Why Older Bodies Need Different Doses
Your body changes as you age-and so should your meds. A pill that worked perfectly at 50 might cause dizziness, falls, or confusion at 75. It’s not about being more sensitive; it’s about how your liver, kidneys, and fat distribution have shifted. The medication dosage adjustments for aging bodies and organs aren’t optional-they’re essential to avoid hospital trips and dangerous side effects.
Think of your body like an old car. The engine still runs, but the fuel system is slower, the filters clog easier, and the oil doesn’t circulate as well. Same with drugs. Older adults absorb, distribute, metabolize, and clear medications differently. A 2022 study in JAMA Internal Medicine found that 35% of hospital admissions for people over 65 are due to bad reactions to meds. Most of those could’ve been avoided with the right dose.
How Aging Changes Your Body’s Handling of Drugs
There are four big ways aging affects how drugs work in your body-and none of them are minor.
- Absorption: Stomach acid drops by 20-30%, and blood flow to the gut slows. That means pills don’t dissolve or get into your bloodstream as quickly. Some meds might not work as well, while others build up slowly and cause delayed side effects.
- Distribution: As you age, you lose muscle and gain fat. Many drugs stick to fat instead of circulating where they’re needed. That’s why a standard dose of a sleep aid or antidepressant can leave you groggy all day-you’re getting more of the drug in your system than intended.
- Metabolism: Your liver processes drugs 30-50% slower after 65. Drugs like painkillers, antipsychotics, and statins hang around longer. That’s why a 10mg dose at 40 might become a 5mg dose at 70.
- Excretion: Kidneys filter drugs out of your blood. After 30, your kidney function drops about 8 mL per minute every decade. By 70, 40% of people have kidney function below the level needed for standard doses of common drugs like gabapentin or metformin.
These changes don’t happen all at once. But they add up. And if you’re taking five or more meds-55% of seniors are-you’re stacking up risks.
The Golden Rule: Start Low, Go Slow
Doctors don’t just guess doses for older adults. They follow a clear, proven method: start low, go slow. This isn’t a suggestion-it’s the standard backed by the American Geriatrics Society since the 1980s.
For example:
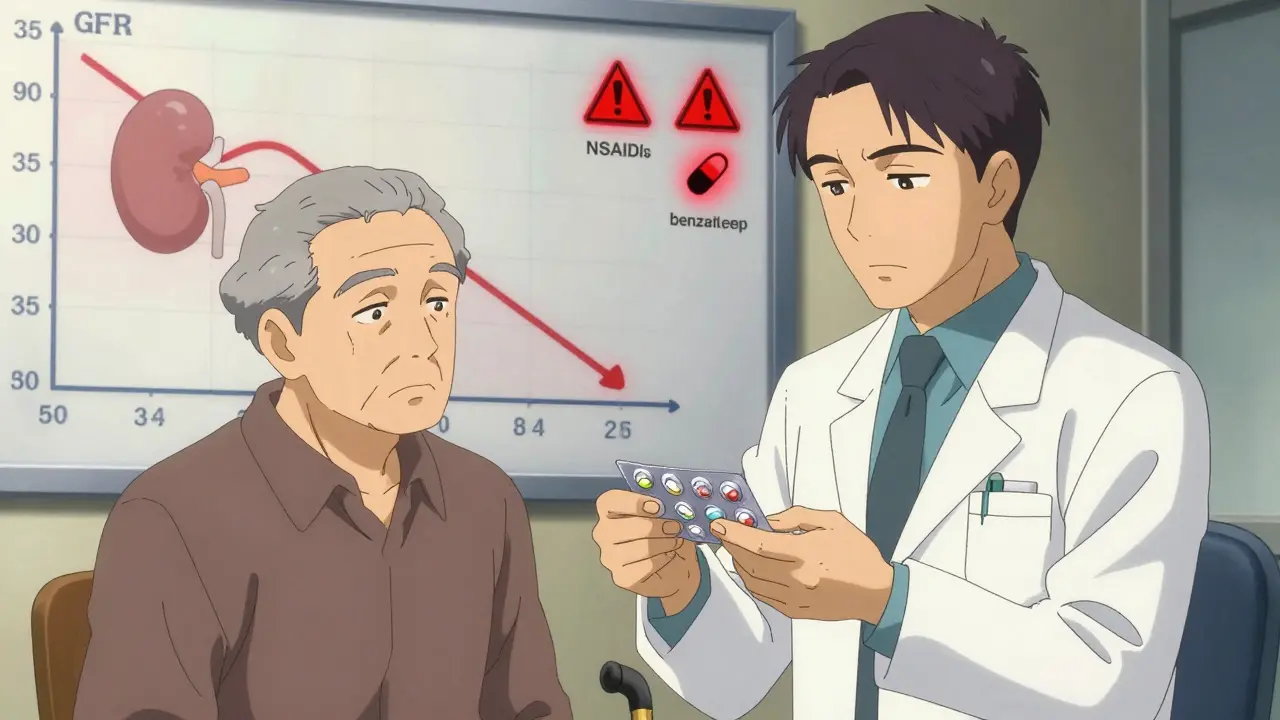
- Gabapentin: Standard dose is 300mg three times a day. For someone over 70 with reduced kidney function, the starting dose is 100mg once a day. It’s slowly increased only if needed.
