When it comes to preventing heart attacks and strokes, knowing your risk isn’t just helpful-it’s life-saving. But how do you turn a list of numbers-cholesterol, blood pressure, age, smoking status-into a real decision about your health? That’s where the ASCVD risk calculator comes in. It’s not magic. It’s math. And it’s the most widely used tool doctors in the U.S. rely on to decide if you need a statin, lifestyle changes, or something more.
What Exactly Is the ASCVD Risk Calculator?
The ASCVD Risk Estimator, developed by the American College of Cardiology and the American Heart Association in 2013 and updated in 2018, is a simple tool that answers one question: What’s your chance of having a heart attack or stroke in the next 10 years? It’s built on data from over 60 years of studies-Framingham, MESA, ARIC, and others-tracking hundreds of thousands of people across different races and genders.
You don’t need a lab coat to use it. Just nine pieces of information:
- Your age (must be between 40 and 79)
- Sex
- Race (White, Black, Hispanic, or Asian)
- Total cholesterol
- HDL (good) cholesterol
- Systolic blood pressure
- Whether you’re on blood pressure meds
- If you have diabetes
- Whether you currently smoke
Plug those in, and it spits out a percentage. Under 5%? You’re low risk. Between 5% and 7.4%? Borderline. 7.5% to 19.9%? That’s intermediate-where things get tricky. 20% or higher? High risk. That’s when guidelines say you should be on a statin, unless there’s a strong reason not to.
Why It Matters More Than You Think
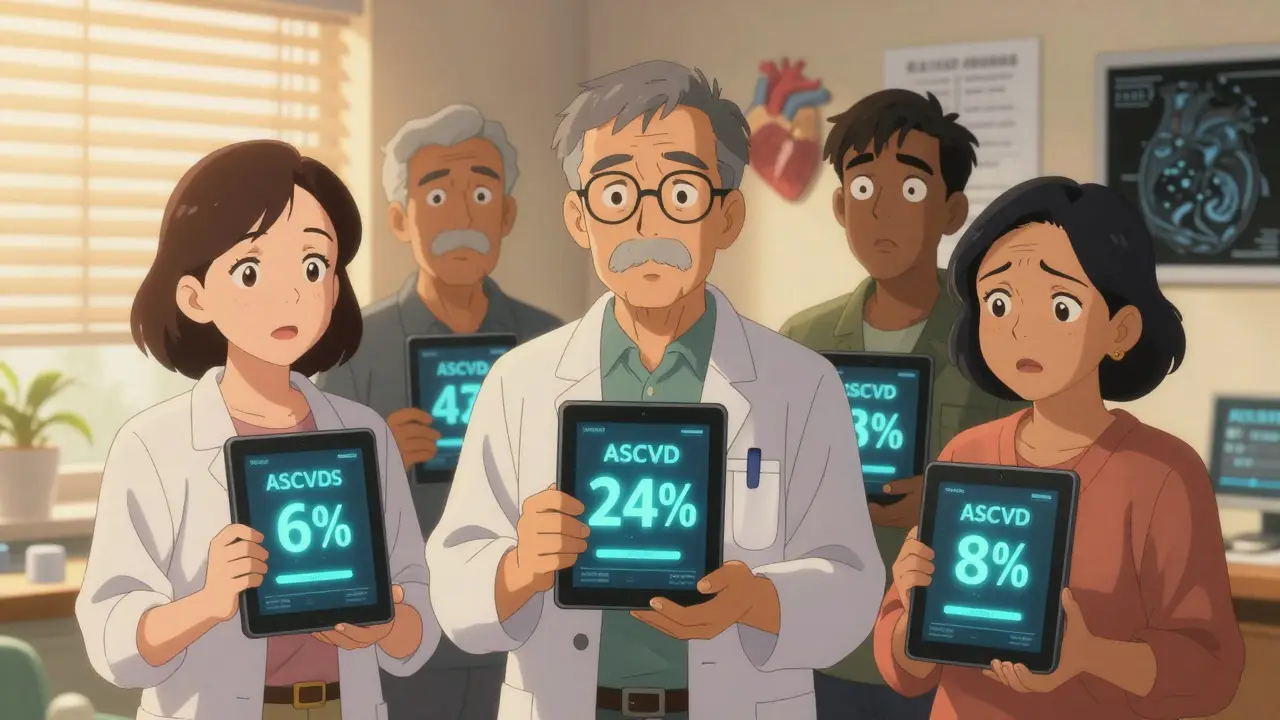
Most people think heart disease is about cholesterol alone. But the ASCVD calculator shows it’s about the full picture. A 52-year-old man with normal cholesterol but high blood pressure, diabetes, and a smoking habit might have a 24% 10-year risk. That’s higher than a 68-year-old with slightly elevated cholesterol but no other risks.
