Every year, thousands of patients in Australia and around the world are harmed by medication errors - wrong dose, wrong drug, wrong patient. These aren’t rare mistakes. They happen in busy pharmacies, under time pressure, with tired staff, and complex prescriptions. The good news? pharmacy workflow systems are changing that. They’re not just fancy machines. They’re smart, layered safety nets built to catch errors before they reach the patient.
How Medication Errors Happen in Pharmacies
It starts with a prescription. Maybe it’s handwritten and hard to read. Maybe it’s electronic but missing critical details. The pharmacist reads it, checks the patient’s history, picks the right bottle, counts the pills, labels it, and hands it off. At each step, something can go wrong.A pharmacist might confuse similar-looking drugs like hydralazine and hydroxyzine. A technician might miscount 60 tablets as 50. A barcode might scan correctly, but the wrong patient’s name is on the label. All of these are real, documented errors. The Institute of Medicine found that in the U.S. alone, medication errors cause between 44,000 and 98,000 preventable deaths every year. Australia doesn’t track this exactly the same way, but studies show similar rates of dispensing errors in community and hospital pharmacies.
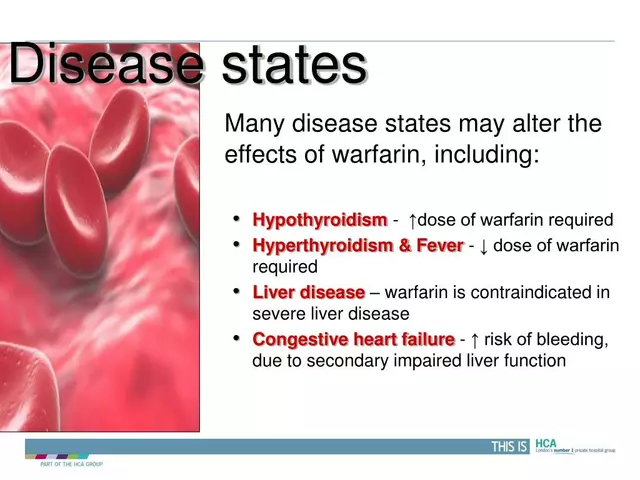
These aren’t always about carelessness. They’re about complexity. A single patient might be on 12 different medications. One drug interacts with another. A kidney patient needs a lower dose. An allergy isn’t flagged in the system. Humans are great at problem-solving - but not at doing the same repetitive, high-stakes task hundreds of times a day without missing something.
What Pharmacy Workflow Systems Actually Do
Pharmacy workflow systems aren’t just one tool. They’re a chain of connected technologies that guide every step of the medication journey - from when the prescription arrives to when the patient walks out.Here’s how it works in a modern pharmacy:
- Electronic prescription intake - Prescriptions come in digitally from GPs or hospitals, eliminating handwriting errors.
- Automated screening - The system checks for drug interactions, allergies, duplicate therapy, and incorrect dosing based on patient age, weight, and kidney/liver function.
- Barcode verification - Every bottle, vial, and pill pack is scanned. The system compares the physical item to the digital order. If it doesn’t match, it stops.
- Robot-assisted dispensing - In hospitals and large pharmacies, robots pull pills from high-capacity bins, count them precisely, and load them into blister packs or bottles. No human fingers touch the medication.
