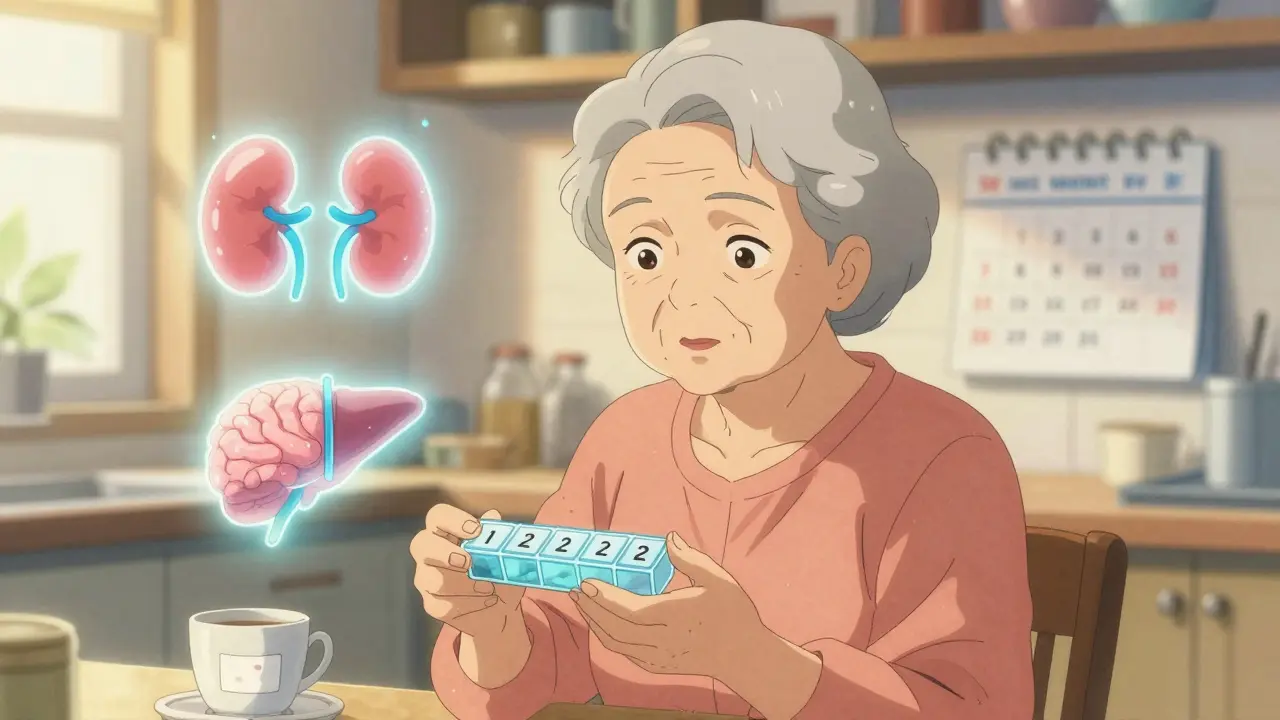
By the time you hit 70, your body doesn’t process medicine the same way it did at 40. That’s not just a myth-it’s biology. Your kidneys slow down. Your liver works less efficiently. Fat replaces muscle. And your brain becomes more sensitive to certain chemicals. These changes don’t happen overnight, but they add up. And when they do, the pills you’ve been taking for years can suddenly become dangerous.
Why Your Body Processes Drugs Differently as You Age
Think of your body like an old car. It still runs, but it needs different fuel, more frequent tune-ups, and a lighter load. The same goes for medication. As you age, four key systems change: your kidneys, liver, body composition, and brain.
Your kidneys filter about half as much blood by age 80 compared to when you were 30. That means drugs like digoxin, warfarin, and many antibiotics stay in your system longer. A standard dose that was safe at 50 can build up to toxic levels by 75. That’s why doctors now check your creatinine clearance-not just your serum creatinine-before prescribing. If your kidney function drops below 60 mL/min, about 40% of common medications need a lower dose.
