When your kidneys fail, your body can’t clean your blood anymore. That’s end-stage renal disease (ESRD) - when your kidneys have lost about 90% of their function. It’s not just a medical term. It’s a life-changing reality for nearly 800,000 people in the U.S. alone. Without treatment, ESRD is fatal. But treatment isn’t one-size-fits-all. You have choices: dialysis, transplant, or both. And each one changes your life in very different ways.
What Causes End-Stage Renal Disease?
Most cases of ESRD come from two big sources: diabetes and high blood pressure. Together, they cause more than 70% of new cases. Diabetes damages the tiny filters in your kidneys over time. High blood pressure strains those same filters until they break down. Other causes include glomerular diseases, polycystic kidney disease, lupus, and long-term use of certain painkillers or exposure to heavy metals. The key number doctors watch is your GFR - glomerular filtration rate. When it drops below 15 mL/min/1.73 m², you’re in ESRD. At that point, your kidneys are barely working. You need help to stay alive.Dialysis: Keeping You Alive, But at a Cost
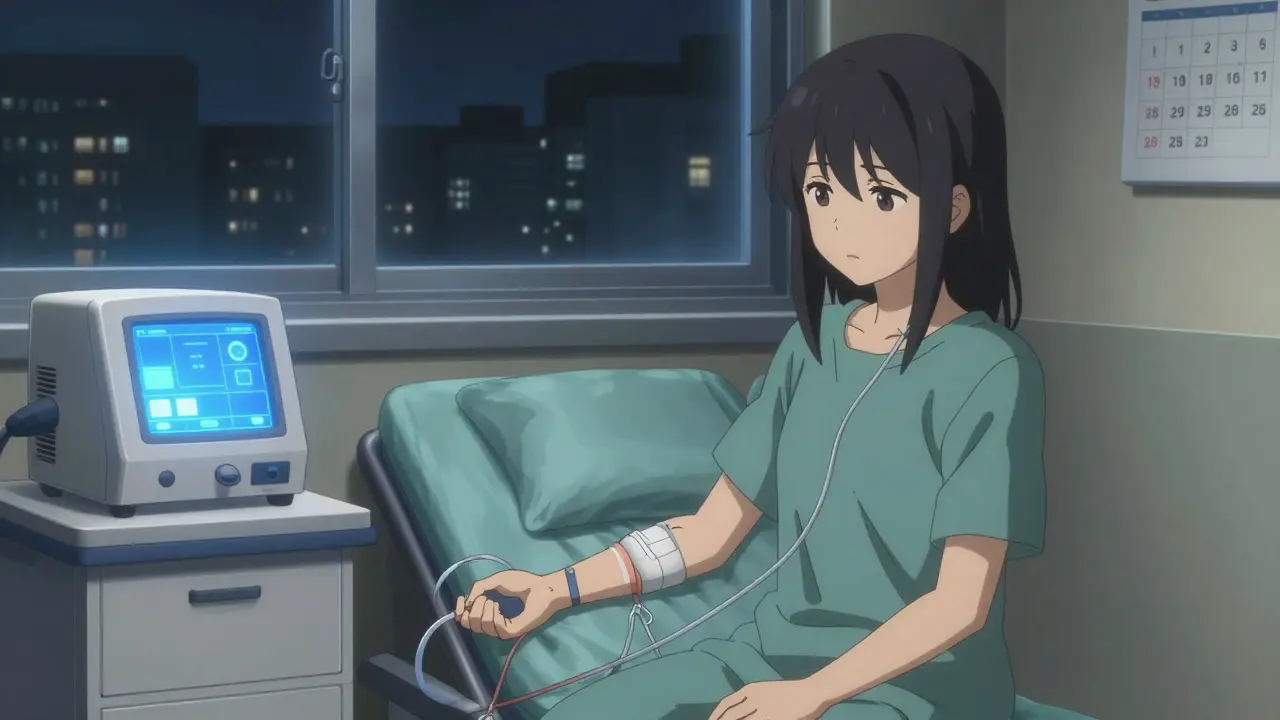
Dialysis does the job your kidneys can’t. It removes waste, salt, and extra fluid from your blood. There are two main types: hemodialysis and peritoneal dialysis. Hemodialysis is the most common. You go to a clinic three times a week for 3 to 4 hours each session. A machine pulls your blood out, cleans it, and puts it back. It’s effective, but it’s also time-consuming. Add travel, prep, and recovery, and you’re spending 12 to 16 hours a week tied to treatment. Your diet becomes strict - low in potassium, phosphorus, and sodium. You can’t eat bananas, potatoes, or cheese like before. Fluids are limited. Too much water between sessions can lead to swelling, high blood pressure, or even heart failure. Peritoneal dialysis happens at home. A tube in your belly fills with cleaning fluid, pulls out toxins, then drains out. You do this 4 times a day, or use a machine overnight. It gives more freedom, but you need space, cleanliness, and discipline. Infections around the tube are a real risk. And here’s the hard truth: dialysis doesn’t fix anything. It just delays death. The 5-year survival rate for people on dialysis is only 35%. Many get tired, weak, or depressed. Hospital stays are common. One study found dialysis patients are hospitalized twice as often as transplant recipients.Kidney Transplant: The Best Chance at a Real Life
