When someone loses a limb, their body doesn’t just lose a part-it loses a sense of that part. Even after the wound heals, many people still feel the limb is there, sometimes painfully. This is phantom limb pain (PLP), and it’s not in your head. It’s in your brain. About 60% to 85% of amputees experience it. For some, it’s a mild tingling. For others, it’s a burning, cramping, or stabbing pain that never goes away. And if it lasts more than six months, it’s unlikely to vanish on its own.
Why Phantom Limb Pain Happens
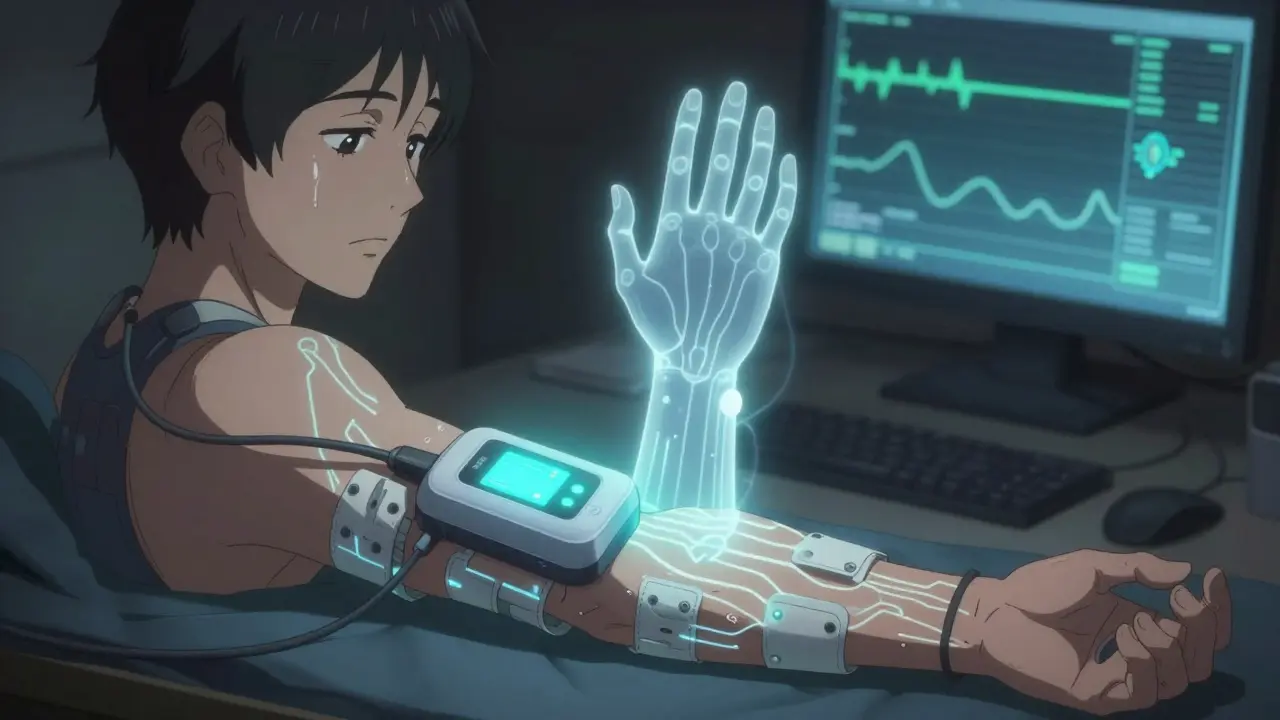
Phantom limb pain isn’t caused by something wrong with the stump. It’s caused by the brain. After an amputation, the nerves that once carried signals from the missing limb don’t just shut off. They keep firing. The brain, still expecting input from that area, misinterprets these signals as pain. Brain scans show that areas once responsible for the amputated limb light up during pain episodes. This is called cortical remapping-the brain rewires itself, and sometimes, it rewires wrong.People who had chronic pain before amputation, those who had severe pain on the day of surgery, or those whose amputation was due to cancer are at higher risk. Triggers like stress, cold weather, tight prosthetics, or even a full bladder can make the pain flare up. It’s not psychological. It’s neurological. And it’s real.