This matters because treatment isn’t one-size-fits-all. If your 10-year risk is below 7.5%, lifestyle changes-cutting sugar, walking daily, quitting smoking-are your main tools. At 7.5% or above, guidelines say moderate-intensity statins should be considered. At 20% or higher, high-intensity statins are recommended. That’s not opinion. That’s based on clinical trials showing statins reduce heart attacks by 25-35% in those groups.
And here’s the kicker: 35-40% of people aged 40-75 fall into that messy middle zone-7.5% to 19.9%. That’s where doctors get stuck. Is it enough to just tell them to eat better? Or should they start a pill? That’s why so many now turn to the next layer: coronary artery calcium (CAC) scoring.
The Hidden Power of CAC Scoring
If your ASCVD score says you’re intermediate risk, your doctor might suggest a CAC scan. It’s a quick, non-invasive CT scan that measures calcium buildup in your heart arteries. No dye. No needles. Just a few seconds in the machine.
Why does this help? Because calcium = plaque. And plaque = risk. A CAC score of zero means you have almost no plaque. That’s rare for someone over 50, but if you’re a smoker with a 12% ASCVD score and a CAC of zero? Your real risk is probably closer to 5%. You might not need a statin yet.
On the flip side, a CAC score over 100-even if your ASCVD score is only 10%-means you’ve got significant plaque. Your risk is much higher than the calculator says. In fact, studies show CAC scoring changes treatment plans in 68% of intermediate-risk patients. The Cleveland Clinic found it reclassifies 52% of them into either low or high risk, making decisions clearer.
This isn’t experimental. The 2022 ACC guidelines give CAC scoring a Class I recommendation-meaning it’s strongly supported-for exactly this group.

Where the Calculator Falls Short
It’s not perfect. And you need to know why.
The original data used to build the ASCVD calculator came mostly from White and Black populations. That means it doesn’t capture risk as accurately for everyone. For example:
- It underestimates risk by 15-25% for American Indians, South Asian Americans, and Puerto Ricans.
- It overestimates risk by 10-20% for East Asian Americans and Mexican Americans.
That’s not a small error. If you’re a 55-year-old South Asian woman with a family history of early heart disease, your ASCVD score might say 8%. But your real risk could be 12%. That changes whether you get a statin.
That’s why newer tools are emerging. The South Asian Risk (SAFR) score, developed in 2016, includes factors like waist-to-hip ratio and family history of early heart disease-things the ASCVD tool ignores. Puerto Rico’s own risk calculator, launched in 2019, adjusts for local diet patterns and genetic factors.
And it’s not just ethnicity. The ASCVD calculator doesn’t include lipoprotein(a)-a genetic cholesterol particle that’s a major independent risk factor. Or high-sensitivity CRP, which measures inflammation. Or your family history beyond diabetes and early heart attacks in parents.
What Experts Really Say About Using It
Doctors aren’t supposed to treat numbers. They’re supposed to treat people.