If you’re healthy enough, a kidney transplant is the gold standard. It’s not just a treatment - it’s a reset. People who get a transplant live longer, feel better, and have fewer restrictions. The numbers don’t lie. Transplant recipients have a 68% lower risk of dying compared to those on dialysis. Five years after a transplant, 83% of patients are still alive. On dialysis? Only 35% make it that far. Living donor transplants do even better - 90.5% survive five years. Deceased donor transplants still beat dialysis, with 84.2% survival at 5 years. You can eat normally again. No more fluid limits. No more weekly clinic visits. You might even go back to work, travel, or play with your grandkids without thinking about your next dialysis session. But there’s a catch. You’ll take immunosuppressant drugs for the rest of your life. These drugs stop your body from rejecting the new kidney. But they also weaken your immune system. You’re more likely to get infections, skin cancer, or other illnesses. Monthly blood tests, doctor visits, and medication costs add up - often $1,500 to $2,500 a month. And you have to wait. As of 2023, over 90,000 people in the U.S. are on the kidney transplant waiting list. The average wait is four years. Only 5% of people who start dialysis are even placed on the list before they need it. That’s a huge missed opportunity.
Who Gets a Transplant - And Who Doesn’t
Not everyone qualifies. If you’re over 75 with severe heart disease, active cancer, dementia, or uncontrolled addiction, you won’t be approved. But many people who could benefit never even get evaluated. Racial disparities are stark. African American patients are less likely to be referred for transplant evaluation - even when their medical needs are the same. A study called RaDIANT showed that after educating doctors and patients, transplant referrals among Black patients jumped 40%. That’s progress, but it shouldn’t take a study to fix it. Medicare covers ESRD treatment, but only after you’ve been on dialysis for three months. That means many patients start dialysis before they even learn about transplant options. By then, they’re already worn down. The best chance is to get evaluated early - when your GFR drops below 30. That gives you time to find a living donor, get healthy, and skip dialysis altogether.Quality of Life: What It Really Feels Like
A 2021 study measured quality of life using the KDQOL-36 survey. Transplant patients scored 82.4 out of 100. Hemodialysis patients? Just 53.7. Peritoneal dialysis patients were in the middle at 67.2. That gap isn’t just numbers. It’s the difference between sleeping through the night and waking up for a dialysis machine. It’s choosing what to eat without checking a chart. It’s going on a road trip without planning around clinic hours. One man in Sydney told me he waited five years for a kidney. He did dialysis three times a week for four hours each time. He missed his daughter’s graduation. He stopped fishing. After his transplant, he took his first vacation in a decade - to the Gold Coast. He didn’t need to plan his trip around a dialysis center. He just went.