Medications: The First Line of Defense
Most doctors start with medication because it’s fast, familiar, and widely available. But not all drugs work the same for everyone. The most common are tricyclic antidepressants like amitriptyline and nortriptyline. These aren’t used because the person is depressed. They work by calming overactive nerves. A typical dose starts at 10 mg at bedtime and slowly increases over weeks. About 45% of users report moderate relief, but drowsiness is common-60% say they feel foggy in the morning.Anticonvulsants like gabapentin and pregabalin are next. Gabapentin starts at 300 mg a day and can go up to 3,600 mg. In Reddit’s r/amputee community, 72% of users found it helpful-but 58% quit because of dizziness or brain fog. Pregabalin works faster but often causes weight gain. Around 40% of users gain at least 5 pounds.
For mild pain, over-the-counter NSAIDs like ibuprofen or naproxen help temporarily. But after three to six months, 80% of users say they stop working. They reduce inflammation, but they don’t touch the nerve signals causing phantom pain.
In stubborn cases, doctors turn to ketamine, an NMDA receptor blocker usually given through IV. It’s powerful-some patients get 50% relief-but it can cause hallucinations or high blood pressure. It’s not for long-term use. Opioids like oxycodone or morphine are controversial. They work, but the risk of addiction is real. The American Pain Society recommends staying under 50 morphine milligram equivalents per day. Still, 35% of long-term users report dependence.
One lesser-known option is botulinum toxin (Botox) injections into the residual limb. For patients with painful neuromas (tangled nerve endings), a single injection can cut pain from 8/10 to 3/10 for up to 12 weeks. It’s not widely used yet, but early results are promising.
Mirror Therapy: Rewiring the Brain Without Drugs
Mirror therapy is one of the most elegant non-drug treatments. It was pioneered by neuroscientist V.S. Ramachandran in the 1990s. The idea is simple: place a mirror vertically beside the intact limb. When you move your good hand and watch its reflection, your brain sees the missing limb moving. This visual feedback tricks the brain into thinking the phantom limb is no longer in pain.You don’t need fancy equipment. A basic mirror box costs under $50. Sessions last 15 to 30 minutes, once or twice a day. You do things like opening and closing your fingers, rotating your wrist, or tapping your toes-whatever you’d do if the limb were still there.
It’s not magic. It takes weeks. Many people give up after two weeks because they don’t feel immediate results. But studies show that those who stick with it for eight weeks or more see pain reductions of 40% to 60%. One 2021 study in the Physical Therapy Journal found that 40% of patients stopped mirror therapy before eight weeks-often because they thought it was silly. But those who kept going? Their pain didn’t just drop-it stayed down.
Now, virtual reality is taking mirror therapy further. Instead of a mirror, patients wear a headset that shows a digital version of their missing limb moving in sync with their good limb. Early trials show this boosts adherence-up to 85% stick with it by 2027, according to the International Association for the Study of Pain. It’s not mainstream yet, but it’s coming.
Other Non-Drug Options
If medications and mirrors aren’t enough, other tools exist. Transcutaneous electrical nerve stimulation (TENS) uses electrodes on the skin to send gentle pulses to the nerves. It’s FDA-cleared, non-invasive, and safe. About 30% to 50% of users report moderate relief. The trick is placement-electrodes need to be near the stump, not on the pain spot. Most people need two or three training sessions to get it right.For severe, unresponsive cases, implanted devices can help. Spinal cord stimulators send pulses to the spinal cord to block pain signals. Newer models, like Saluda Medical’s Evoke, were FDA-approved in January 2024. They adjust automatically based on movement and posture. In trials, patients saw 65% average pain reduction. Motor cortex stimulation, where electrodes are placed on the brain’s surface, is rarer and riskier, but works for about 40% to 60% of patients.
