Lupus Flare Risk Calculator
Your Personalized Risk Assessment
When we talk about Lupus is a chronic autoimmune disease where the immune system attacks healthy tissues, infections often pop up as unexpected triggers. The connection isn’t a coincidence - the immune system’s over‑reaction to germs can set off a cascade that worsens lupus symptoms.
TL;DR
- Infections can provoke lupus flares by spiking cytokines and stressing the immune system.
- Bacterial and viral bugs differ in how aggressively they trigger flares.
- Vaccination, good hygiene, and early treatment lower flare risk.
- Talk to your rheumatologist before stopping or changing immunosuppressive meds during an infection.
- Recognize warning signs: sudden joint pain, rash, fever, or organ‑specific symptoms.
Why infections matter for people with lupus
People with Systemic Lupus Erythematosus (SLE) already have an immune system that’s on high alert. When an infection strikes, the body releases cytokines like interleukin‑6 and tumor necrosis factor‑α to fight the pathogen. In lupus patients, that cytokine surge can overshoot, sparking a flare that attacks skin, kidneys, heart, or joints.
How different germs affect lupus activity
Not all germs behave the same way. Bacterial infections such as Streptococcus pneumoniae often cause high fevers and rapid inflammation, which have been linked to acute kidney involvement in lupus. Viral infections-think flu, Epstein‑Barr virus (EBV), or COVID‑19-tend to linger, keeping the immune system in a “switched‑on” mode that fuels chronic joint pain and skin rashes.
| Factor | Bacterial Infection | Viral Infection |
|---|---|---|
| Typical Onset | Sudden fever, chills, localized pain | Gradual fever, fatigue, respiratory symptoms |
| Common Triggers | Pneumonia, urinary tract infection, skin cellulitis | Influenza, COVID‑19, EBV, herpes simplex |
| Flare Pattern | Sharp increase in renal or CNS activity | Persistent joint pain, photosensitive rash |
| Management | Prompt antibiotics + possible steroid boost | Antivirals (if available) + careful immunosuppressant adjustment |
Immunosuppressive therapy: double‑edged sword during infection
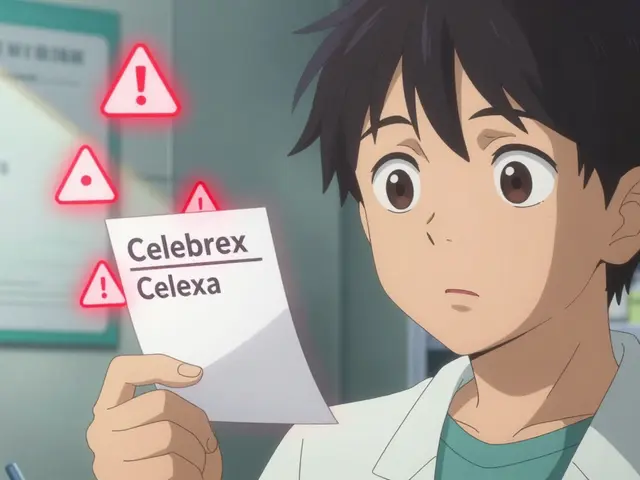
Most lupus patients rely on drugs such as hydroxychloroquine, mycophenolate, or low‑dose prednisone. These medicines keep the immune system from attacking the body, but they also blunt the response to real pathogens. The key is balance: you don’t want the infection to run wild, but you also don’t want a flare caused by abruptly stopping medication.
Clinical guidelines (2023 American College of Rheumatology) suggest tapering steroids only after the infection is controlled, while maintaining hydroxychloroquine when possible because it offers modest antiviral protection.

Preventing infections before they trigger a flare
Prevention is the smartest strategy. Here are the proven moves:
- Vaccination: Get the flu shot, COVID‑19 booster, and pneumococcal vaccine annually. Studies from 2022‑2024 show a 30% reduction in hospitalization for lupus patients who stay up‑to‑date on vaccines.
- Hand hygiene: Simple hand‑washing with soap for 20 seconds cuts bacterial spread by roughly 40% in clinical settings.
- Dental care: Periodontal bacteria can enter the bloodstream, occasionally sparking skin rashes. A dental check‑up every six months lowers this risk.
- Prompt treatment: At the first sign of fever or sore throat, see your doctor. Early antibiotic or antiviral therapy limits the cytokine surge that fuels flares.
Spotting infection‑induced flares early
Because infections and flares share symptoms-fever, fatigue, joint pain-it’s easy to miss the underlying cause. Keep a symptom diary and look for these clues that point to an infection:
- Sudden rise in temperature above 38°C (100.4°F) that doesn’t respond to usual NSAIDs.
- Localized pain (e.g., sore throat, ear pain, urinary burning) that precedes joint swelling.
- New rash that appears in a pattern typical of viral exanthems rather than classic lupus malar rash.
If two or more of these appear, contact your rheumatologist promptly. Early labs-CBC, CRP, and cultures-help differentiate infection from a pure autoimmune flare.
