Scaly Skin Condition Identifier
Answer a few questions about your skin symptoms to get an idea of possible conditions. This tool is for educational purposes only and does not replace a professional diagnosis.
When you glance in the mirror and spot a patch of skin that looks dry, flaky, or oddly raised, you’re probably dealing with what dermatologists call Scaly Overgrowths of Skin - a group of conditions where excess keratin builds up on the surface, creating visible scales or plaques. These overgrowths aren’t just cosmetic; they can signal underlying inflammation, infection, or genetic factors. Below, a dermatologist walks you through the most common types, how they’re diagnosed, and what you can do to keep them under control.
What Are Scaly Overgrowths?
At their core, scaly overgrowths are caused by the skin’s outermost cells, the Keratinocytes, producing too much keratin - the protein that gives skin its toughness. When keratin accumulates faster than it can shed, it forms the characteristic scales you see. Triggers range from immune system misfires to fungal infections, and even sun damage can play a role.
Common Types and How They Differ
Not every flaky patch is the same. Here are the five most frequently encountered scaly conditions, each with its own tell‑tale signs:
| Condition | Typical Appearance | Common Triggers | Usual Treatment |
|---|---|---|---|
| Psoriasis | Red plaques with silvery‑white scales | Genetic predisposition, stress, infections | Topical steroids, biologics, phototherapy |
| Seborrheic Dermatitis | Yellowish, greasy scales on scalp, eyebrows, chest | Malassezia yeast, hormonal changes | Antifungal shampoos, topical ketoconazole |
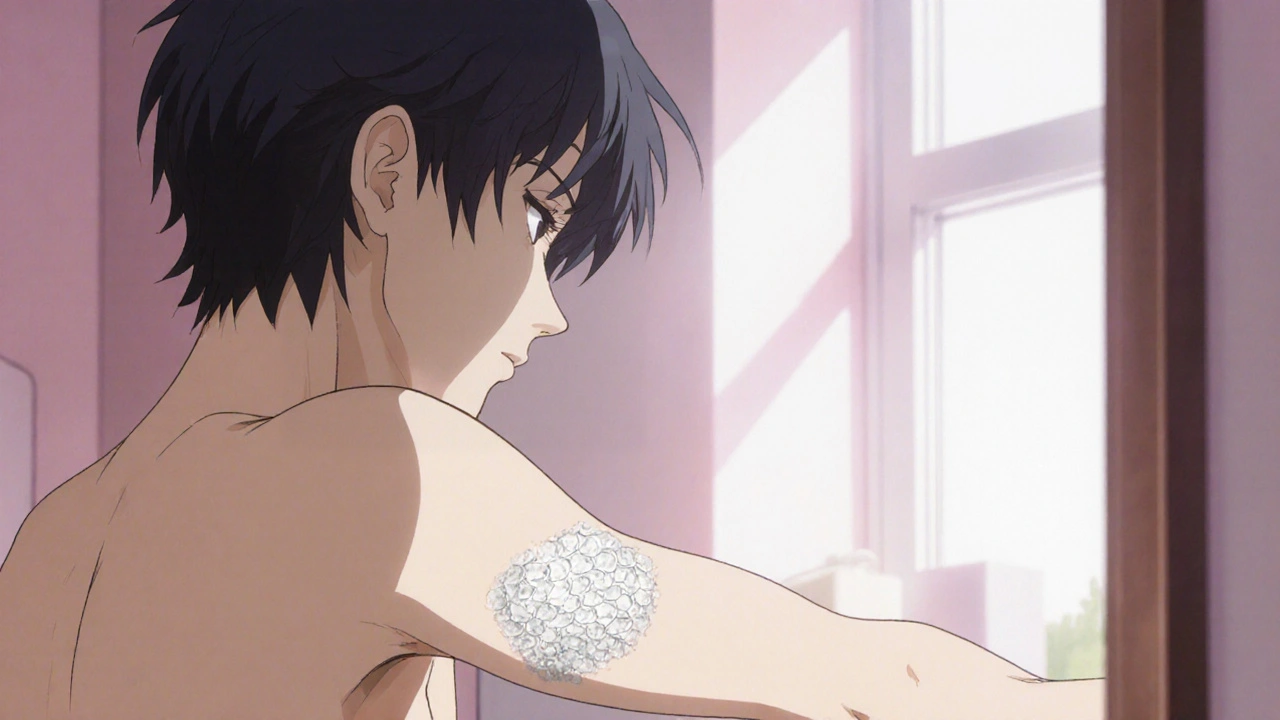
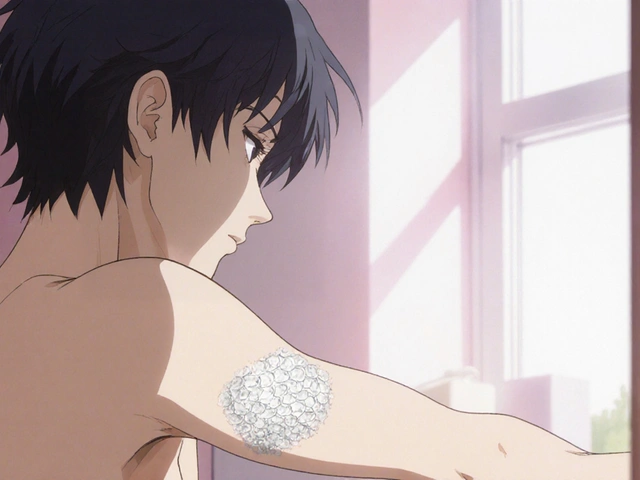
| Ichthyosis | Generalized dry, fish‑scale‑like skin | Genetic mutations (e.g., filaggrin) | Regular moisturizers, retinoids |
| Actinic Keratosis | Small, rough, crusty bumps on sun‑exposed areas | Chronic UV exposure | Cryotherapy, topical 5‑fluorouracil |
| Tinea (Ringworm) | Annular, scaly border with clearer centre | Dermatophyte fungi, warm‑humid environments | Oral or topical antifungals |
Understanding these visual cues helps you (and your doctor) narrow down the cause without a biopsy.
