Autoimmune Disease Medications: What Works, What Risks, and What You Need to Know
When your body turns on itself, autoimmune disease medications, drugs designed to calm an overactive immune system that attacks healthy tissue. Also known as immunomodulators, these treatments don’t cure the disease—they help you live with it without constant pain, swelling, or damage to your organs. Conditions like rheumatoid arthritis, lupus, Crohn’s disease, and ankylosing spondylitis aren’t just inconvenient—they can be disabling. That’s where these drugs step in, targeting the root cause instead of just masking symptoms.
Not all autoimmune disease medications are the same. TNF inhibitors, a class of biologic drugs that block tumor necrosis factor, a protein driving inflammation. Also known as anti-TNF agents, they include Humira, Enbrel, and Remicade—medications that have helped millions regain mobility and reduce joint damage. But they’re not magic. These drugs suppress your immune system, which means you’re more vulnerable to infections. Some studies show a small but real increase in skin cancer and lymphoma risk. That’s why doctors check for TB, hepatitis, and other hidden infections before starting treatment.
Biologics, lab-made proteins that mimic or block natural immune system signals. Also known as targeted therapies, they’re the next generation after older drugs like methotrexate. Unlike broad immunosuppressants, biologics are precise. Anti-IL-5 drugs like mepolizumab target only one type of immune cell, making them ideal for severe asthma tied to eosinophils. But they’re expensive, require injections or infusions, and don’t work for everyone. And because they’re so new, long-term side effects are still being tracked.
What you won’t find in most doctor’s brochures? How these drugs interact with everyday things. Grapefruit juice can mess with how your body breaks down some of them. Over-the-counter painkillers like ibuprofen can trigger dangerous flare-ups in people with Aspirin-Exacerbated Respiratory Disease. Even something as simple as storing your meds in a humid bathroom can make them less effective. These aren’t just side effects—they’re hidden risks that can derail your treatment.
And then there’s the emotional side. Many people worry that biologics are "too strong" or "experimental." But science shows they’re often safer than long-term steroid use. The real danger? Waiting too long to start them. The longer inflammation runs unchecked, the more damage it does to your joints, lungs, or gut. That’s why early treatment matters more than fear.
What you’ll find in the posts below isn’t just a list of drugs. It’s the real talk about what works, what doesn’t, and what no one tells you until it’s too late. You’ll see how TNF inhibitors affect cancer risk, why some patients switch to generics, how humidity ruins your meds, and what to do if your biologic stops working. These aren’t theoretical debates—they’re stories from people who’ve been there. And they might just help you make the next right choice.
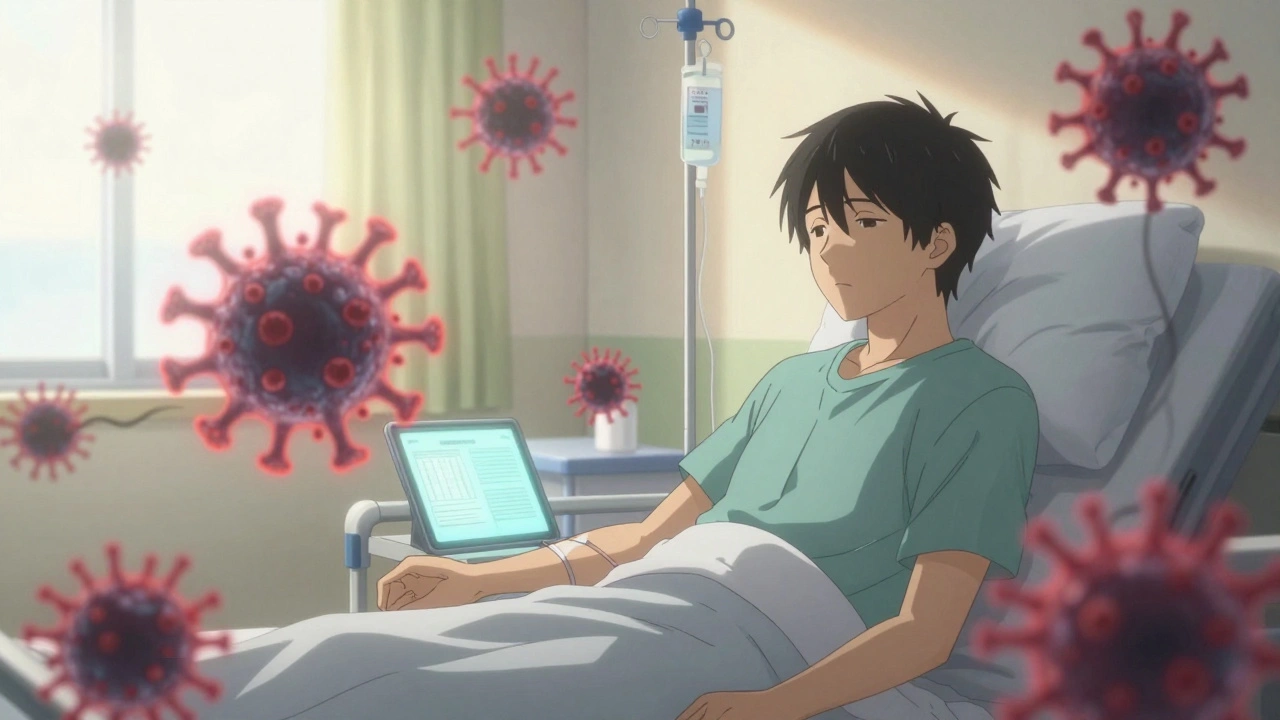
Immunocompromised Patients and Medication Reactions: What You Need to Know About Special Risks
Immunocompromised patients face higher risks of serious infections from medications meant to treat autoimmune diseases or prevent transplant rejection. Learn how different drugs affect the immune system and what steps can reduce life-threatening complications.