Managing a flare triggered by infection
When an infection‑related flare strikes, a stepwise approach works best:
- Identify the pathogen: Blood, urine, or throat cultures guide targeted therapy.
- Adjust immunosuppression: Temporarily increase steroids (e.g., prednisone 10‑20mg) while keeping hydroxychloroquine.
- Use disease‑specific agents wisely: Biologics like belimumab can be paused during severe bacterial infections.
- Supportive care: Hydration, rest, and nutrition help the body fight both the bug and the autoimmune attack.
Most patients recover fully within 2‑4 weeks once the infection is cleared and the flare is quelled.
Living with the risk: a long‑term outlook
Long‑term data from the Lupus International Collaborating Clinics (LICC) registry (2020‑2024) show that patients who follow a strict infection‑prevention plan experience 25% fewer severe flares over five years. That translates into better quality of life, fewer hospital stays, and lower cumulative organ damage.
It’s not about eliminating every germ-an impossible goal-but about staying ahead of the ones that matter most.

Frequently Asked Questions
Can the flu cause a lupus flare?
Yes. The flu triggers a strong cytokine response that can aggravate skin, joint, and kidney involvement in lupus. Getting the flu vaccine each year dramatically lowers this risk.
Should I stop my lupus meds if I catch a cold?
Usually no. Hydroxychloroquine is safe to continue and may even help. Only steroids or stronger immunosuppressants might need temporary adjustment, and that should be done under your doctor’s guidance.
Are antibiotics enough to prevent a lupus flare?
Antibiotics treat bacterial infections, which can stop an infection‑driven flare. However, they won’t affect viral triggers, so antiviral meds or vaccines are also crucial.
What are the most common infections in lupus patients?
Urinary tract infections, pneumonia, and skin cellulitis are top bacterial culprits. Viral respiratory infections-flu, COVID‑19, and RSV-are the leading viral threats.
How often should I see my doctor for infection monitoring?
At minimum, schedule a routine rheumatology visit every 3‑6 months. If you develop any fever, new rash, or worsening joint pain, call your clinic within 24‑48 hours.




Hey everyone, just wanted to say that understanding how infections spark lupus flares can really empower us to stay ahead of the game. Keeping an eye on subtle fever spikes and quick changes in joint pain can be the early alarm we need. Vaccinations and solid hand‑hygiene routines are simple yet powerful tools that most of us can stick to. If you’re on immunosuppressants, a quick chat with your rheumatologist before any infection hits can save a lot of trouble. Remember, the goal is to manage the triggers, not to live in fear.
Great, another reminder that germs love us more than we love pizza.
It’s worth noting that not every fever means a lupus flare; sometimes it’s just a harmless cold that the body is clearing. Still, the overlap can be confusing, so a symptom diary can make a huge difference when you talk to your doctor. Staying on hydroxychloroquine during mild viral infections often provides a safety net without compromising the immune response too much. Regular blood work helps catch any hidden inflammation before it escalates.
While the advice above is sound, physicians must also remember that abrupt tapering of steroids during an infection can precipitate a rebound flare of even greater severity. The cytokine cascade, once unleashed, behaves like a runaway train, overwhelming both renal and central nervous system tissues. Therefore, the decision to adjust immunosuppression should be anchored in objective laboratory markers, not just clinical intuition. A balanced approach-maintaining baseline therapy while judiciously adding short‑term steroids-often yields the best outcomes.
When we dive deep into the mechanics of how a simple bacterial infection can turn a relatively stable lupus patient into a storm of symptoms, the picture becomes both fascinating and alarming. First, the invading pathogen triggers an acute phase response, flooding the bloodstream with interleukin‑6, tumor necrosis factor‑α, and other pro‑inflammatory mediators. Those molecules, although meant to fight the infection, also act like accelerators on the already sensitized immune system of a lupus patient. The result is a rapid escalation of autoantibody production, which in turn begins to deposit in kidneys, skin, and joints. This cascade is not instantaneous; it often begins within hours of the initial fever and can peak within a few days, leaving little time for the patient to react. Moreover, the nervous system picks up these signals, leading to headaches, confusion, and sometimes seizures if cerebral vasculature is involved. The kidneys, being especially vulnerable, may show rising proteinuria, prompting an urgent need for nephrology input. Meanwhile, the skin may develop a rash that mimics the classic malar pattern but with a more widespread distribution, adding to diagnostic confusion. All of these manifestations demand a swift reassessment of the current immunosuppressive regimen. Physicians often face the dilemma of whether to intensify steroids, introduce additional agents, or hold off to avoid compromising the fight against the infection itself. In practice, many clinicians opt for a short course of high‑dose prednisone while preserving the baseline hydroxychloroquine, striking a delicate balance between anti‑infective immunity and autoimmune control. Simultaneously, supportive care-adequate hydration, rest, and nutritional support-plays an unsung yet crucial role in modulating the body’s response. Preventive strategies, such as up‑to‑date vaccinations and meticulous oral hygiene, form the first line of defense, reducing the probability of such catastrophic events. Lastly, patient education cannot be overstated; individuals who understand the warning signs are more likely to seek early medical attention, ultimately averting severe organ damage. In sum, the interplay between infection and lupus flare is a high‑stakes dance, where timing, dosage, and vigilance dictate the outcome.
