis of greatest tension. Finally, reassess scar height and pliability every four weeks to adjust the regimen.
Consistency is the hidden catalyst behind every successful scar‑rehab program. When patients commit to a twice‑daily massage routine, the collagen matrix begins to align like a well‑ordered library. Pair that habit with a silicone sheet worn overnight, and you create a moist environment that softens the tissue. I always tell my clients to log each session; the data acts as a motivation booster. Over time the scar not only looks flatter, it feels more pliable during daily activities.
lol this scar stuff is actually kinda cool 😆
yeah it is! keep it up and dont forget the silicone at night
Think of scar management as a team sport, where you, the therapist, and the skin all have roles. A supportive coach encourages you to set realistic milestones, like three weeks of daily ROM before adding compression. Emphasize proper hydration of the skin; a dry surface resists smooth remodeling. Celebrate small wins, such as reduced redness after the first month. This mindset turns the rehab journey into a positive growth experience.
While your pep talk sounds nice, many patients skip the compression because it feels restrictive and you ignore that reality. A coach should address real barriers, not just hand out feel‑good slogans. If the garment is uncomfortable, modify the material or wear schedule instead of insisting on 24‑hour use. Evidence shows adherence drops dramatically when protocols are too rigid. So, balance motivation with practical flexibility.
As we watch the scar soften, it reminds us that the body is capable of quiet miracles. Each gentle stretch is a silent promise that the tissue will regain its grace. The journey may be slow, but patience yields a smoother line and less discomfort. Keep the focus on progress, not perfection. Together we celebrate each subtle improvement.
Some manufacturers hide the truth about compression garments, claiming they’re harmless while they actually limit blood flow if worn too long. The same companies that sell silicone sheets also push expensive laser treatments that have questionable efficacy. Independent studies suggest a simple home‑made silicone wrap can be just as effective as pricey alternatives. Don’t let big‑brand hype dictate your scar plan; trust the science that’s openly published. Remember, every extra device adds another layer of cost and complexity. The safest approach is often the most straightforward one.
yeah man, keep it simple and let the scar do its thing. i’ve used a cheap silicone sheet and some daily stretches and it’s worked fine for me. no need to splurge on fancy gear. just stay consistent and listen to your body.