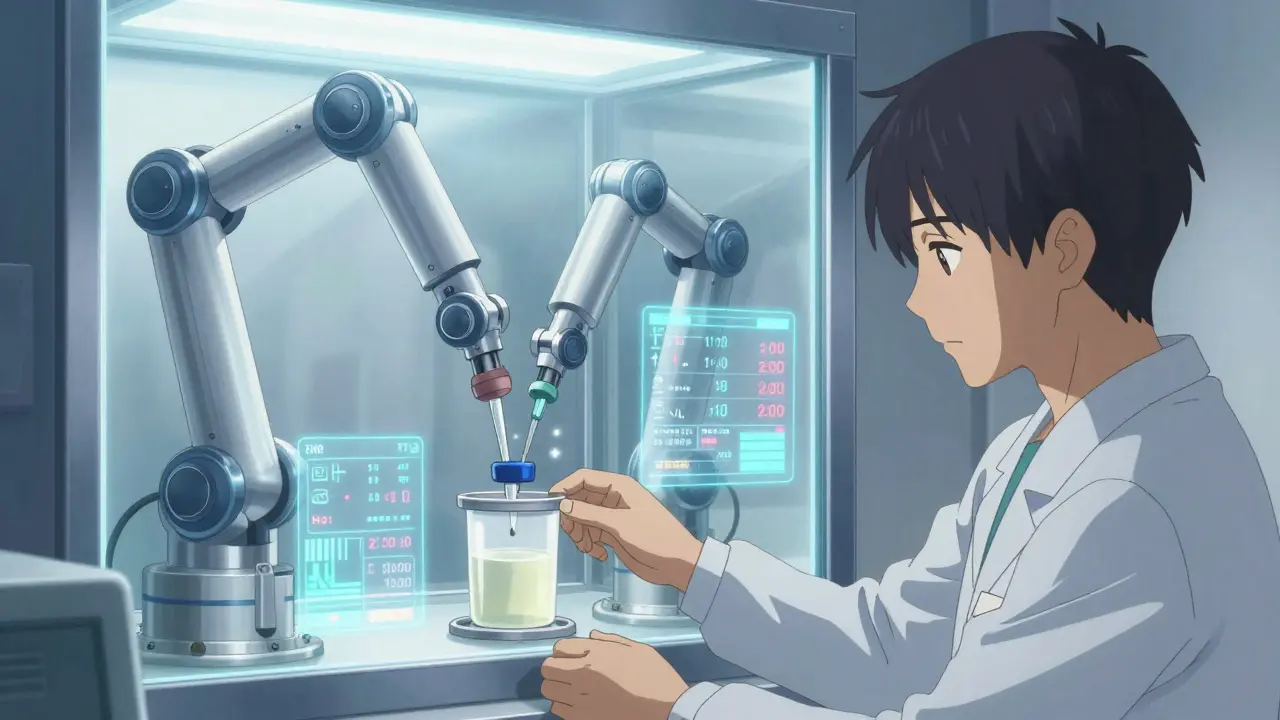
- IV compounding automation - For intravenous drugs, robotic arms measure and mix sterile solutions with milligram accuracy, reducing contamination and dosing errors.
- Real-time inventory tracking - The system knows exactly how many tablets are left, when they expire, and automatically flags shortages before they become a problem.
- Integration with EHRs - The pharmacy system talks to the hospital’s electronic health record. If the doctor changes a prescription, the pharmacy gets the update instantly.
This isn’t science fiction. It’s happening in Sydney hospitals right now. Systems like BD Pyxis™ and Wolters Kluwer’s Simplifi+ IV are used daily in major health networks. The goal isn’t to replace pharmacists - it’s to free them from counting pills and chasing down expired stock so they can focus on patient counseling and complex cases.
Key Technologies Behind the Workflow
There are three core technologies making this possible:- Barcode scanning - Every medication has a unique barcode. Scanning it at every step creates a digital audit trail. If the wrong drug is picked, the system alerts the pharmacist immediately. Studies show barcode systems catch 14 times more errors than manual checks.
- Robotics - Automated dispensing machines and IV compounding robots don’t get tired. They don’t miscount. They follow the same exact steps every time. In IV rooms, these robots reduce preparation time by up to 50% and cut contamination risks by 90%.
- Interoperability - The system doesn’t work in a bubble. It connects to the hospital’s electronic medical record (EMR) via HL7 protocols. That means when a patient’s lab results change, the pharmacy system automatically adjusts dosing recommendations. It also pulls in allergy histories, past prescriptions, and even insurance status.
These systems are built on secure, HIPAA-compliant cloud platforms with 99.9% uptime. They’re not cheap - enterprise systems cost between $50,000 and $250,000 a year - but the cost of a single error can be far higher: legal fees, patient harm, lost trust, and regulatory fines.