It is incumbent upon the medical community to acknowledge that the prevailing emphasis on vaccination, while undeniably beneficial, may inadvertently marginalize the nuanced role of personalized immunosuppressive tapering protocols during acute infections. The literature reveals a paucity of randomized controlled trials that delineate optimal steroid adjustment thresholds, thereby leaving practitioners to rely on anecdotal experience. Such a deficit underscores the necessity for rigorously designed studies that stratify patients based on infection type, severity, and baseline disease activity. Until such evidence emerges, clinicians must exercise prudence, documenting each therapeutic decision with meticulous detail to inform future practice. Moreover, patient autonomy should be respected by involving individuals in shared decision‑making, particularly when weighing the risks of potential flare against infection control. In this manner, we can aspire to a more balanced therapeutic paradigm that prioritizes both safety and efficacy.
One practical tip that often gets overlooked is the importance of regular dental check‑ups; gum disease can act as a silent source of bacterial translocation, subtly fueling systemic inflammation. Pair that with a simple habit of carrying hand sanitizer in your bag, and you’ve got two low‑effort, high‑impact defenses against infection. Also, consider setting a reminder on your phone to schedule flu and pneumococcal vaccinations well before the cold season rolls around. Staying proactive not only reduces flare risk but also gives you a psychological boost, knowing you’ve taken concrete steps to protect your health.
If we examine the concept of “trigger” through a broader philosophical lens, we might conclude that every external stimulus merely reveals the underlying fragility of an already dysregulated immune network. In other words, infections are not the cause of lupus; they are merely mirrors reflecting an immune system primed for overreaction. This perspective invites a shift in focus from attempting to eradicate every possible pathogen to cultivating resilience within the body's regulatory pathways. Practices such as stress reduction, adequate sleep, and balanced nutrition therefore become integral components of a comprehensive management strategy.
Some folks argue that the whole “vaccinate‑or‑you‑die” narrative is a smokescreen, obscuring the fact that pharmaceutical companies hold patents on many of the adjuvants that can themselves provoke immune activation. While the evidence for large‑scale harm is limited, the mere possibility that certain preservatives could act as hidden triggers should encourage us to scrutinize vaccine formulations more closely. Transparency in ingredient disclosure would empower patients to make truly informed choices, especially those already battling an autoimmune condition.
When a patient experiences a mild upper‑respiratory infection, the body’s innate immune response, characterized by neutrophil recruitment and interferon release, can overlap with the pathways that drive lupus activity. This overlap often manifests as joint stiffness and low‑grade fever, which can be mistaken for a simple cold. Recognizing this pattern early allows for timely intervention, such as a short course of low‑dose steroids, to prevent a full‑blown flare. Continual monitoring of biomarkers like CRP and complement levels offers an objective gauge of whether the infection is escalating into autoimmunity.
From a clinical standpoint, the synergy between meticulous hand hygiene and up‑to‑date immunizations constitutes a cornerstone of infection prophylaxis for lupus patients. Hand washing with soap for a minimum of 20 seconds reduces microbial load significantly, while vaccines prime the adaptive immune system without overwhelming the suppressed innate defenses. Additionally, regular assessment of immunoglobulin levels can reveal hidden deficiencies that predispose patients to opportunistic infections. Addressing such gaps with appropriate IgG replacement therapy further fortifies the patient’s immune resilience, thereby minimizing flare‑inducing insults.
Vaccines are a game‑changer for lupus 🙌
Here’s a quick checklist to keep infections at bay and protect against lupus flares:
• Get the annual flu shot and a pneumococcal vaccine every five years.
• Wash your hands thoroughly for at least twenty seconds before meals and after public transport.
• Keep dental appointments every six months to prevent periodontal bacteria from entering the bloodstream.
• Carry a small hand‑sanitizer bottle for on‑the‑go cleaning.
• Schedule routine blood work to monitor CRP, complement levels, and complete blood counts.
• Maintain a symptom diary to spot early signs of infection or flare.
By sticking to these habits, you reduce the likelihood of an infection‑driven flare dramatically.
Absolutely! I’ve seen patients who missed just one dental cleaning and subsequently battled a nasty gum‑derived infection that snowballed into a renal flare. The lesson? Consistency beats occasional heroics every time.
Keeping a simple fever log-recording temperature spikes, duration, and accompanying joint pain-can serve as an early warning system, letting you and your doctor intervene before a full flare sets in.
Let's all rally around preventive care! 🎉 Stay vaccinated, wash those hands, and never skip a dentist visit-your future self will thank you! 🌟💪
In the spirit of collaboration, I’d add that sharing personal success stories about infection prevention within support groups can amplify motivation and spread practical tips across the community.