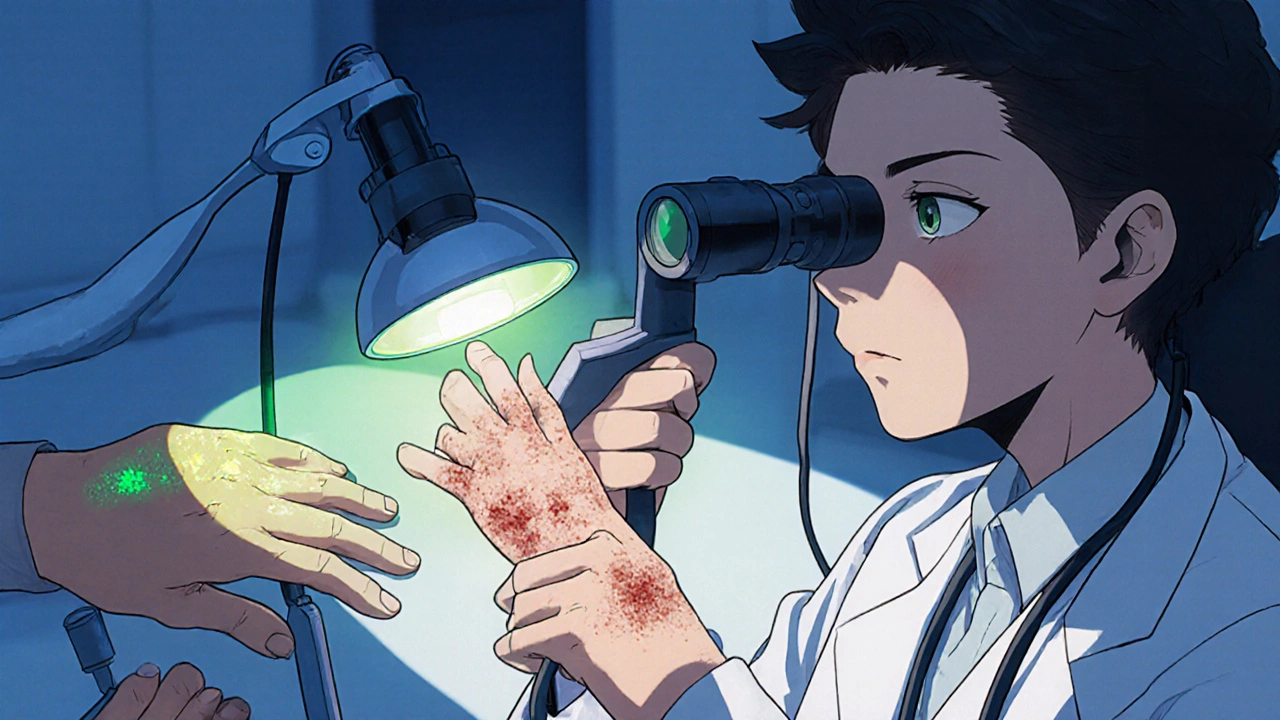
How Dermatologists Diagnose Scaly Skin
A dermatologist starts with a thorough history - age, family skin disorders, recent stressors, medication changes, and sun exposure. A visual exam follows, often with a dermatoscope to magnify patterns that are invisible to the naked eye. When the picture isn’t clear, a skin scraping or punch biopsy can confirm fungal infection or rule out pre‑cancerous lesions.