How These Systems Prevent Specific Errors
Let’s look at real error types and how workflow systems stop them:| Error Type | How the System Prevents It |
|---|---|
| Wrong drug | Barcode scan matches physical item to digital order. If it doesn’t match, the system locks and sounds an alarm. |
| Wrong dose | Automated alerts flag doses outside safe ranges based on patient weight, age, or kidney function. |
| Wrong patient | Scanning patient ID wristband at pickup confirms identity before dispensing. |
| Drug interaction | System cross-references all current meds and flags dangerous combinations (e.g., warfarin and NSAIDs). |
| Expired medication | Inventory system auto-flags items nearing expiry and prevents them from being selected. |
| Missing allergy alert | System pulls allergy data from EHR and blocks dispensing if conflict exists. |
| IV contamination | Robotic compounding happens in sterile, HEPA-filtered environments with no human touch. |
These aren’t theoretical. A 2023 study at a Sydney hospital showed a 72% drop in dispensing errors after implementing a full workflow system with barcode scanning and robotic dispensing. The same hospital saw a 40% reduction in patient complaints about medication confusion.
Challenges and Real-World Limitations
No system is perfect. Even the best pharmacy workflow tools have hurdles:- Cost - Small independent pharmacies can’t afford $200,000 systems. Some use scaled-down versions or shared services.
- Training - Staff need to learn new workflows. Rushing this leads to workarounds - like disabling alarms or skipping scans - which defeat the purpose.
- Integration issues - If the pharmacy system doesn’t talk properly to the hospital’s EHR, data gaps appear. HL7 connectivity is critical but often poorly implemented.
- Alert fatigue - Too many pop-up warnings can make staff ignore them. Smart systems learn over time and reduce false alarms.
- Transition time - Going from paper to digital takes 3 to 6 months. Productivity dips during this time. Staff need support, not just software.
The American Society of Health-System Pharmacists (ASHP) says it clearly: technology alone won’t fix safety. You need culture change. Pharmacists must be involved in designing the workflow. Staff must be trained not just on how to use the system, but why it matters. One hospital in Melbourne saw error rates climb again after a year because staff started bypassing scans to save time. They had to retrain everyone and add random audits.
What the Best Systems Have in Common
The most successful pharmacy workflow systems share three traits:- They’re built by pharmacists - Not IT vendors. The best platforms, like Simplifi+ and Cflow, were designed by frontline pharmacists who know the daily frustrations.
- They’re flexible - One-size-fits-all doesn’t work. A community pharmacy needs different tools than a hospital IV compounding unit.
- They track performance - Top systems include dashboards that show key metrics: average fill time, error rate per 100 scripts, inventory turnover, and patient wait times. You can’t improve what you don’t measure.
For example, Kissflow’s reporting tools let pharmacies see which staff members have the lowest error rates - and why. Maybe they double-check barcodes every time. Maybe they always verify patient ID. Those habits can be shared across the team.

The Future: AI, Predictive Analytics, and Telepharmacy
The next wave of pharmacy workflow tech is smarter:- Predictive inventory - AI analyzes prescription trends to predict when certain drugs will run out - even before the pharmacist notices.
- AI-powered interaction alerts - Instead of generic warnings, systems will say: “This patient is 82, has heart failure, and is on digoxin. Adding this new diuretic increases risk of toxicity by 68%.”
- Telepharmacy integration - Remote pharmacists can review and approve prescriptions for rural clinics in real time, with workflow systems ensuring compliance and documentation.
- Blockchain for supply chain - Tracking medication from manufacturer to patient to prevent counterfeit drugs.
These aren’t distant dreams. Companies like BD and Wolters Kluwer are already testing them. The push is driven by regulation - USP <797> and <800> standards for sterile compounding are getting stricter - and by patient demand for safer care.
What You Should Look For in a System
If you’re a pharmacy owner, manager, or clinician evaluating a workflow system, ask these questions:- Does it integrate with our EHR and billing system? (HL7 is a must.)
- Can it handle our specific needs? (e.g., IV compounding, controlled substances, chronic disease scripts.)
- Is training included? How long does it take to get staff fully proficient?
- What’s the uptime guarantee? Is support available 24/7?
- Can we see real data from other pharmacies using it? (Ask for case studies.)
- Does it reduce, not just report, errors? (Look for metrics on error reduction, not just alerts.)
Don’t be fooled by flashy demos. Ask for a 30-day trial. Watch how it works during your busiest hours. Talk to the technicians who will use it every day.
