Ankylosing Spondylitis: Symptoms, Treatments, and Medication Insights
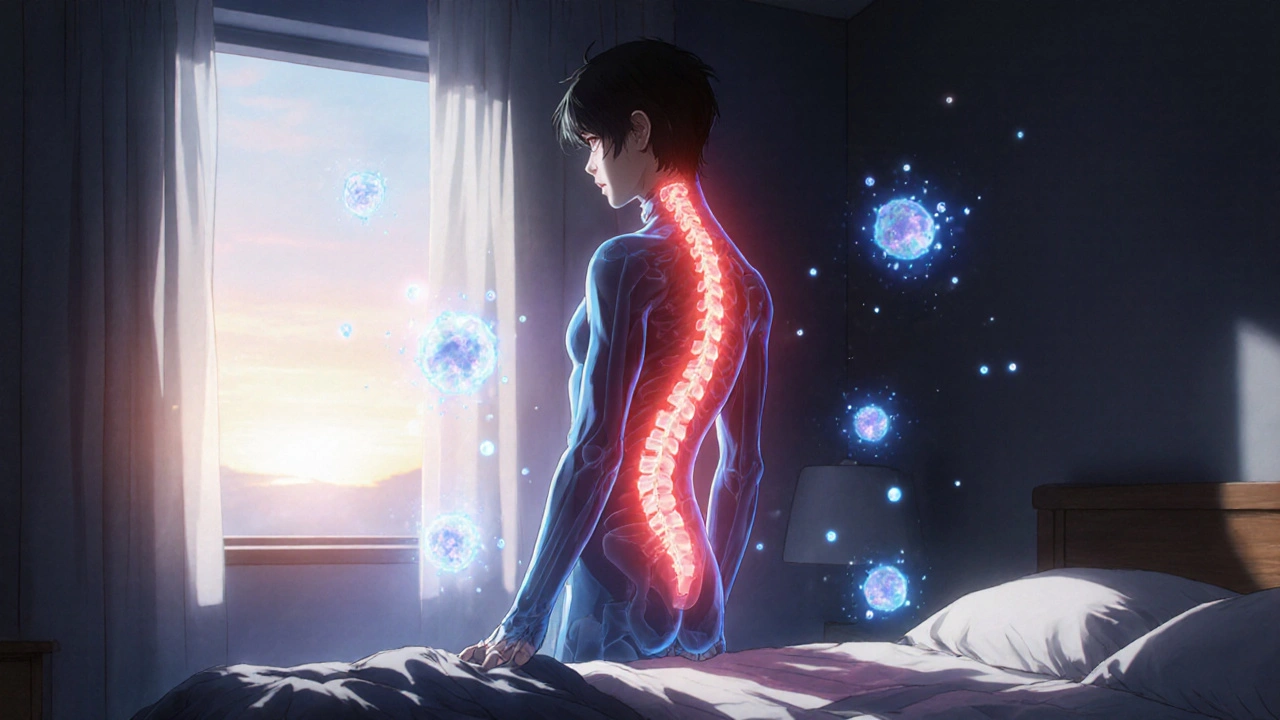
When you hear ankylosing spondylitis, a type of inflammatory arthritis that mainly targets the spine and sacroiliac joints, causing stiffness and pain that worsens over time. Also known as AS, it doesn’t just make your back hurt—it can lock your spine in place if left unchecked. Unlike regular back pain from lifting or sitting too long, ankylosing spondylitis starts young—often in your 20s or 30s—and creeps up slowly. Morning stiffness that lasts more than 30 minutes? Pain that improves with movement but gets worse with rest? Those aren’t just signs of aging. They’re red flags for AS.
What makes this condition tricky is how it connects to other parts of your body. Many people with AS also deal with eye inflammation (uveitis), gut issues like Crohn’s disease, or even heart valve problems. It’s not just a back problem—it’s a whole-system issue. And while there’s no cure, NSAIDs, nonsteroidal anti-inflammatory drugs like naproxen or indomethacin, are the first-line defense for reducing pain and inflammation—and they work for most people, at least at first. But when NSAIDs stop helping, that’s when things get serious. That’s when doctors turn to biologic drugs, targeted therapies like adalimumab or etanercept that block specific immune system proteins driving inflammation. These aren’t magic pills, but for many, they’re the only thing that stops the spine from fusing together.
Physical therapy isn’t optional with AS—it’s essential. Stretching, posture training, and swimming aren’t just nice-to-haves; they’re what keep you mobile. Without them, even the best drugs can’t prevent spinal fusion. And while some people worry about long-term side effects from biologics, the real danger is doing nothing. The longer inflammation runs wild, the more damage it does. It’s not about avoiding medication—it’s about using the right ones at the right time.
You’ll find posts here that dig into how common painkillers interact with AS meds, why some people switch from one biologic to another, and how diet and gut health might influence flare-ups. There’s also advice on managing AS alongside other conditions like high blood pressure or depression—because rarely does one illness travel alone. These aren’t theoretical guides. They’re written by people who’ve lived with AS, doctors who treat it daily, and pharmacists who know which pills work together—and which ones clash.
Whether you’re newly diagnosed, struggling with side effects, or just trying to understand why your back won’t loosen up, this collection gives you the real talk—not the brochures. No fluff. No hype. Just what works, what doesn’t, and what you need to ask your doctor next.
Ankylosing Spondylitis: How TNF Inhibitors Reduce Spine Inflammation and Improve Daily Life
Ankylosing spondylitis causes chronic spine inflammation and stiffness. TNF inhibitors like Humira and Enbrel target the root cause, reducing pain, slowing bone fusion, and improving mobility for most patients. Learn how they work and who benefits most.