Personalized Medicine: Tailored Treatments Based on Your Genetics and Lifestyle
When you hear personalized medicine, a healthcare approach that customizes treatment based on an individual’s genes, environment, and lifestyle. Also known as precision medicine, it moves away from the one-size-fits-all model and asks: What works for you? This isn’t science fiction—it’s happening right now in cancer clinics, psychiatric care, and even for common conditions like high blood pressure and diabetes.
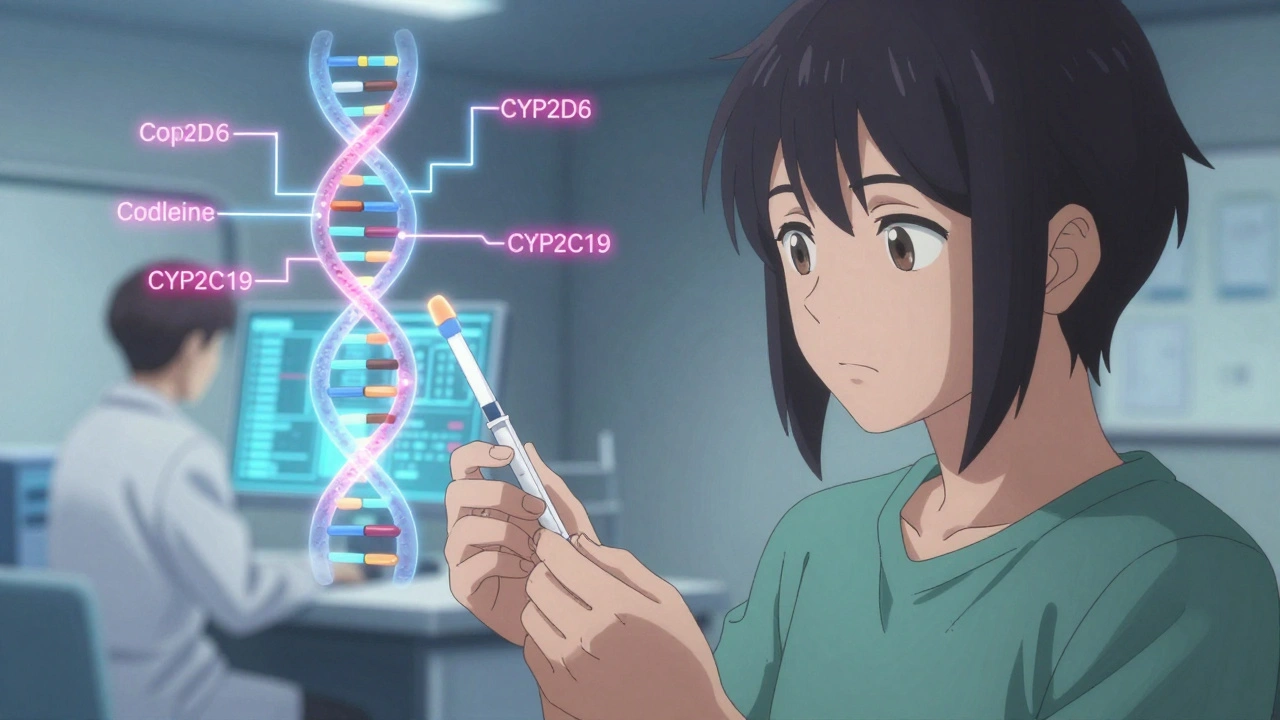
At the heart of personalized medicine is pharmacogenomics, the study of how your genes affect how your body processes drugs. Two people can take the same pill, but one gets relief while the other suffers side effects—or nothing at all. Why? Because of tiny differences in their DNA. For example, some people have a gene variant that makes them metabolize blood thinners too fast or too slow. Doctors can now test for these variants before prescribing, cutting trial-and-error and avoiding dangerous reactions. This same logic applies to antidepressants, pain meds, and even chemotherapy drugs. The goal isn’t just to treat disease—it’s to treat it right the first time.
Personalized medicine also looks beyond genes. Your diet, sleep, stress levels, and even your gut bacteria influence how medications work. That’s why someone with chronic inflammation might respond better to a biologic like a TNF inhibitor, a type of targeted therapy that blocks a specific protein driving inflammation—but only if their body produces too much of that protein. It’s why some people with depression need a different SSRI than others, not because their condition is different, but because their brain chemistry responds differently. Even something as simple as avoiding grapefruit with certain pills is part of this puzzle—because your body’s ability to break down drugs is shaped by more than just your genes.
You won’t find a single test that tells you everything. But you will find a growing number of tools that help doctors connect the dots: genetic reports, drug interaction checkers, wearable health trackers, and even AI that predicts how you’ll respond to a treatment. And as more data becomes available, treatments are becoming more precise. That’s why posts here cover everything from how personalized medicine affects opioid prescribing to why some generic drugs work better for certain people than others. You’ll find real stories about patients who avoided side effects, got better faster, or stopped guessing what works. This isn’t about future tech—it’s about using what’s already here to make your care smarter, safer, and more effective.
Pharmacogenomics Testing: How Your Genes Determine Which Medications Work for You
Pharmacogenomics testing uses your genes to predict how you'll respond to medications, reducing side effects and improving treatment success-especially for depression, heart disease, and pain management.