When your doctor switches your prescription from brand-name to generic, do you feel relieved-because it’s cheaper-or uneasy-because you’re not sure it’ll work the same? You’re not alone. Millions of patients across the U.S. have the same gut feeling: generic drugs might save money, but do they save lives too?
Why Do People Doubt Generic Drugs?
The science is clear: the FDA requires generic drugs to be bioequivalent to their brand-name counterparts. That means they deliver the same active ingredient, in the same strength, and work the same way in your body-within a narrow 80% to 125% range of absorption. But patients don’t always trust the numbers. They trust their experiences. A 2012 CDC survey found that 20% to 40% of patients weren’t sure if generics were as safe or effective as brand-name drugs. One in five outright believed generics were less safe. Why? Because the word "generic" itself triggers a psychological bias. It sounds like "basic," "cheaper," or "inferior." That’s not just about packaging-it’s about how our brains link cost to quality. Studies show people assume expensive things work better, even when they don’t. And when a pill looks different-color, shape, size-it feels like a different medicine, even if the active ingredient is identical.Who’s Most Likely to Worry?
Not everyone feels the same way about generics. Risk perception isn’t random-it’s shaped by who you are. Older adults, especially those over 60, are more likely to fear side effects. A 2024 study found 31.9% of seniors worried about adverse reactions, compared to just 24.7% of younger patients. People with lower education levels were nearly twice as likely to believe generics were dangerous. Those who are unemployed or retired tended to be more accepting-maybe because they’ve felt the pinch of high drug prices. Meanwhile, Black and Hispanic patients were 1.8 times more likely than White patients to express safety concerns, according to a 2009 NIH study. Rural patients often believe generics are weaker and need higher doses. Urban patients worry more about where the drugs are made. And patients with low health literacy-those who struggle to understand medical information-are twice as likely to think generics are less effective. These aren’t just opinions. They’re deeply held beliefs shaped by personal stories, cultural cues, and lack of clear communication.The Anecdote That Beats the Data
Science says generics are equivalent. But patients remember the time their blood pressure spiked after switching to a generic. Or when their depression symptoms returned after changing from brand-name sertraline to a generic version. On Reddit, users share stories like: "I switched to generic bupropion and felt like I was going through withdrawal. Went back to the brand-symptoms vanished." These aren’t rare. PatientsLikeMe, a community forum, has over 1,200 reports of people saying generics caused different side effects or seemed less effective. The FDA even issued a safety notice in 2012 about certain generic versions of bupropion XL, which fueled these fears-even though later studies showed most cases were due to individual variation, not product failure. Here’s the problem: one bad experience sticks. A 2021 survey found 68% of patients who switched to generics saw no difference. But the 32% who did? Their stories echo louder than the majority. When someone says, "My doctor said they’re the same, but how do I know which batch they gave me?"-they’re not questioning science. They’re questioning control.
Doctors and Pharmacists Hold the Key
Who you hear it from matters more than what you hear. A 2011 study in JAMA Internal Medicine found patients were 3.2 times more likely to accept a generic if their doctor explained bioequivalence clearly. That’s not just handing them a pamphlet. It’s saying: "This generic has the same active ingredient, works the same way, and is held to the same standards. I’ve prescribed it to dozens of patients with the same results." Pharmacists play a critical role too. When they take even a few extra minutes to explain why the pill looks different, adherence improves by 37%. But here’s the catch: the average pharmacist-patient conversation about a generic substitution lasts just 47 seconds. That’s not enough to undo years of misinformation. Specialists are less likely to prescribe generics than primary care doctors. And patients in poorer neighborhoods use generics at lower rates-even when insurance covers them. Why? Because trust isn’t built by price tags. It’s built by relationships, clarity, and consistency.What Actually Works to Change Minds?
