Biologic Drugs: What They Are, How They Work, and What You Need to Know
When you hear biologic drugs, medications made from living organisms like cells or proteins, not chemicals in a lab. Also known as biologics, they’re designed to target specific parts of your immune system—unlike traditional pills that work broadly across the body. These aren’t your grandfather’s aspirin. Biologic drugs are engineered to block specific proteins that cause inflammation, making them powerful tools for conditions like rheumatoid arthritis, psoriasis, Crohn’s disease, and multiple sclerosis.
They’re made from living cells—often from bacteria, yeast, or animal cells grown in labs. One of the most common types is monoclonal antibodies, laboratory-made proteins that lock onto a single target in your body, like a key fitting into a lock. These can shut down the immune signals that turn healthy tissue into inflamed, damaged tissue. That’s why they work so well for autoimmune diseases: they don’t just calm your immune system—they surgically disable the parts causing the problem.
But they’re not magic. Because they’re so targeted, they can leave you vulnerable to infections. People on biologics get more colds, and sometimes serious ones like tuberculosis. They also cost way more than regular pills—often thousands a month. That’s why many patients switch between brands or look for biosimilars, which are cheaper copies of the original biologic. And unlike pills, you can’t swallow them. Most biologics are injected under the skin or given through an IV.
They’re not just for adults. Kids with severe juvenile arthritis and teens with Crohn’s are getting biologics too. But monitoring is key. These drugs don’t just change how your body fights disease—they can change how it grows, responds to vaccines, or even reacts to other meds. That’s why doctors check liver enzymes, blood counts, and infection history before starting them.
There’s also a growing list of targeted therapy, a category of treatments that focus on specific molecules involved in disease that overlaps with biologics. Think of it like upgrading from a shotgun to a sniper rifle. Traditional drugs spray everywhere. Biologics aim precisely. But precision means you need to know exactly what you’re shooting at—and what might happen if you miss.
You’ll find posts here that dig into how biologics interact with other drugs, why some patients get better results than others, and what to do if your insurance denies coverage. There are guides on managing side effects, comparing biosimilars to brand names, and even how diet and stress might affect how well they work. Some people swear by them. Others quit because of side effects. The truth? They’re not for everyone—but for the right person, they can change everything.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit for anyone taking, considering, or managing biologic drugs—whether you’re a patient, caregiver, or just trying to understand why your doctor recommended one.
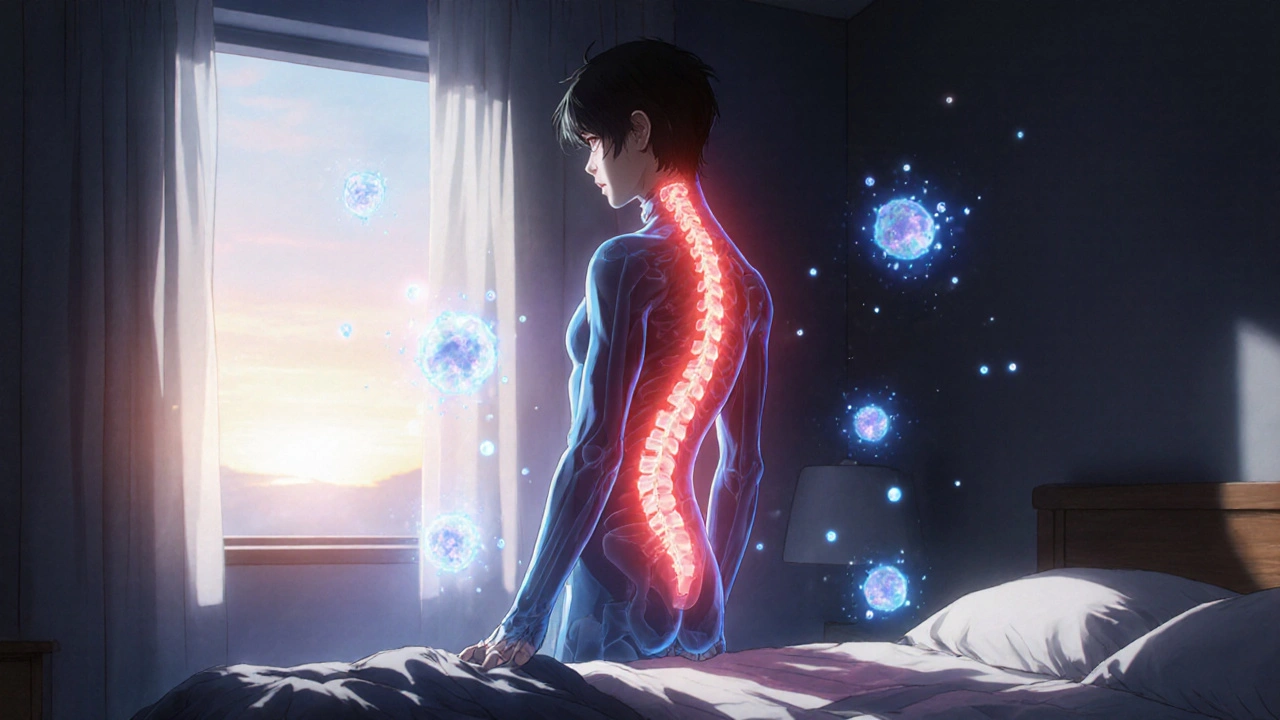
Ankylosing Spondylitis: How TNF Inhibitors Reduce Spine Inflammation and Improve Daily Life
Ankylosing spondylitis causes chronic spine inflammation and stiffness. TNF inhibitors like Humira and Enbrel target the root cause, reducing pain, slowing bone fusion, and improving mobility for most patients. Learn how they work and who benefits most.