Your liver, which breaks down drugs like propranolol and lidocaine, loses about 30-40% of its blood flow after 70. That slows down metabolism. Drugs that used to wear off in 8 hours might now last 16. That’s why some people feel dizzy or drowsy long after taking a pill they’ve used for decades.
Body fat increases as you age-especially in women. That means fat-soluble drugs like diazepam (Valium) or amitriptyline get stored in fatty tissue and released slowly. This can cause prolonged effects, even with normal doses. Meanwhile, muscle mass drops, which affects how water-soluble drugs like lithium are distributed. The result? You need less of the same drug to get the same effect.
More Sensitive Brain, More Side Effects
It’s not just about how your body handles drugs-it’s about how your brain reacts to them. Older adults are 2 to 3 times more sensitive to central nervous system depressants. Benzodiazepines like lorazepam or sleep aids like zolpidem can cause confusion, falls, and memory problems even at low doses. One study found that 25% of adults over 75 developed confusion on a standard 25mg dose of hydroxyzine-something that rarely happened under 60.
Even drugs you might think are harmless can be risky. Diphenhydramine, found in many over-the-counter sleep aids and allergy pills, has strong anticholinergic effects. In older adults, it can cause urinary retention, constipation, blurred vision, and cognitive decline. The Anticholinergic Cognitive Burden Scale is now used by geriatricians to measure this risk. A score above 3 increases dementia risk by 50% over seven years.
Heart medications also behave differently. Beta-blockers like metoprolol don’t work as well because your heart’s beta-receptors lose about half their responsiveness after 70. But your blood vessels still react to alpha-receptors, so blood pressure meds can still drop your pressure too much-leading to dizziness or falls. That’s why some seniors need different drugs altogether, not just lower doses.
Why Standard Doses Don’t Work for Seniors
Most drug dosing was tested on healthy adults under 65. That’s a problem. Only 12% of participants in phase 3 clinical trials are over 75. So when you see a pill labeled “5 mg daily,” that number was likely determined by a 45-year-old man in a trial-not a 78-year-old woman with kidney disease and arthritis.
Take warfarin, for example. The standard dose is 7-10 mg. But for older adults, especially those over 80, 5-6 mg is often enough. Why? Their liver makes fewer clotting factors, and their albumin levels drop. That means more of the drug floats around freely in the blood, increasing bleeding risk. A 2023 study showed that using age-adjusted dosing cut major bleeding events by 31% in patients over 80.
Insulin is another example. Older adults are more sensitive to its effects. A dose that worked fine at 60 can cause dangerous lows at 80. Emergency room visits for insulin-related hypoglycemia in seniors have risen sharply. Many endocrinologists now start insulin at 2-4 units instead of 10, then adjust slowly.
Even common painkillers like acetaminophen behave differently. Slower stomach emptying delays absorption by 1-2 hours. That might make you think the pill isn’t working, so you take another. But when it finally kicks in, you end up with too much. That’s why experts recommend sticking to 3,000 mg max per day for seniors-even though the label says 4,000.
What Doctors Should Be Doing (But Often Aren’t)
There are tools to help. The Beers Criteria, updated in 2023, lists 30 medications that should be avoided or used with extreme caution in seniors. These include anticholinergics, certain NSAIDs, and long-acting benzodiazepines. Yet, many doctors still prescribe them because they’re familiar or because they don’t have time to review every pill.