- Metformin: Used for diabetes. If your kidney filter rate (eGFR) drops below 45, the dose is cut in half. Below 30, it’s stopped entirely.
- Benzodiazepines: Drugs like diazepam or lorazepam are linked to a 50% higher risk of falls in seniors. Even if prescribed for anxiety or sleep, they’re often replaced with safer alternatives-or avoided altogether.
The goal isn’t to eliminate meds. It’s to find the smallest dose that still works. Sometimes, less is more.
How Doctors Calculate the Right Dose
It’s not just about age. It’s about function. Two 72-year-olds might need completely different doses based on their kidneys, liver, and overall health.
The most common tool doctors use is the Cockcroft-Gault equation. It estimates kidney function using age, weight, and a blood test for creatinine. Here’s the simplified version:
CrCl = [(140 - age) × weight in kg] ÷ [72 × serum creatinine]
For women, multiply the result by 0.85.
If your CrCl is below 50 mL/min, most kidney-cleared drugs need a dose reduction. For drugs processed by the liver, doctors use the Child-Pugh score, which looks at liver function through blood tests and physical signs like fluid buildup. A score of 7-9 means cut the dose in half. A score of 10-15 means avoid the drug entirely.
For some meds, like digoxin (used for heart rhythm), doctors check blood levels. In older adults, the safe range is 0.5-0.9 ng/mL-much lower than for younger people. But here’s the problem: blood tests like this aren’t available for 85% of common medications. That’s why doctors rely on clinical signs: confusion, dizziness, fatigue, or unexplained falls.
High-Risk Meds to Watch Out For
The 2023 Beers Criteria® lists 30 classes of drugs that are risky for older adults. These aren’t just “maybe bad”-they’re known to cause harm.
- Anticholinergics: Found in many sleep aids, bladder meds, and even some allergy pills. Long-term use doubles dementia risk.
- NSAIDs: Ibuprofen, naproxen. Increase stomach bleeding risk by 300%. Even occasional use can be dangerous.
- Antipsychotics: Used for dementia-related agitation. They increase stroke and death risk in seniors.
- Warfarin: A blood thinner. Older adults need 20-30% lower doses. Too much can cause internal bleeding.
- Insulin and sulfonylureas: Can cause dangerous low blood sugar. Seniors often don’t feel the warning signs.
If you’re on any of these, ask: Is this still necessary? Is there a safer alternative? Could the dose be lowered?
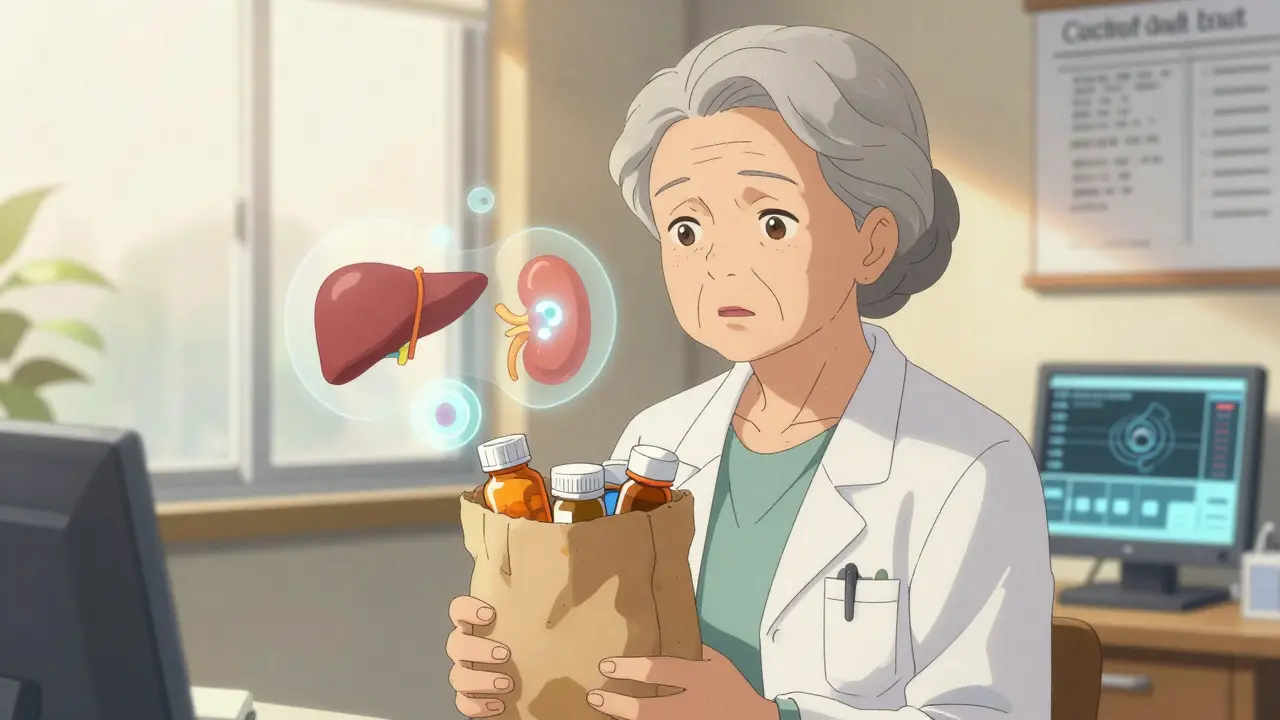
What You Can Do: The Brown Bag Review
You don’t have to wait for your doctor to catch a problem. Take control with the brown bag review.
Every six months, empty all your pills-prescription, over-the-counter, vitamins, supplements-into a brown paper bag. Bring them to your appointment. Don’t just say, “I take my meds.” Show them.
Studies show this simple step cuts medication errors by 40%. Why? Because:
- You might be taking two pills with the same active ingredient.
- You might be using an old prescription you forgot to refill.
- You might be taking something your doctor didn’t know about.
