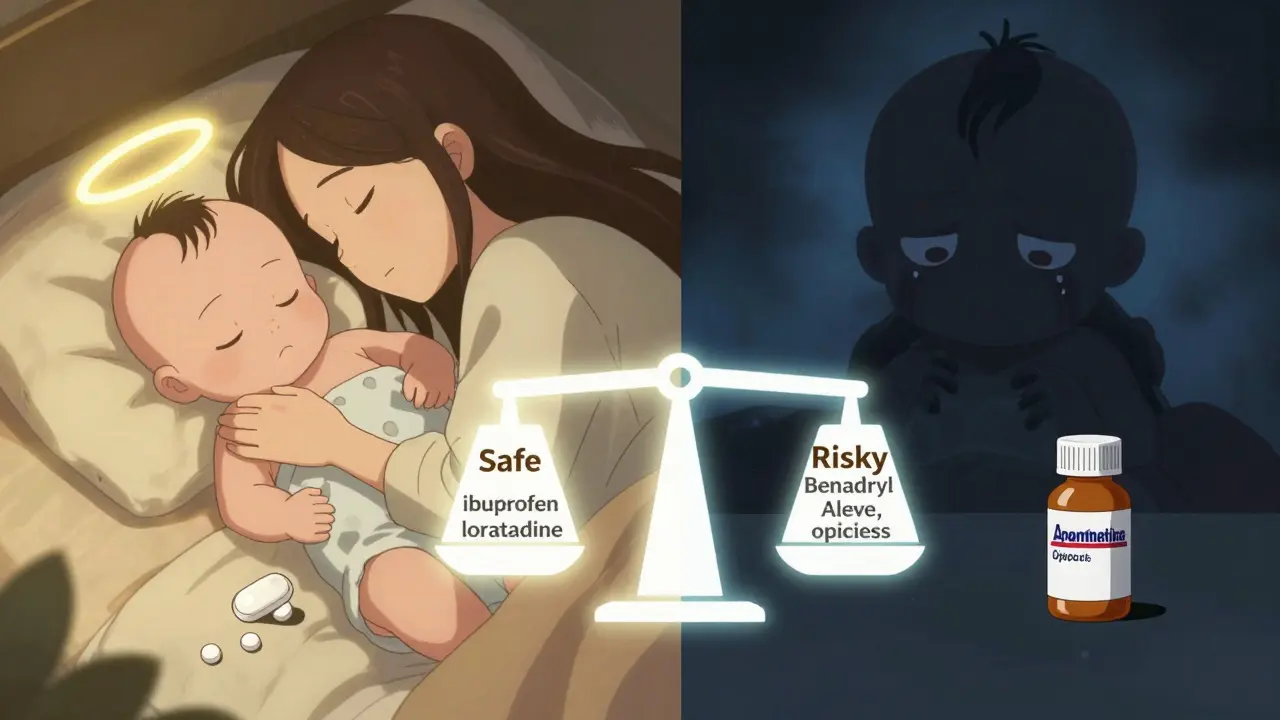
When you’re nursing and hit by allergies or a headache, the last thing you want is to choose between feeling better and protecting your baby. The good news? Many common medications are perfectly safe - if you pick the right ones. The wrong choice? It can leave your baby drowsy, fussy, or even struggling to feed. So what actually works without risk? Let’s cut through the confusion with clear, evidence-backed facts.
Which Antihistamines Are Safe While Nursing?
Not all antihistamines are created equal. The big divide is between first-generation and second-generation drugs. First-gen antihistamines - like diphenhydramine (Benadryl), chlorpheniramine, and promethazine - are the ones you might reach for because they’re cheap and fast-acting. But they come with a hidden cost: they cross into breast milk easily and can make your baby sleepy, sluggish, or even cause feeding problems. One study found that infants of mothers using diphenhydramine regularly had lower milk intake and longer sleep cycles, which can lead to poor weight gain over time.
