Genetic Drug Response: How Your DNA Affects Medication Effectiveness
When a drug works perfectly for one person but causes a bad reaction in another, it’s often not about dosage or luck—it’s about genetic drug response, how your inherited DNA influences the way your body processes and reacts to medications. Also known as pharmacogenomics, this field explains why two people taking the same pill at the same dose can have completely different outcomes. Your genes control the enzymes that break down drugs, the receptors they bind to, and even how your body eliminates them. This isn’t theoretical—it’s why some people need half a pill to feel relief while others need double the dose, and why others end up in the hospital from side effects that never affected anyone else.
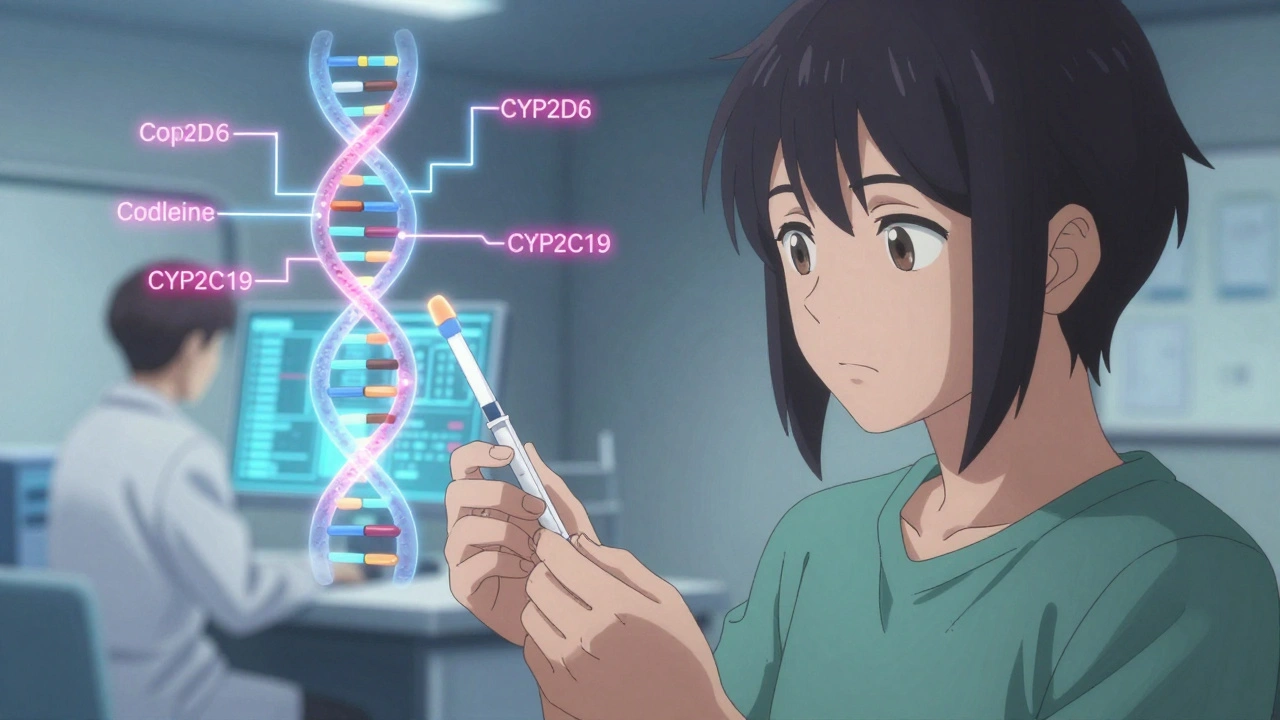
One of the biggest players here is the CYP450 enzyme system, a group of liver enzymes responsible for metabolizing over 90% of commonly prescribed drugs. If you have a variant that makes CYP3A4 or CYP2D6 work too fast, your medication might get cleared before it can help. If it works too slow, the drug builds up and turns toxic. This is why statins, antidepressants, blood thinners, and even painkillers can behave unpredictably across individuals. Another key factor is how your body handles personalized medicine, the practice of tailoring drug choices and doses based on genetic testing. Hospitals and clinics are starting to use genetic tests before prescribing certain drugs—not because it’s futuristic, but because it prevents hospitalizations and saves lives.
It’s not just about what works—it’s about what’s safe. Someone with a slow-metabolizer gene might get severe muscle pain from a common cholesterol drug, while another person with a fast-metabolizer gene gets no benefit at all. These differences aren’t rare. Studies show nearly 90% of people carry at least one genetic variant that affects how they respond to at least one medication. And yet, most doctors still prescribe based on weight, age, or symptoms alone. That’s changing, slowly. The science is solid. The tools are available. What’s missing is awareness.
Below, you’ll find real-world stories and science-backed insights on how genetic drug response shows up in everyday medicine—from why some people get itching from morphine while others don’t, to how grapefruit and antidepressants collide in your liver, to why certain heart meds are dangerous for some and lifesaving for others. These aren’t abstract concepts. They’re the reason your pills work—or don’t. And knowing how your genes play into this could change everything for your health.
Pharmacogenomics Testing: How Your Genes Determine Which Medications Work for You
Pharmacogenomics testing uses your genes to predict how you'll respond to medications, reducing side effects and improving treatment success-especially for depression, heart disease, and pain management.