You can’t just tell people they’re wrong. You have to meet them where they are. A 2017 study in the Journal of General Internal Medicine showed that tailored education for low-literacy patients reduced safety concerns by 42%. Simple visuals, plain language, and stories from other patients worked better than technical brochures. The FDA’s own materials scored only 3.2 out of 5 on clarity. But AARP’s guide? It scored 4.5. Why? Because it spoke like a neighbor, not a regulator. Timing matters too. Patients who get a clear explanation at the moment of prescribing are 2.8 times more likely to accept the generic. Waiting until they pick up the prescription is too late. The doubt has already taken root. Some insurers are trying new approaches. Medicare plans that offer $0 copays for generics saw 18% higher usage than those with tiered pricing. When cost isn’t a barrier, people are more open to trying-but not always. The biggest barrier isn’t money. It’s fear.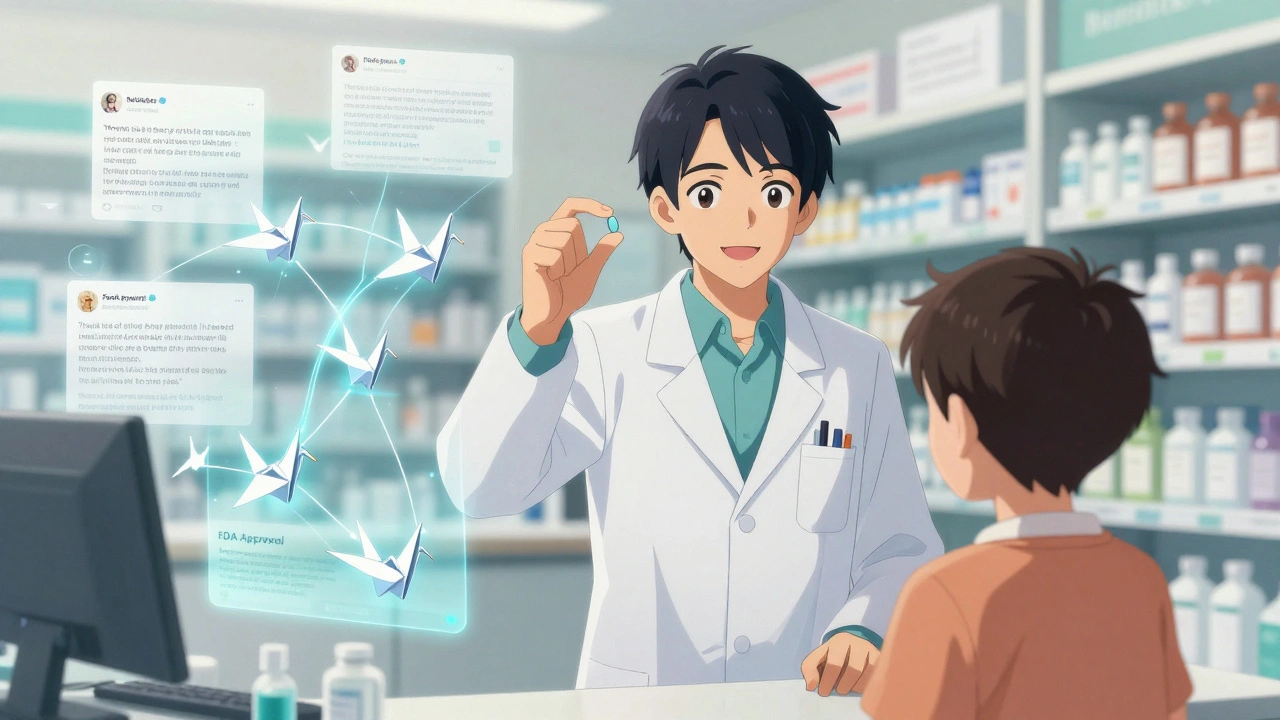
The Hidden Cost of Doubt
Generics make up 90% of prescriptions in the U.S., but they account for only 23% of drug spending. That’s $370 billion saved every year. Yet, because of safety fears, patients still request brand-name drugs-costing the system an estimated $8 billion annually in unnecessary prescriptions. Brand-name companies have even started selling "authorized generics"-their own drugs, sold under a generic label. It’s a smart business move. But it backfires psychologically: if the brand is good enough to sell as a generic, why didn’t they just make it generic in the first place? This confusion deepens mistrust. Newer complex generics-like inhalers, eye drops, or topical creams-are harder to prove equivalent. And patients know it. A 2023 survey found 48% of people specifically worry about these types of generics. The science is catching up, but perception is lagging.What’s Next?
The FDA is launching multilingual campaigns to tackle misconceptions. Machine learning tools can now predict with 87% accuracy which patients are most likely to reject generics-so clinics can target them with personalized education. But technology alone won’t fix this. The real solution is human. It’s a doctor taking 90 seconds to say: "I know you’re worried. Let me explain why this is safe." It’s a pharmacist asking: "Have you taken this before? How did it feel?" It’s clear, consistent, and compassionate communication. Until we address the emotional truth behind the numbers-until we rebuild trust, one conversation at a time-we’ll keep seeing patients pay more, feel less safe, and get worse outcomes. The science is settled. The question now is: can we make the message stick?Are generic drugs really as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards as brand-name drugs for quality, strength, purity, and stability. They must deliver the same active ingredient in the same way and produce the same clinical effect. Over 90% of prescriptions in the U.S. are generics, and they’ve been used safely by millions for decades.
Why do some people feel generics don’t work as well?
Sometimes, people notice differences in side effects or effectiveness after switching. This can happen due to variations in inactive ingredients (like fillers or dyes), which affect how the drug is absorbed or how the pill looks and tastes. In rare cases, certain generic versions of drugs like bupropion XL had issues in the past, which were later addressed. But most often, it’s a psychological effect-patients expect a change, so they perceive one. Studies show 68% of patients report no difference at all.
Do cheaper generics mean lower quality manufacturing?