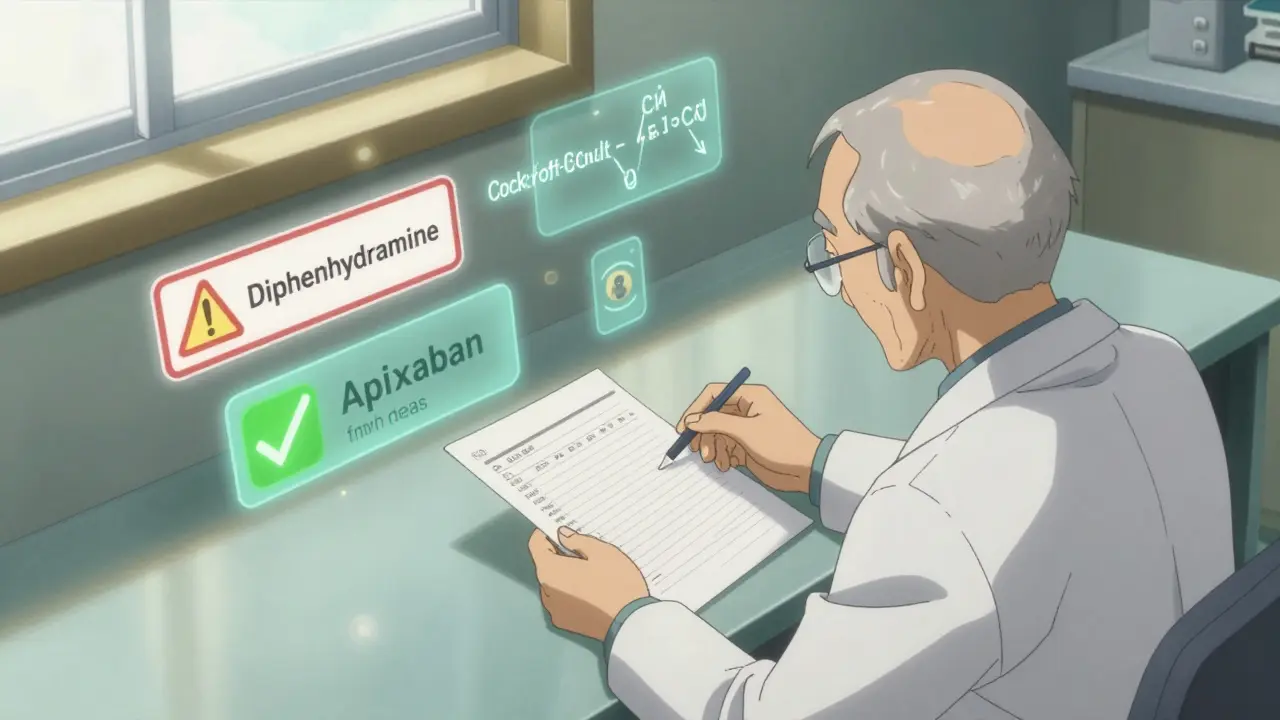
Pharmacists are stepping in. In Australia, the UK, and the U.S., pharmacist-led medication reviews have reduced inappropriate prescribing by 35%. The START/STOPP criteria help identify both missing needed drugs and harmful ones. For example, a senior with atrial fibrillation might need apixaban-but if their kidney function is low, the dose must be adjusted. One Reddit user shared that their father’s AFib only stabilized after his apixaban was increased from 2.5mg to 5mg once his creatinine clearance improved.
Another key tool is the Cockcroft-Gault equation, which estimates kidney function using age, weight, and sex-not just a single blood test. Many clinics still rely on serum creatinine alone, which can be misleading in seniors with low muscle mass. A normal creatinine level doesn’t mean normal kidney function.
The ‘Start Low, Go Slow’ Rule
The most important rule in geriatric prescribing is simple: start low, go slow. That means beginning with 25-50% of the standard adult dose, especially for drugs cleared by the kidneys or affecting the brain. Then, wait weeks before adjusting. This isn’t just caution-it’s science.
A 2022 survey of 1,200 pharmacists found that 82% saw better outcomes when they followed this approach. One woman in Sydney, 81, was on 10mg of sertraline for anxiety. She started feeling foggy and unsteady. Her GP reduced it to 2.5mg. Within two weeks, her balance improved and her mood stayed stable. She didn’t need a higher dose-just the right one.
For new medications, doctors should ask: Is this absolutely necessary? Is there a safer alternative? Can we start with half the dose? Too often, the answer is no, no, and no.
What You Can Do Right Now
You don’t need to be a doctor to protect yourself or a loved one. Here’s what works:
- Keep a full list of every pill, supplement, and OTC drug you take-including what it’s for and when you take it. Bring it to every appointment.