Second-generation antihistamines are the clear winners for nursing moms. Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are the top picks. Why? They’re designed not to cross the blood-brain barrier, which means they don’t cause drowsiness in you - or your baby. According to LactMed, loratadine transfers to breast milk at just 0.04% of the maternal dose. Fexofenadine? Even lower at 0.02%. That’s practically negligible. These drugs also have long half-lives, meaning you can take them once a day and still stay protected. No need to time doses around feedings.
What about older advice that said “antihistamines are contraindicated”? That’s outdated. A 2022 review from the American Academy of Family Physicians confirmed that second-gen antihistamines show no adverse effects in over 200,000 breastfeeding cases. The old warnings came from limited data and anecdotal reports. Today’s guidelines are based on real-world outcomes, not fear.
Best Pain Relievers for Nursing Moms
Pain relief is simpler than you think. Two drugs dominate the safe list: acetaminophen (Tylenol) and ibuprofen (Advil, Motrin). Both are low-risk and widely recommended by pediatricians and lactation consultants.
Acetaminophen reaches breast milk at about 1-2% of your dose. It’s been studied in thousands of nursing mothers with zero reports of harm to infants. You can take it regularly - even daily - if needed for headaches, postpartum pain, or dental work. Ibuprofen is even better in some ways. It transfers at only 0.6-0.8% of your dose, has a short half-life (just 2 hours), and binds tightly to proteins in your blood, leaving little free drug to enter milk. Studies show no impact on infant growth or development, even with long-term use.
Now, what about the others? Naproxen (Aleve) is a no-go for regular use. It sticks around longer - up to 17 hours - and transfers at 7% of your dose. There are documented cases of infants developing anemia or vomiting after prolonged exposure. Opioids like codeine, hydrocodone, and tramadol? Avoid them. Codeine, in particular, can be metabolized differently in some mothers, leading to dangerous morphine levels in breast milk. Even morphine, while sometimes used after C-sections, should only be given in single doses under medical supervision.

What About OTC Cold and Allergy Mixes?
This is where most nursing moms get tripped up. You grab a bottle labeled “Day & Night Cold Relief” or “Allergy & Sinus,” and suddenly you’re getting a double dose of antihistamine - plus decongestants, cough suppressants, and sometimes alcohol. Many of these combos contain diphenhydramine or chlorpheniramine, even if the label doesn’t scream it.
Always read the active ingredients. If you see “diphenhydramine,” “doxylamine,” or “chlorpheniramine,” put it back. Stick to single-ingredient options. Need allergy relief? Get loratadine alone. Need pain relief? Get plain ibuprofen. If you’re unsure, ask your pharmacist - they’re trained to spot hidden antihistamines in multi-symptom products.
Also, watch for hidden alcohol. Some liquid cold remedies contain ethanol. Even small amounts can affect your baby’s developing nervous system. Choose tablets or capsules instead.
When to Be Extra Cautious
Even safe drugs need careful use if you have certain health conditions. If you have liver or kidney problems, your body processes these drugs slower. That means higher levels build up in your milk. Talk to your doctor before taking anything regularly if you have chronic illness.
Also, watch your baby. If you take a new medication and notice your baby is unusually sleepy, feeding less, or seems fussy, stop the drug and call your pediatrician. It doesn’t mean the drug is unsafe - it just means your baby might be extra sensitive. Most reactions are mild and go away once you stop.
Don’t assume “natural” or “herbal” means safe. Some herbal antihistamines, like butterbur or stinging nettle, lack safety data in breastfeeding. Stick to well-studied pharmaceuticals.
Real-World Tips for Safe Medication Use
- Take meds right after a feeding - not before. That gives your body time to clear the drug before the next nursing session.
- Use the lowest effective dose. You don’t need to take two tablets if one works.
- Keep a log: write down what you took, when, and how your baby reacted. This helps spot patterns.
- Never combine multiple OTC meds. One antihistamine is enough. Adding another doesn’t make it work better - it just increases risk.
- Ask your pharmacist: “Is this safe while breastfeeding?” They’re your best ally.