In many cases, a simple Wood’s lamp (UV light) can highlight fungal colonies, turning them a vivid yellow‑green. That quick test can differentiate Tinea from inflammatory conditions like Psoriasis.
Treatment Options Overview
Once the specific condition is identified, treatment follows three broad strategies: reduce inflammation, control keratin buildup, and address any underlying trigger.
- Topical therapies - corticosteroid creams, vitamin D analogues (for psoriasis), or antifungal ointments (for tinea). These are the first line for mild to moderate cases.
- Systemic medications - oral retinoids for severe ichthyosis, methotrexate or biologic agents for extensive psoriasis, and oral antifungals for stubborn ringworm.
- Procedural interventions - phototherapy (UVB) for psoriasis, cryotherapy for actinic keratosis, and laser resurfacing for stubborn seborrheic patches.
Choosing the right approach hinges on the area involved, patient age, and any co‑existing health issues. For example, a young adult with limited scalp seborrheic dermatitis often does well with a medicated shampoo, while an elderly patient with multiple actinic keratoses may need a series of cryotherapy sessions.
Managing Flare‑Ups and Lifestyle Tips
Even with medication, lifestyle plays a huge role in keeping scales at bay.
- Moisturize daily. Look for ointments containing ceramides or petrolatum - they lock in moisture and reduce keratin buildup.
- Control triggers. Limit alcohol, quit smoking, and manage stress through mindfulness or gentle exercise.
- Sun protection. Broad‑spectrum sunscreen (SPF 30 or higher) prevents actinic damage that can turn a simple patch into a precancerous lesion.
- Balanced diet. Omega‑3 fatty acids, found in fish and flaxseed, have anti‑inflammatory properties that may calm psoriasis flares.
- Regular check‑ups. A Dermatologist can spot early changes that you might miss, especially on hard‑to‑see areas like the scalp or back.

When to Seek Immediate Care
If you notice any of the following, call your dermatologist right away:
- Rapidly enlarging lesions that bleed or ulcerate.
- Sudden, widespread scaling accompanied by fever or joint pain.
- Persistent itching that disrupts sleep despite treatment.
- New patches on previously unaffected skin after extensive sun exposure.
These signs could indicate infection, severe inflammation, or early skin cancer - conditions that need prompt attention.
Key Takeaways
Scaly overgrowths of skin range from harmless dry patches to conditions that require medical intervention. Recognizing the pattern, seeking a professional diagnosis, and adopting a tailored treatment plan can keep your skin smooth and healthy. Remember, the best defence is a combination of good skin hygiene, trigger management, and regular dermatologist visits.



I've seen a lot of people feel overwhelmed when they first notice flaky patches, so I get how unsettling it can be. The guide does a solid job breaking down the main culprits, from psoriasis to actinic keratosis, and that helps keep the anxiety in check. Keeping a daily moisturiser routine and watching for triggers like stress or sun exposure can make a real difference. If you’re unsure which condition you have, a quick visit to a dermatologist for a dermatoscope exam is worth the peace of mind.
In accordance with current dermatological literature, the pathophysiology of keratinocyte hyperproliferation is unequivocally linked to dysregulated cytokine signaling pathways, particularly the IL‑23/Th17 axis, which necessitates a tiered therapeutic approach. Topical corticosteroids remain the first‑line intervention for inflammatory etiologies, whilst biologic agents such as secukinumab demonstrate superior efficacy in refractory psoriasis cases. Furthermore, phototherapy protocols, calibrated to specific UVB dosing regimens, have been statistically validated to reduce plaque thickness by up to 45 % (p < 0.01). It is imperative to recognize that patient adherence, often compromised by adverse‑effect concerns, can be mitigated through comprehensive education and follow‑up scheduling 😊. Ultimately, a multidisciplinary strategy, integrating dermatology, nutrition, and psychosocial support, optimizes clinical outcomes 😌.
Honestly, most of these “guidelines” sound like textbook fluff that rarely translates to real‑world skin care.
Thank you for compiling such a thorough overview; it respects the diverse experiences people have with skin conditions across different backgrounds. I especially appreciate the emphasis on lifestyle adjustments, like diet and stress management, which resonate universally. Remembering to hydrate the skin and protect it from sun exposure is a practice echoed in many cultures, and it’s great to see it highlighted here. Your balanced tone makes the information accessible without feeling clinical.
Reading this makes me want to take better care of my skin and help others do the same The steps are clear and doable and the reminder to see a doctor early is key Keep up the good work
Look, everyone, this is exactly why we need to pay attention to the details, because ignoring the basics-like daily moisturisation-leads to bigger problems, and we can’t afford to be complacent, especially when sun damage is lurking, so I urge you all, yes, all of you, to adopt rigorous sunscreen habits, and don’t neglect follow‑up appointments, your skin’s future depends on it!