Also, ask: “Is this still helping me?” If you’re taking a statin for cholesterol but haven’t had a heart issue in 10 years, maybe it’s time to reconsider. If you’re on a sleep pill that’s made you fall three times in the last year, it’s not worth it.
When to Ask for a Pharmacist’s Help
Pharmacists are the hidden heroes in geriatric dosing. A 2022 study found they reduce medication errors by 67% in older patients.
Most pharmacies now offer free medication reviews. Ask for one. They’ll:
- Check for dangerous interactions.
- Spot duplicate prescriptions.
- Adjust doses based on kidney or liver function.
- Set up blister packs with daily doses.
Programs like the University of North Carolina’s “Pharm400” use weekly blister packs and pharmacist check-ins to reduce hospitalizations by 22%. That’s not magic-it’s smart, consistent care.

Family and Caregivers: Your Role Matters
If you’re helping a parent or partner manage meds, you’re not just a helper-you’re a safety net.
Research shows family involvement improves adherence by 37%. Here’s how to help:
- Keep a written list of all meds, doses, and times.
- Set phone alarms for pill times.
- Watch for new confusion, balance issues, or loss of appetite.
- Don’t let them skip doses “just because they feel fine.”
And if they’re in a nursing home or assisted living, ask: Do they have a pharmacist reviewing meds weekly? If not, push for it.
The Future: Personalized Dosing for Seniors
Right now, dosing is based on age and lab numbers. But the future is smarter.
Researchers are starting to use functional age instead of chronological age. That means:
- How fast can they walk? (Timed Up and Go test: over 12 seconds = higher risk)
- Can they remember to take pills?
- Do they have muscle weakness or balance problems?
AI tools are being tested to predict the right dose based on real-world data. One pilot at Johns Hopkins cut dosing errors by 47%. The NIH is spending $127 million to build models that predict how a person’s body will handle a drug-not just based on age, but on their unique biology.
By 2030, experts predict 70% of high-risk meds for seniors will be dosed using personalized, lab-guided methods. That’s huge. But until then, the best tool you have is awareness-and asking the right questions.
Final Thought: It’s Not About Age. It’s About Function.
There’s no magic number. You can be 70 and have the kidneys of a 50-year-old. Or you can be 80 and still strong, sharp, and active. The dose should match your body-not your birth certificate.
Don’t assume your meds are fine just because they’ve been on your list for years. Revisit them. Ask your doctor or pharmacist: Is this still right for me today?
One small change-a lower dose, a different pill, a stopped med-can mean the difference between staying independent and ending up in the hospital. And that’s worth every conversation.
Why can’t older adults take the same dose as younger people?
Older bodies process drugs differently. Kidneys and liver slow down, body fat increases, and muscle mass decreases. This means drugs stay in the system longer and can build up to dangerous levels. A standard adult dose may be too strong and lead to falls, confusion, or organ damage.
