Proton Pump Inhibitors: What They Are, How They Work, and What You Need to Know
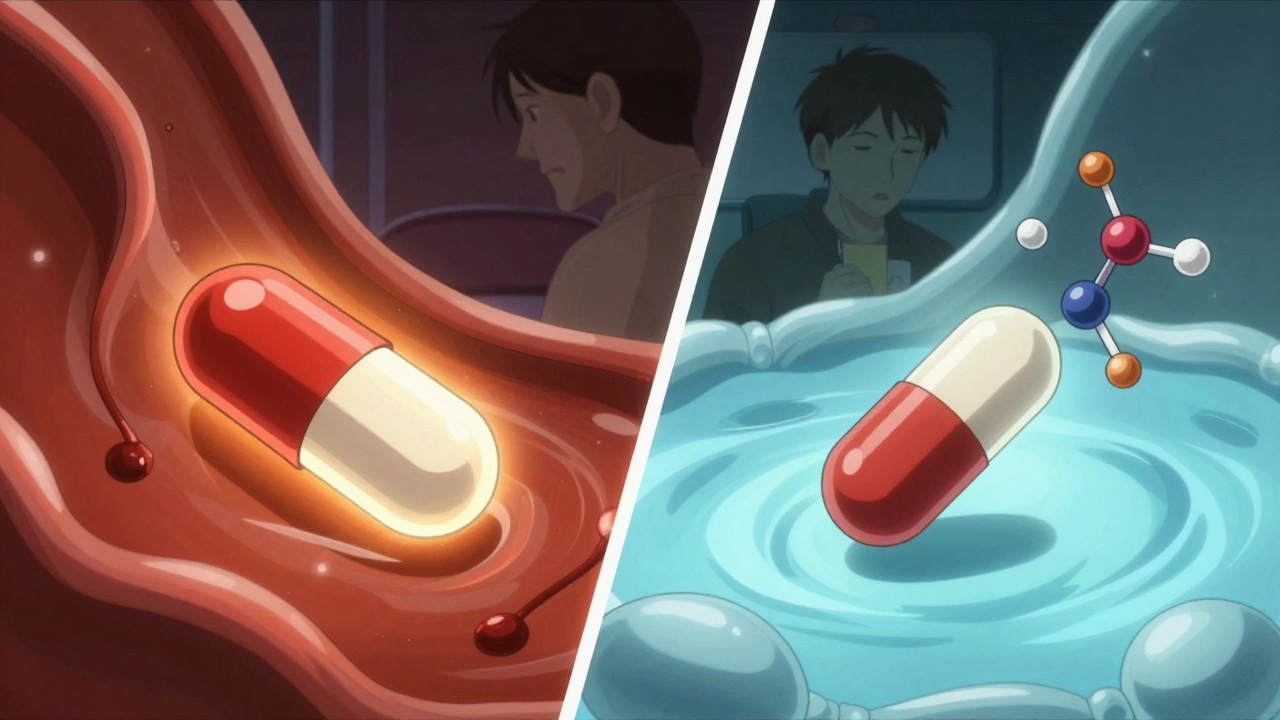
When you hear proton pump inhibitors, a class of medications that block acid production in the stomach. Also known as PPIs, they’re among the most prescribed drugs in the world—for good reason. If you’ve ever had heartburn that wouldn’t quit, or been told you have GERD or an ulcer, chances are you’ve taken one. These drugs don’t just mask symptoms—they shut down the source of the problem by targeting the proton pumps in your stomach lining, the tiny valves that release acid after you eat.
But here’s the catch: PPIs aren’t harmless. Long-term use has been linked to kidney issues, bone loss, and even an increased risk of certain infections. And while they work fast—often relieving pain within days—they’re not meant to be taken forever. Many people stay on them way longer than needed because the symptoms come back the moment they stop. That’s not failure—it’s a sign the root cause wasn’t addressed. The real question isn’t just whether PPIs work, but whether they’re the right tool for your situation.
Related to this are GERD, a chronic condition where stomach acid flows back into the esophagus, and stomach acid, the powerful digestive fluid your body produces to break down food. These aren’t just medical terms—they’re part of your daily life. If you’ve ever felt that burning sensation after spicy food, or woke up with a sour taste in your mouth, you’ve felt the impact of uncontrolled acid. And while PPIs silence that signal, they don’t fix why it’s happening in the first place.
Some people use PPIs for occasional heartburn. Others take them daily for years. The posts below show you the full picture: how these drugs interact with other medications, what happens when you stop them cold, why some people never get relief even on high doses, and what alternatives—like diet changes, H2 blockers, or even lifestyle shifts—might work better for you. You’ll also find real stories about side effects, unexpected risks, and how to talk to your doctor about cutting back safely.
There’s no one-size-fits-all answer here. What works for someone with a bleeding ulcer might be overkill for someone with occasional indigestion. The goal isn’t to scare you off PPIs—it’s to help you understand when they’re necessary, when they’re not, and how to take control of your digestive health without relying on a pill you didn’t ask for in the first place.
Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption and Effectiveness
Proton pump inhibitors can severely reduce absorption of key antifungals like itraconazole and ketoconazole, leading to treatment failure. Fluconazole is safer, but interactions with liver enzymes still matter. New research hints PPIs might even boost antifungal power in resistant infections.