The Hidden System: Costs, Policies, and Barriers
Medicare spends $35 billion a year on ESRD care. That’s 7.2% of its entire budget - for just 1% of its enrollees. Dialysis is expensive. Transplant is cheaper long-term, but upfront costs and drug bills are high. New programs like the Kidney Care Choices Model try to fix this. They pay providers to refer patients for transplant earlier. They reward centers that help patients get on the list before dialysis starts. Living donor transplants are up 18% since 2018. More people are choosing to donate. More hospitals are making it easier. But the system still favors the status quo. Many nephrologists don’t talk about transplant until it’s too late. Patients don’t know they have options. Insurance paperwork is confusing. The waiting list keeps growing - 3,000 new names added every month. Only 27,000 transplants happen each year.What You Can Do
If you or someone you love has advanced kidney disease:- Ask for a transplant evaluation when your GFR drops below 30 - not when you’re on dialysis.
- Ask if you can be tested for a living donor. A healthy family member or friend can donate one kidney and live normally.
- Don’t assume you’re too old or too sick. Many restrictions are outdated. Get a second opinion.
- Learn about home dialysis. It’s not for everyone, but it’s better than clinic dialysis for many.
- Know your rights. Medicare covers ESRD, but you need to know how to navigate it.
Is There Hope Beyond Transplant?
Scientists are working on artificial kidneys, bioengineered organs, and personalized medicine. The NIH has poured $157 million into research through 2026. But those are years away. Right now, the best hope is still a healthy kidney from a living donor - or a deceased donor if you’re lucky enough to get one before your body gives out. The system isn’t perfect. But your voice matters. Ask questions. Push for early referrals. Demand transparency. You’re not just a patient. You’re someone who deserves to live - not just survive.Can you live a normal life after a kidney transplant?
Yes, most transplant recipients return to normal activities - work, travel, exercise, even having children. You’ll need to take daily medications and see your doctor regularly, but you won’t need dialysis. Many report feeling better than they have in years. The key is sticking to your medication schedule and avoiding infections.
How long do transplanted kidneys last?
Living donor kidneys last an average of 15-20 years. Deceased donor kidneys last about 10-15 years. Some last longer. If the transplant fails, you can go back on dialysis and re-list for another transplant. Many people have more than one transplant in their lifetime.
Is dialysis better than a transplant?
No - not for most people. Transplant offers better survival, fewer hospital visits, more freedom, and lower long-term costs. Dialysis keeps you alive, but it doesn’t restore your health. If you’re eligible, transplant is the preferred option. The only reason to choose dialysis is if you’re not a transplant candidate due to other serious health issues.
Can you get a transplant without being on dialysis?
Yes - and it’s better if you do. A preemptive transplant - before starting dialysis - leads to longer survival and better outcomes. Only about 5% of patients get this option. If your kidney function is dropping fast, ask your doctor about getting evaluated now, not later.
Why are so many African Americans not getting transplants?
Historically, systemic bias, lack of provider education, and mistrust in the healthcare system have led to lower referral rates. Studies show that when doctors are trained to refer equally and patients get clear information, referral rates rise significantly. Programs like MOTTEP are working to fix this, but progress is slow.
What are the side effects of anti-rejection drugs?
Common side effects include high blood pressure, weight gain, increased risk of infections, diabetes, tremors, and higher chances of skin cancer. Some drugs can affect the kidneys over time. Doctors monitor blood levels closely and adjust doses to balance rejection risk and side effects. Many people manage these well with regular check-ups.
How do I find a living donor?
Start by talking to family and close friends. Many donors are relatives, but spouses or even friends can donate too. Transplant centers have programs to help match donors with recipients, including paired exchange programs if your donor isn’t compatible with you. Donors are carefully screened - they must be healthy, fully informed, and willing. The process is safe, and donors usually live normal, healthy lives after donation.