No. Generic drugs are made in the same type of facilities as brand-name drugs, and they’re inspected by the FDA using the same standards. Many generics are made by the same companies that produce brand-name versions. The FDA has invested over $150 million since 2012 to improve oversight of generic manufacturing, both in the U.S. and abroad.
Can I ask my doctor to keep me on the brand-name drug?
Yes. You always have the right to ask for a brand-name prescription. But your doctor may need to write "Do Not Substitute" on the prescription, and your insurance may charge you more. If you’re concerned about switching, talk to your provider. They can help you understand whether a generic is appropriate for your condition and address any worries you have.
Why do generics look different from brand-name pills?
By law, generic drugs can’t look exactly like the brand-name version, even if they contain the same active ingredient. That’s to avoid trademark infringement. Differences in color, shape, or size are normal and don’t affect how the drug works. If you’re confused by a new pill, ask your pharmacist-it’s not a sign of lower quality, just a legal requirement.
Should I be worried about complex generics like inhalers or creams?
Complex generics-like inhalers, nasal sprays, or topical creams-are harder to prove equivalent because their delivery method matters as much as the drug itself. The FDA has stricter requirements for these, but public concern is higher. If you’re prescribed one, ask your doctor or pharmacist about the specific product and whether it’s been tested for equivalence. Most are safe and effective, but it’s okay to ask questions.


Been prescribing generics for years. My patients who stick with them report zero issues. The pill looks different? So what. It’s the same active ingredient. The real problem isn’t the drug-it’s the lack of a 90-second chat from the doc or pharmacist. Just say: 'This works the same. I’ve seen it work for 50 people like you.' That’s all it takes. 🙌
I switched to a generic blood pressure med last year and felt like I was being slowly poisoned. My hands shook. My head throbbed. I went back to the brand and suddenly I was human again. Science doesn’t feel your pulse. Only your body does.
OMG I’m so glad someone finally said this. My mom took generic sertraline and cried for three days straight. She said she felt ‘empty’ like her soul got swapped out. The pharmacist just shrugged and said ‘it’s the same.’ Like that fixes grief.
The entire discourse is predicated on a foundational epistemological fallacy: that bioequivalence is ontologically sufficient to guarantee therapeutic equivalence. The phenomenological experience of the patient-the hermeneutic reading of one’s own somatic text-is rendered illegible by the positivist hegemony of the FDA’s statistical thresholds. We are not data points. We are embodied subjects navigating a pharmacological labyrinth of semiotic dissonance.
The notion that psychological bias invalidates empirical evidence is a classic case of conflating perception with reality. The FDA’s bioequivalence standard is not arbitrary-it is statistically validated, peer-reviewed, and legally binding. To dismiss it on the basis of anecdotal discomfort is to elevate subjectivity above scientific consensus. This is not skepticism. It is anti-intellectualism dressed in the language of patient autonomy.
My cousin took generic metformin and got sick every time. Switched back to brand-zero issues. The pharmacy said it was the same. But my cousin didn’t feel the same. Who’s wrong here? The FDA? Or the system that treats people like machines? We need to stop pretending science has all the answers when people are suffering.
Bro the FDA is just a corporate puppet. They approve generics made in India that look like candy. My uncle took one and his liver went on vacation. Now he’s on dialysis. And you wanna tell me it’s ‘the same’? 😒
Let me tell you something. In rural India, people take generics because they have no choice. But they don’t trust them. Why? Because they’ve seen too many fake pills. So when they get a generic here, they think: ‘Is this the real one?’ It’s not about science. It’s about survival. We need to fix trust first. Not just information.
One must question the very ontology of the pharmaceutical industry. If the same molecule is manufactured by the same corporation under two labels-one premium, one ‘generic’-is not the latter a performative act of class stratification disguised as cost-efficiency? The brand-name is a placebo for the bourgeoisie. The generic is the proletariat’s burden wrapped in the illusion of equity.
I get it. I used to be scared of generics too. Then I started reading the FDA’s inspection reports. Same factories. Same inspectors. Sometimes the same people making both. The only difference? The price tag. And the pill color. I don’t care if it’s blue or white. I care if it keeps me alive. It does. 🤝
Actually the bupropion XL issue was a known problem and the FDA recalled the bad batches. So if you’re still scared of generics because of that, you’re using a 12-year-old fear to ignore 99% of safe, tested meds. You’re not being cautious. You’re being stubborn. And it’s costing you money. And possibly your health.
It is not merely a matter of patient perception-it is a systemic failure of medical education and institutional communication. The failure to articulate bioequivalence with clarity, consistency, and empathy is not a patient problem. It is a professional failure. To blame the patient for distrusting a system that refuses to explain itself is not only unscientific-it is ethically indefensible.
My grandma takes generic lisinopril. She’s 82. Still walks 3 miles a day. No side effects. She doesn’t know what ‘bioequivalent’ means. But she knows her body. And hers says: ‘This works.’ 💪❤️