Most importantly - don’t suffer in silence. Allergies and pain are real, and you deserve relief. The right meds won’t harm your baby. In fact, feeling better means you’ll be more present, more rested, and better able to care for your child.
Is it safe to take Zyrtec (cetirizine) while breastfeeding?
Yes, cetirizine (Zyrtec) is considered one of the safest antihistamines for nursing mothers. Studies show it transfers to breast milk in very small amounts - less than 1% of the maternal dose - with no reported side effects in infants. It’s non-sedating for both mother and baby, making it ideal for daily use.
Can I take Benadryl (diphenhydramine) while breastfeeding?
Benadryl is not recommended for regular use while breastfeeding. While occasional use is unlikely to cause harm, diphenhydramine can make babies drowsy, reduce milk supply, and interfere with feeding patterns. It’s better to use a second-generation antihistamine like loratadine or cetirizine instead.
Is ibuprofen safe for long-term use while nursing?
Yes, ibuprofen is safe for long-term use while breastfeeding. It has a short half-life, low transfer into milk (under 1%), and no documented effects on infant development. Many mothers take it daily for postpartum pain, migraines, or arthritis without issue.
What pain reliever should I avoid while breastfeeding?
Avoid naproxen (Aleve) for regular use - it transfers into milk at higher levels and can cause anemia or vomiting in infants. Also avoid opioids like codeine, tramadol, and hydrocodone due to unpredictable metabolism and risk of infant sedation. Stick to acetaminophen or ibuprofen instead.
Do antihistamines reduce milk supply?
First-generation antihistamines like diphenhydramine and chlorpheniramine may reduce milk supply in some women, especially with frequent or high-dose use. This is likely due to their anticholinergic effects. Second-generation antihistamines like loratadine and cetirizine do not affect milk production and are preferred for this reason.



From a pharmacokinetic standpoint, second-generation H1-antihistamines like cetirizine and loratadine exhibit negligible placental transfer and minimal mammary excretion due to their high plasma protein binding (>80%) and low lipophilicity (logP < 2). The maternal-to-infant milk-to-plasma ratio for cetirizine is approximately 0.04, well below the threshold for clinical concern (<0.1). This aligns with LactMed’s evidence-based classification as ‘L1: Safest.’
Conversely, first-gen agents like diphenhydramine demonstrate higher lipophilicity (logP ~3.9), facilitating passive diffusion into breast milk. Their anticholinergic activity also suppresses prolactin signaling via muscarinic receptor antagonism - a documented mechanism for reduced milk volume in longitudinal studies.
For analgesia, ibuprofen’s low milk transfer (<0.8%) and rapid clearance (t½ = 2h) make it ideal. Its protein binding exceeds 99%, leaving virtually no free fraction to enter milk. Acetaminophen, while slightly more transferred (~1.5%), lacks metabolites of concern and has a 20-year safety record in neonates.
OPINION: Avoiding combination OTC products isn’t just prudent - it’s pharmacologically essential. Many contain pseudoephedrine (a vasoconstrictor) or doxylamine (a potent anticholinergic), both of which independently suppress lactation. Stick to monotherapy. Always.
As a lactation consultant, I see so many moms panic over meds they don’t need to avoid. The science is clear: loratadine and cetirizine are not just ‘safe’ - they’re optimal. I’ve had patients on daily Zyrtec for years with zero issues. Their babies are alert, feeding well, gaining weight. No drowsiness. No fussiness.
And ibuprofen? It’s practically the gold standard. I recommend it over acetaminophen for postpartum pain because it’s anti-inflammatory too - helps with swelling, perineal healing, even mastitis. Plus, it’s gentler on the liver.
Pro tip: Take meds right after nursing. Even better, pump and dump if you’re really nervous - though you almost never need to. Your baby’s not getting a hit of morphine from a single Advil.
You’ve got this. You’re not failing your baby by taking care of yourself. You’re doing the opposite.
Thank you for this. Seriously. 🙏
I was about to grab a NyQuil because my sinuses were killing me - then I remembered reading somewhere that it had diphenhydramine. I almost made a terrible mistake.