Dr. Donald Lloyd-Jones, who helped create the guidelines, says the calculator is a starting point for a conversation-not a final answer. Dr. Roger Blumenthal at Johns Hopkins calls it a dynamic tool that needs to evolve as we learn more.
Here’s what the Mayo Clinic says clearly: “Results should not be used alone to determine medical treatment.”
That means if your score says 11%, but you’ve had three family members die of heart attacks before 60, you’re likely higher risk than the number suggests. If you’re a 45-year-old woman with prediabetes, high triglycerides, and a sedentary job, your lifetime risk might be sky-high-even if your 10-year score is only 6%.
That’s why lifetime risk matters. About 78% of heart events happen in people whose 10-year risk is under 20%. So if you’re under 55 and your 10-year score is borderline or intermediate, your doctor should also look at your lifetime risk. That’s where prevention really starts.
What Happens After the Number?
Let’s say your ASCVD score is 14%. What now?
- First: Confirm your numbers. Did you report your smoking status correctly? (Studies show 22% of people misreport this.) Was your blood pressure taken properly? (Inconsistent readings can add 8-12 mm Hg of error.)
- Second: Ask about CAC scoring. It’s often covered by insurance if you’re in the intermediate range.
- Third: Talk about lifestyle. Even if you’re on a statin, diet and exercise still matter. Walking 30 minutes a day cuts risk by 20%. Cutting added sugar reduces triglycerides and inflammation.
- Fourth: Consider other tests. If your CAC is high, your doctor might check your lipoprotein(a) or hsCRP.
And here’s something most people don’t know: since 2014, the use of statins has gone up 27% because of these calculators. But only 58% of people who should be on them actually are. Why? Because doctors still rely on gut feeling, not numbers. Or patients refuse pills because they think they’re “fine.”
The Future: Beyond the Calculator
The next generation of risk tools is already here.
The American Heart Association’s PREVENT Online Calculator, launched in January 2023, now includes social factors: neighborhood poverty levels, food access, and education. Why? Because living in a food desert or working two jobs with no time to cook raises your heart risk by 23%, independent of cholesterol.
And then there’s genetics. The UK Biobank study showed that adding a polygenic risk score-based on 6.6 million genetic markers-improves prediction accuracy by 14.3% in intermediate-risk patients. Imagine a future where your risk score includes your DNA, your lifestyle, your environment, and your calcium score-all in one place.
For now, the ASCVD calculator is your best starting point. It’s not perfect. But it’s better than guessing.
Frequently Asked Questions
Can I use the ASCVD calculator if I’m under 40 or over 79?
No. The calculator is only validated for people aged 40 to 79. If you’re younger, your risk is likely low, but family history, diabetes, or severe high cholesterol could still mean you need attention. If you’re over 79, your risk is already high by age alone-so doctors focus on overall health and symptoms instead of the calculator.
Is the ASCVD calculator accurate for non-American populations?
It’s less accurate for people of South Asian, Indigenous, or Puerto Rican descent, where it underestimates risk. For East Asians and Mexican Americans, it may overestimate. If you’re from one of these groups, ask your doctor about ethnicity-specific tools like the SAFR score or local risk calculators. Don’t rely on the standard calculator alone.
Do I need a statin if my ASCVD score is 8%?
Guidelines say yes, if you’re between 40 and 75 and have no other reasons to avoid it. But it’s not automatic. Your doctor should discuss your lifestyle, family history, and whether a CAC scan would help clarify your risk. Some people with an 8% score choose to start with diet and exercise first-especially if they’re young and otherwise healthy.
Can I calculate my ASCVD risk myself?
Yes. The American College of Cardiology offers a free online tool called the ASCVD Risk Estimator Plus. You can find it by searching for “ACC ASCVD Risk Calculator.” Just make sure you have your latest cholesterol and blood pressure numbers handy. But remember-it’s for discussion with your doctor, not a final diagnosis.