What is the Beers Criteria and why does it matter?
The Beers Criteria is a list of medications that are potentially harmful for older adults, updated every two years by the American Geriatrics Society. It identifies drugs like benzodiazepines, NSAIDs, and anticholinergics that increase risks of falls, dementia, or bleeding. Doctors use it to avoid prescribing these drugs or to reduce doses when absolutely necessary.
How do I know if my kidney function is low enough to need a dose change?
Your doctor can calculate your creatinine clearance (CrCl) using your age, weight, and a simple blood test for creatinine. If your CrCl is below 50 mL/min, many medications-like gabapentin, metformin, or certain antibiotics-need lower doses. A GFR (eGFR) below 60 is also a red flag. Ask for your numbers at your next visit.
Can I just stop a medication if I think it’s causing problems?
Never stop a prescribed medication without talking to your doctor. Some drugs, like blood pressure pills or antidepressants, can cause serious withdrawal effects if stopped suddenly. But if you’re feeling dizzy, confused, or unusually tired, bring it up. Your doctor can help you safely reduce or switch the drug.
Are over-the-counter meds safe for seniors?
Not always. Many OTC drugs-like sleep aids with diphenhydramine, pain relievers like ibuprofen, or cold medicines with antihistamines-are anticholinergic or hard on the kidneys. They’re often just as risky as prescription drugs. Always check with your pharmacist before taking anything new, even if it’s sold on a shelf.
How often should my meds be reviewed?
At least once a year, but ideally every six months if you’re on five or more medications. Changes in health, weight, or kidney function can make old doses unsafe. A brown bag review with your pharmacist or doctor is the best way to stay on track.
Next Steps for Seniors and Families
Start today. Grab a brown bag. Write down every pill, vitamin, and supplement you take. Schedule a 20-minute appointment with your pharmacist or doctor. Ask: “Is this still the right dose for me?”
Small actions now prevent big problems later. One less pill, a lower dose, or a safer alternative can mean more independence, fewer falls, and more years living well at home.




I took my mom to her pharmacist for a brown bag review last month. Turned out she was taking two different sleep aids with diphenhydramine. One was prescription, one was OTC. She’d been dizzy for months. Cut one out, lowered the other. She’s walking without a cane now. Why don’t more people do this?
In India, we don’t have access to pharmacists who do these reviews. Most seniors just take what the doctor gives them and never question it. I’ve seen grandmas on five meds they don’t need. The system doesn’t care. But awareness is growing. My uncle stopped his statin after 12 years-no heart issues since 2010. His doctor was shocked he asked.
This post is dangerously naive. You’re telling people to just stop or lower meds without understanding the consequences. I’ve seen patients go into cardiac arrest because their beta-blocker was cut too fast. This isn’t a DIY project. It’s medical malpractice waiting to happen.
The Cockcroft-Gault equation remains the gold standard for estimating CrCl in older adults, though CKD-EPI is gaining traction in younger populations. For drugs with narrow therapeutic windows-digoxin, warfarin, lithium-TDM is essential. Unfortunately, TDM availability is severely limited in community settings, forcing reliance on clinical vigilance. The Beers Criteria is underutilized in primary care; only 38% of PCPs report using it routinely.
My dad was on gabapentin for nerve pain. 300mg three times a day. He started nodding off in the middle of dinner. We asked his doctor to check his kidney function. CrCl was 38. They dropped him to 100mg once a day. He’s been fine since. It’s not about age. It’s about function. Simple.
I’m 68 and I’ve been on metformin for 15 years. Last year my eGFR dropped to 42. My doctor cut my dose in half and told me to check my blood sugar more often. I didn’t even know I could get my kidney numbers without a full panel. This post saved me from a fall. Thank you.
My aunt in Delhi was on ibuprofen daily for arthritis. She ended up in the ER with a GI bleed. Turned out she didn’t know it was an NSAID. She thought it was just a painkiller. We need more public education. Not just for seniors, but for families who think OTC means safe.
I just started doing the brown bag thing with my 81-year-old neighbor. We sat on her porch with a big paper bag full of bottles. Found three pills she hadn’t taken in six months. Found one she was taking twice a day by accident. We laughed. She cried. Then we called her pharmacist together. She said, ‘I feel like I just got my life back.’ That’s what this is about. Not science. Not numbers. People.
I’m a retired nurse. I’ve seen this too many times. A 76-year-old woman on 11 medications. Seven of them were for side effects of the others. We cut four. She stopped falling. She started gardening again. The system is broken. But you don’t need the system to fix this. You just need to ask the question: Is this still helping?