TNF Inhibitors: What They Are, How They Work, and Which Conditions They Treat
When your immune system goes rogue and starts attacking your own body, TNF inhibitors, a class of biologic drugs that block tumor necrosis factor, a key protein driving inflammation. Also known as anti-TNF agents, they’re one of the most targeted treatments we have for autoimmune diseases. These drugs don’t just ease symptoms—they change the course of diseases like rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease by silencing a specific inflammatory signal your body can’t turn off on its own.
TNF inhibitors work by locking onto TNF-alpha, a signaling molecule that tells immune cells to ramp up inflammation. In healthy people, this helps fight infection. In autoimmune conditions, TNF-alpha is stuck in overdrive, causing joint damage, gut inflammation, and skin plaques. Drugs like adalimumab, infliximab, and etanercept act like molecular sponges, soaking up excess TNF-alpha before it can trigger damage. This isn’t guesswork—it’s precision medicine. People who’ve tried standard drugs like methotrexate and still struggle with pain or flare-ups often find real relief with these. But they’re not magic pills. They require injections or infusions, cost thousands a year, and can raise infection risk. That’s why they’re usually reserved for moderate to severe cases.
These drugs are part of a bigger picture. They’re closely tied to autoimmune diseases, conditions where the immune system mistakenly targets healthy tissue, including ulcerative colitis, ankylosing spondylitis, and plaque psoriasis. They’re also connected to biologic drugs, medications made from living cells, designed to target specific parts of the immune system, which include other classes like IL-17 or JAK inhibitors. Unlike older drugs that suppress the whole immune system, TNF inhibitors are more selective. But they’re not the only option—some patients switch to other biologics when TNF blockers stop working or cause side effects.
You’ll find posts here that dig into how these drugs interact with other meds, why some people need to take them long-term, and how lifestyle changes like diet and stress management can support treatment. You’ll also see how they compare to alternatives like corticosteroids or traditional DMARDs, and why some patients end up on separate pills instead of combo packs. There’s no one-size-fits-all answer. What works for someone with severe rheumatoid arthritis might not help someone with psoriasis, and side effects can vary widely. The goal isn’t just to treat the disease—it’s to help you live better, with less pain, fewer flares, and more control over your health.
TNF Inhibitors and Cancer Risk: What You Need to Know About Biologics and Immunosuppression
TNF inhibitors help control autoimmune diseases but raise concerns about cancer risk. This article breaks down the real data on skin cancer, lymphoma, and survival rates - and what you should do before starting treatment.
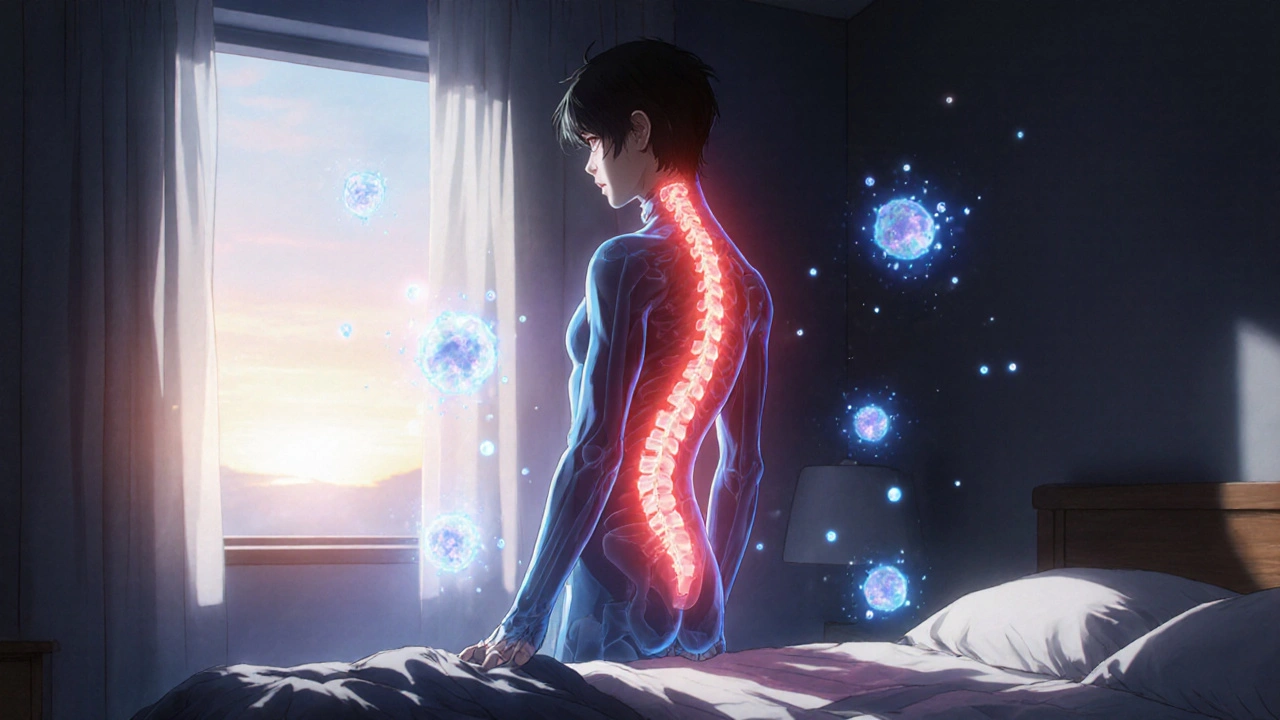
Ankylosing Spondylitis: How TNF Inhibitors Reduce Spine Inflammation and Improve Daily Life
Ankylosing spondylitis causes chronic spine inflammation and stiffness. TNF inhibitors like Humira and Enbrel target the root cause, reducing pain, slowing bone fusion, and improving mobility for most patients. Learn how they work and who benefits most.