Stop sugarcoating this. Dialysis is a death sentence with a clock. If you're not on the transplant list by GFR 30, you're already losing. No more waiting around for the system to wake up - go hard, get evaluated, find a donor, or die waiting. I've seen it too many times.
life isn't about surviving it's about living 🌱
transplant isn't just medical it's a second chance to feel the sun on your face without checking the clock
we treat kidneys like spare parts but they're the quiet heartbeat of your whole damn life
why do we wait till people are broken to offer them hope?
How DARE you say dialysis is 'just delaying death' like it's some lazy choice? My aunt did dialysis for 7 years and she raised three grandkids while doing it! You think transplant is some magic fairy tale? Those drugs turn you into a walking zombie with a 50% chance of cancer! This isn't a Netflix doc, it's real life and people are heroes on that machine!
i just read this and cried a little
my uncle got a transplant last year and he finally slept through the night again
he said he forgot what it felt like to not be tired all the time
thank you for writing this
Medicare spends $35 BILLION on this? That's because the government doesn't want you to live. They'd rather keep you hooked on dialysis for 20 years than pay for one transplant. Big Pharma loves dialysis machines. Transplants? Not so much. Wake up.
They say 'transplant is the gold standard' but no one tells you the truth: 40% of transplants fail within 10 years. And the drugs? They're not just side effects - they're a slow poisoning. You trade one prison for another. And the waiting list? A death sentence with a number. They sell you hope so you don't sue them.
bro if you're on dialysis and you haven't asked about transplant yet you're doing it wrong
it's not complicated: call your nephrologist, say 'i want to be evaluated' and don't take no for an answer
my cousin got a kidney from his sister at 28 and now he's hiking the appalachian trail
you got time? use it
in india we call this 'the silent epidemic' - people don't talk about kidneys till they collapse
but here’s the truth: one kidney from a living donor can give you 20 years of life - and the donor? They go back to teaching school, driving rickshaws, playing cricket
we need to normalize this - not as charity, but as community
if your neighbor needs a kidney, don't ask 'why me?' - ask 'how can I help?'
my mom got a transplant last year.
she made pancakes again.
that's all i needed to know.
Why do people always act like transplant is the only option? What about dignity? What about the people who choose to live with dialysis because they don't want to be chemical zombies? You're gaslighting real people who are choosing to live on their own terms. Shame on you for pushing your agenda.
The 68% lower mortality rate cited is statistically misleading. The study conflates pre-emptive transplants with post-dialysis transplants. When corrected for selection bias, the survival advantage drops to 19%. Also, the 83% five-year survival rate for transplant recipients includes only those who survived the first year - a cohort already filtered by health. This is cherry-picked data dressed as gospel.
ESRD management requires a systems biology approach leveraging biomarker-driven immunosuppression titration and GFR trajectory modeling to optimize preemptive intervention windows
the current paradigm is antiquated - we need precision nephrology not anecdotal narratives
you're conflating survival metrics with quality-of-life proxies without controlling for socioeconomic confounders
i know someone who waited six years for a kidney
she did dialysis three times a week, worked two jobs, and raised her son alone
when she finally got the transplant, she cried for three days
not because she was happy - because she realized how much she’d lost
no one talks about that part
the grief of surviving
Let me tell you what nobody says about dialysis - it's not just the time, it's the loneliness. You sit in a room with 10 other people, all hooked up, all silent, all wondering if today's the day they don't make it home. The nurses are nice, but they're overworked. The TV is always on, but no one watches it. You don't talk about your kids, your dreams, your regrets. You just breathe. And wait. And hope the machine doesn't alarm. And then you do it again in three days. And again. And again. And you start to forget what your own voice sounds like. Transplant isn't just a medical choice - it's a chance to remember who you were before you became a patient.
my cousin got a kidney from a stranger in canada
they met for coffee after the surgery
he said 'thank you' and the donor just smiled and said 'you're welcome, now go live'
that’s the kind of humanity we need more of
not politics, not profit - just human to human
we can do better