Now I’ve got my Claritin and ibuprofen on standby. No more guessing. No more fear.
You’re right - feeling better means I can be the mom I want to be. 😊
Stick to single ingredients. Always.
LMAO. You people are so scared of medicine. ‘Oh no, my baby might get 0.02% of a drug!’ Meanwhile, half of you are chugging kombucha with live cultures and eating raw honey because ‘natural.’
Here’s the truth: your baby’s been exposed to more toxins in your breast milk from environmental pollutants than from any FDA-approved OTC med. You’re not protecting your kid - you’re performing performative parenting.
And don’t even get me started on ‘lactation consultants.’ Most of them are certified by a guy who runs a blog out of his basement. Read the actual studies. Not the Instagram summaries.
Take the damn Zyrtec. And if you’re worried? Pump and dump. Or better yet - stop obsessing and live your life.
While the general tenor of this article is commendable, one must acknowledge the epistemological limitations of extrapolating pharmacokinetic data derived from healthy, term neonates to preterm infants or those with metabolic disorders such as UDP-glucuronosyltransferase deficiency.
Furthermore, the conflation of ‘safety’ with ‘absence of adverse reports’ risks committing the fallacy of argumentum ad ignorantiam. The absence of evidence is not evidence of absence - particularly when longitudinal studies exceeding five years remain scarce.
One must also interrogate the commercial incentives behind the promotion of second-generation antihistamines, which are now off-patent and thus favored by institutional guidelines not due to superior efficacy, but due to cost-effectiveness.
Prudence, not convenience, should guide maternal pharmacotherapy.
Thank you for writing this - I needed this so badly. 💕
I had a baby with reflux and was terrified to take anything. I thought Benadryl was fine because ‘it’s just for allergies.’ Turns out, it made her so sleepy she’d fall asleep mid-feed. Took me three weeks to realize what was going on.
Switched to Zyrtec. She’s been a different baby. Alert. Hungry. Happy.
Also, ibuprofen changed my life. My postpartum pain was brutal. I thought I had to ‘tough it out.’ Nope. Two pills a day and I could actually hold her without crying.
You’re not weak for needing help. You’re wise. And you’re doing amazing.
Let’s be honest - this is just pharmaceutical industry propaganda dressed as ‘evidence.’
Second-gen antihistamines? They’re cheaper to produce. That’s why they’re ‘recommended.’
And ibuprofen? Did you know it’s linked to premature closure of the ductus arteriosus in utero? Now you’re telling me it’s safe for infants? Please.
Real mothers used to rely on rest, hydration, and herbal teas. Now we’re medicating our babies with synthetic chemicals because we’re too lazy to breathe steam.
Also, your ‘pharmacist’? Probably on commission. Ask your OB. Or better yet - go to a naturopath. They actually care about your baby.
Stop trusting Big Pharma. Start trusting your instincts.
It’s irresponsible to say these drugs are ‘safe’ without mentioning that every medication has potential side effects - even if rare.
What about the baby who develops a rash? Or the one who becomes lethargic? What if the mother has a genetic variation that alters metabolism?
This article reads like a marketing brochure. ‘Just take Zyrtec and you’ll be fine.’
But what if you’re the one in 10,000? What then?
I’d rather suffer quietly than risk my child’s health on a statistical average.
OH MY GOD YES. 🙌
I took Benadryl for three days last month. My baby went from feeding every 2 hours to sleeping 6 hours straight. I thought she was ‘sleeping like a angel.’ Turns out, she was drugged. And I didn’t even know it.
Switched to Zyrtec. She’s back to her old self - hungry, squirmy, and obsessed with my boob. Perfect.
Also - I used to take Aleve for my back pain. Then I read about the anemia risk. I stopped cold. Now I take ibuprofen. No issues. No guilt. No drama.
If you’re still using combo cold meds? Stop. Right now. Go read the label. If it says ‘antihistamine’ - it’s probably diphenhydramine. Put it back.
You’re not being paranoid. You’re being a good mom. And you deserve to feel better - safely.