Biofeedback teaches people to control their body’s responses. By watching heart rate or muscle tension on a screen, patients learn to relax. It’s not a cure, but 25% to 40% report better pain control after 10 sessions.

What Works Best Together
No single treatment works for everyone. The most effective approach combines two or more. A 2023 review in OrthoEvidence found that patients who used both gabapentin and mirror therapy had 70% better outcomes than those who used either alone. Those who added TENS or biofeedback saw even more improvement.Doctors are shifting toward early, aggressive treatment. If pain lasts beyond six weeks, waiting isn’t wise. The longer it goes untreated, the more the brain locks in the pain pattern. That’s why top hospitals now have specialized PLP clinics with pain specialists, physical therapists, and psychologists working as a team.
And the need is growing. In 2005, 1.6 million Americans lived with limb loss. By 2050, that number will hit 3.6 million. The pain management market for amputees is already $2.3 billion a year-and it’s only going up.
What to Do Next
If you or someone you know has phantom limb pain:- Start with a low-dose tricyclic antidepressant like amitriptyline, and give it 4-6 weeks to work.
- Try mirror therapy daily for at least 8 weeks. Use a mirror box or a smartphone app with VR mirror simulation.
- If pain doesn’t improve, ask about gabapentin or pregabalin. Don’t be afraid to adjust the dose under a doctor’s care.
- Consider TENS if you want something drug-free and non-invasive.
- Track your pain triggers. Note what makes it worse-stress, cold, fatigue-and try to avoid them.
- Join a support group. The Amputee Coalition has over 12,000 members who share tips, tools, and hope.
Phantom limb pain doesn’t have to be a life sentence. It’s not a mystery. It’s a neurological glitch-and like any glitch, it can be fixed. With the right mix of science, patience, and persistence, relief is possible.
Is phantom limb pain real or just in my head?
It’s real-and it’s neurological, not psychological. Brain scans show activity in areas that once controlled the missing limb. This isn’t imagination; it’s your brain misfiring after nerve damage. The pain is physical, even though the limb is gone.
How long does phantom limb pain last?
For many, it fades within weeks or months. But if it lasts more than six months, it’s unlikely to disappear without treatment. The longer it goes untreated, the more the brain adapts to the pain pattern, making it harder to reverse.
Does mirror therapy really work?
Yes, for many people. Studies show 40% to 60% of users get significant pain reduction after 8 weeks of daily use. The key is consistency. It’s not instant, but it changes how the brain processes pain over time. It’s one of the few treatments with no side effects.
What’s the best medication for phantom limb pain?
There’s no single best drug. Amitriptyline and gabapentin are the most commonly used and studied. Amitriptyline helps with nerve pain and sleep; gabapentin reduces nerve firing. Many people need to try two or three before finding one that works. Always start low and go slow to avoid side effects.
Can I use opioids for phantom limb pain?
Opioids can help in severe cases, but they’re not recommended for long-term use. The risk of dependence is high, and they don’t fix the root cause. The American Pain Society advises limiting opioids to under 50 morphine milligram equivalents per day. They should only be used when other treatments fail and under close supervision.
Are there new treatments on the horizon?
Yes. In January 2024, the FDA approved a new spinal cord stimulator called Evoke that adjusts automatically to movement. Virtual reality mirror therapy is also improving, with apps and headsets that boost adherence. Researchers are testing new NMDA blockers that work like ketamine but with fewer side effects. These could become standard in the next few years.



Been living with this for 12 years now. Mirror therapy saved me. Not magic, just consistent. Did 20 minutes every morning for 10 weeks. Pain dropped from a constant 7/10 to a occasional 2/10. No drugs. No side effects. Just a mirror and patience.
People think it’s placebo. It’s not. Your brain believes what it sees. If you show it the limb moving, it stops screaming.