Final Thought: It’s Not About Technology - It’s About Trust
The goal of pharmacy workflow systems isn’t to make things faster, although they do. It’s not to cut costs, although they save money. It’s to make sure the person walking out of the pharmacy with their prescription doesn’t have to wonder: “Is this right?”When a system catches a mistake before it leaves the counter, it doesn’t just prevent harm. It builds trust. Patients trust that their meds are safe. Pharmacists trust that the system has their back. Hospitals trust that they’re meeting their duty of care.
That’s the real value. Not the robots. Not the barcodes. Not the price tag. It’s knowing that someone - whether human or machine - is watching out for you.
How do pharmacy workflow systems reduce medication errors?
They reduce errors by automating key safety checks: barcode scanning verifies the right drug and dose, electronic alerts flag dangerous interactions or allergies, robotics eliminate human counting mistakes, and integration with patient records ensures dosing is tailored to individual needs. Studies show these systems catch up to 14 times more errors than manual processes.
Are pharmacy workflow systems only for hospitals?
No. While hospitals use advanced systems for IV compounding and robotic dispensing, community pharmacies also benefit from simpler workflow tools. These include electronic prescribing, automated inventory alerts, drug interaction checkers, and barcode verification for dispensing. Even small pharmacies can use cloud-based platforms like Cflow or Kissflow to reduce errors and save time.
How much do pharmacy workflow systems cost?
Costs vary widely. Enterprise hospital systems with robotics and full EHR integration can cost $50,000 to $250,000 per year. Smaller community pharmacy solutions start at $5,000-$20,000 annually. Many vendors offer subscription models with monthly fees. The biggest expense is often training and workflow redesign, not the software itself.
Do these systems replace pharmacists?
No. They free pharmacists from repetitive tasks like counting pills or checking inventory so they can focus on clinical work - reviewing complex prescriptions, counseling patients, managing chronic conditions, and catching subtle errors that machines might miss. Pharmacists remain the final safety check.
What are the biggest challenges in implementing these systems?
The biggest challenges are staff resistance, inadequate training, poor integration with existing systems, and alert fatigue. Many pharmacies fail because they treat it as a tech upgrade, not a process change. Successful implementations involve pharmacists in design, offer hands-on training, and phase in changes gradually over 3-6 months.
Are pharmacy workflow systems compliant with Australian regulations?
Yes, modern systems are designed to meet Australian standards including TGA requirements for medication safety, ASHP guidelines, and privacy laws under the Privacy Act 1988. For sterile compounding, systems must comply with AS/NZS 3678 and align with USP <797> and <800> equivalents. Vendors should provide documentation of compliance.

This is the kind of stuff that makes me proud of healthcare in general. Not flashy, not sexy, but it saves lives every single day.
People think tech is about apps and social media, but real progress is quiet. It's in the barcode scan that stops a mix-up.
Keep going.
Love this so much 🙌 I work in a small clinic and we just got our first barcode system last year. Before? Chaos. After? Honestly? I can breathe again.
Pharmacists deserve better than counting pills at 3am.
You all act like this is new but India's been doing automated dispensing since 2015 with way less budget. Your systems are overpriced and overhyped. We use open source tools and still catch 90% of errors. Stop acting like the US invented safety
The part about alert fatigue is so real. I’ve seen pharmacies turn off alarms just to get through the day.
It’s not the tech’s fault. It’s how we implement it.
Training should be ongoing, not a one-time webinar. And staff need to feel heard when they say the system is broken.
I used to work in a pharmacy where the robot broke every other week. We called it ‘the grumpy bot’.
Still, even with the glitches, it cut our errors in half.
Humans are the weak link. Not because we’re lazy. Because we’re tired.
And tech that lets us rest? That’s the win.
It’s funny how we think progress means more machines. But what really matters is who’s holding the machine accountable.
The system doesn’t care if you skip a scan.
The patient does.
The pharmacist does.
Maybe the real innovation isn’t the barcode or the robot.
It’s remembering that every pill is someone’s hope.
And no algorithm should ever replace that awareness.
Nupur’s right about cost. Small pharmacies can’t afford $200k systems. But here’s the thing - some vendors offer tiered plans now. Like, basic barcode + alerts for $8k/year.
It’s not perfect, but it’s better than nothing.
And honestly? If your pharmacy still uses handwritten scripts in 2025, you’re already behind.
Australia doesn’t even track medication deaths properly. Why are we even talking about this like it’s a success story? This is just PR. Real change needs policy, not robots.