Why does my doctor want a CAC scan if I’m already on a statin?
Sometimes, even if you’re on a statin, your doctor wants to see how much plaque is still building up. A CAC scan can show if the treatment is working-or if you need something stronger. It’s not about starting treatment. It’s about fine-tuning it.
What to Do Next
If you’re between 40 and 79, ask your doctor for your ASCVD score at your next checkup. Don’t wait for them to bring it up-ask. If you’re in the intermediate range, ask about a CAC scan. If you’re under 40, know your numbers anyway: cholesterol, blood pressure, and whether you smoke. If you’re over 79, focus on staying active and managing conditions like diabetes or high blood pressure.
Heart disease doesn’t strike suddenly. It builds over years. The ASCVD calculator helps you see the buildup before it’s too late. Use it. Talk about it. Don’t let a number scare you. Let it guide you.




This is actually super helpful. I never knew my risk could be so different just by adding smoking + BP. I'm 47, Nigerian, and my doc just gave me a 9%... but I smoke and my dad died at 54. I'm getting a CAC scan next week. 🙏
Oh sweet mercy. Another tool that tells me I'm 'intermediate risk' while ignoring that I live in a food desert, work 12-hour shifts, and my only 'exercise' is walking to the fridge. 🙄 The calculator doesn't care that my neighborhood has more liquor stores than grocery stores. Thanks, ACC.
I appreciate the nuance here-especially the CAC point. But I must say: the reliance on race-based algorithms still makes me uneasy. It’s not that the data isn’t useful-it’s that we’re still using crude proxies for genetic and socioeconomic risk. We need better. And yes, I’m a Brit, but I’ve seen this in the NHS too. 😕
Let’s be real: the ASCVD calculator is just a glorified Excel sheet built on 1980s data and white-coat arrogance. Meanwhile, my lipidologist uses lipoprotein(a), apoB, and coronary calcium-and laughs at the 7.5% threshold like it’s a kindergarten math test. If your doctor still uses this without checking your actual plaque, they’re practicing medicine in the Stone Age. 🧪
Lipoprotein(a) not included? HsCRP? Polygenic scores? Bro. The calculator is outdated. Like, 2013 outdated. My doc ran it and said 'statin.' I asked about apoB. He said 'what's that?' 😴
The notion that a risk calculator-designed primarily on cohort data from the American Midwest-can accurately predict cardiovascular outcomes across global populations is, frankly, a statistical fallacy of the highest order. One cannot ethically apply a model calibrated on a non-representative sample to heterogeneous demographics without acknowledging systemic bias. The guidelines, while well-intentioned, are fundamentally flawed.
They’re using this to push statins so Big Pharma can make billions. 😡 I read a Reddit thread where a guy said his doc told him he was 'intermediate risk'-then he got a CAC scan and it was ZERO. Next thing he knew, he was getting billed for a $2000 'preventive protocol.' This isn’t medicine-it’s a racket. 🇺🇸🇨🇦🇪🇺
Yo from Lagos-just wanted to say this hit different. My cousin in India got his ASCVD score and it was 7%. He’s got a waist-to-hip ratio of 0.98 and his uncle had a heart attack at 48. He didn’t get a statin. He started walking 5K every morning and eating millet instead of white rice. Two years later? His CAC is zero. The calculator didn’t see that. But he did.
Wait-so if you’re a Black woman with diabetes and high BP, the calculator says you’re 'intermediate risk'... but if you’re a white guy with the same numbers, you’re 'high risk'? That’s not science. That’s systemic bias dressed up as math. And now they want us to pay for a CAC scan to fix their broken algorithm? No. Just no.
I’ve been telling my patients for years: numbers are a map, not the territory. I had a 58-year-old woman with a 12% score and a CAC of 0. She quit smoking, started yoga, and now her LDL is 78. No statin needed. The calculator didn’t predict her willpower. But she did. And that’s what matters. 🙌