Start small. Don’t quit after a week. It’s like rehab for your mind.
Thank you for this comprehensive and clinically grounded overview. As a rehabilitation specialist in Vancouver, I have witnessed firsthand the transformative potential of multimodal interventions for phantom limb pain. The integration of mirror therapy with pharmacological management, particularly gabapentinoids, demonstrates a neuroplasticity-based paradigm shift in pain management.
Moreover, the emergence of adaptive spinal cord stimulators such as Evoke represents a significant advancement in precision neuromodulation. I encourage clinicians to refer patients early, before central sensitization becomes entrenched.
They don’t want you to know this… but mirror therapy? It’s just a distraction. The real cause? EMF radiation from smart prosthetics. They’re implanting microchips under the guise of ‘helping’ and the brain’s screaming because it’s being hacked.
They’re using your phantom pain as a data stream. That’s why gabapentin doesn’t work long-term-it’s masking symptoms while they track you.
Try grounding yourself. Walk barefoot. Unplug everything. And stop trusting Big Pharma. They profit from your suffering. The truth is out there.
🫡
ok so like… i read this and i’m like… the brain is remapping but wait-what if it’s not remapping? what if it’s just… the nerves are still firing and the brain is just stuck in a loop? like… it’s not rewiring wrong, it’s just… not getting the signal to shut off?
also i think the btox thing is wild but i’m not surprised. i had a neuroma after my knee amputation and it felt like a live wire. one shot and boom. quiet. but no one talks about it because it’s not profitable.
also… why is everyone so obsessed with gabapentin? it’s just gabapentin. it’s not a miracle. it’s just… less bad than the alternatives. also i spelled ‘botox’ wrong on purpose. i’m tired.
also… did you know that 78% of amputees in the VA system get prescribed opioids within 3 months? and 42% are still on them 2 years later? that’s not treatment. that’s abandonment with a script.
Thank you for presenting this information with such clarity and scientific rigor. The integration of neuroplastic principles into clinical practice for phantom limb pain represents a paradigm shift in rehabilitation medicine. The data supporting mirror therapy, particularly when combined with pharmacological interventions, aligns with current evidence-based guidelines from the International Association for the Study of Pain.
I would respectfully suggest that future iterations include citations for the 2021 Physical Therapy Journal study and the 2023 OrthoEvidence review, to further enhance academic credibility.
I tried everything. Gabapentin made me dizzy. Amitriptyline made me sleep 14 hours. TENS didn’t do squat. Mirror therapy? I thought it was dumb. Then I did it for 30 days straight. No drama. Just me, a mirror, and my good hand.
Now I can get dressed without wincing. That’s worth it.
Don’t listen to the noise. Just try it. For 8 weeks. No excuses.
Neurophysiological mechanisms underlying PLP involve maladaptive cortical reorganization, particularly in the somatosensory homunculus. The mirror visual feedback paradigm induces top-down modulation via the mirror neuron system, reducing aberrant nociceptive signaling.
Pharmacologically, gabapentinoids act on the α2δ subunit of voltage-gated calcium channels, decreasing central sensitization. Amitriptyline inhibits serotonin and norepinephrine reuptake, enhancing descending inhibitory pathways.
Emerging neuromodulatory devices like Evoke utilize closed-loop adaptive stimulation, dynamically adjusting amplitude based on kinematic feedback-this is the future. But only if we stop treating PLP as a psychological issue and start treating it as a neurologic disorder.
Also, Botox for neuromas? Underutilized. 10-20U per neuroma, ultrasound-guided, repeat every 12 weeks. Works better than most meds.
I lost my leg in a motorcycle crash. The pain was worse than the crash. I cried every night for six months.
Then I got a mirror. Then I got a VR headset. Then I got my life back.
It’s not about being strong. It’s about being stubborn.
And yeah-I still do mirror therapy every morning. Even now. Just in case.
Thank you for writing this. I needed to see it again.