- Ask your doctor or pharmacist: “Is this still necessary?” and “Could this be causing my dizziness or confusion?”
- Request a medication review at least once a year-especially if you’re on five or more drugs.
- Use the Beers Criteria app (downloaded over 250,000 times) to check if any of your meds are flagged for seniors.
- Never stop a drug suddenly-especially antidepressants, blood pressure meds, or anti-seizure drugs. Talk to your doctor first.
- Watch for new symptoms after starting a new drug. Confusion, falls, nausea, or fatigue aren’t just “getting older”-they might be side effects.
The Future of Senior Medications
Science is catching up. The FDA now requires new drugs to include data from adults over 65. In 2023, they approved the first age-adjusted dosing algorithm for dabigatran (Pradaxa), which cut bleeding in seniors by a third.
Researchers are also exploring senolytics-drugs that clear out aged, damaged cells. Early studies show they may restore how organs respond to medication. One combination (dasatinib + quercetin) reduced a key aging marker (p16^INK4a) by 50% in human fat tissue. That could mean drugs work more predictably in older bodies in the future.
But until then, the best medicine is awareness. Aging isn’t a disease. But treating it like it is-by giving older adults the same doses as younger people-is dangerous.
Medication isn’t one-size-fits-all. Especially not after 65. The right dose isn’t what’s on the bottle. It’s what your body can handle now.
Why do seniors need lower doses of medication?
As you age, your kidneys and liver process drugs more slowly, your body fat increases, and your brain becomes more sensitive to certain chemicals. This means drugs stay in your system longer and have stronger effects-even at the same dose. A standard adult dose can become toxic in someone over 75, so lower doses are often safer and just as effective.
What medications should seniors avoid?
The American Geriatrics Society’s Beers Criteria lists 30 medications to avoid or use with caution in seniors. These include benzodiazepines (like diazepam), anticholinergics (like diphenhydramine), certain NSAIDs (like indomethacin), and long-acting sleep aids. These drugs increase risks of falls, confusion, kidney damage, and dementia. Always ask if there’s a safer alternative.
Can over-the-counter drugs be dangerous for older adults?
Yes. Many OTC drugs, like sleep aids, allergy pills, and stomach remedies, contain anticholinergics or NSAIDs that are risky for seniors. Diphenhydramine (Benadryl) and doxylamine (Unisom) can cause confusion and urinary retention. Pain relievers like ibuprofen can damage kidneys or cause bleeding. Always check the active ingredients and talk to a pharmacist before taking anything new.
How do I know if a medication is causing side effects?
New symptoms within days or weeks of starting a drug are often side effects. Look for confusion, dizziness, falls, nausea, loss of appetite, fatigue, or changes in urination or bowel habits. These aren’t normal aging-they’re red flags. Keep a symptom diary and bring it to your doctor. Sometimes, lowering the dose or switching drugs fixes the problem.
What’s the best way to manage multiple medications?
Ask for a medication review with your doctor or pharmacist at least once a year. Use a pill organizer, keep a written list of all drugs (including supplements), and never take anything new without checking if it interacts with your current meds. Tools like the Beers Criteria app and the Anticholinergic Burden Calculator can help identify risks. Many pharmacies now offer free medication reviews for seniors.




The Beers Criteria is non-negotiable in geriatric pharmacotherapy. If you're still prescribing diphenhydramine for sleep in a patient over 70, you're not just outdated-you're endangering lives. Anticholinergic burden isn't a suggestion, it's a Class I risk factor for dementia. And don't get me started on NSAIDs in the elderly-COX-2 inhibition without renal perfusion is a one-way ticket to acute kidney injury. The Cockcroft-Gault equation should be mandatory, not optional. Serum creatinine alone is meaningless when muscle mass is 30% below baseline. This isn't opinion-it's clinical gospel.
I’ve seen this firsthand with my dad. He was on 10mg of sertraline for years and started stumbling around like he was drunk. The doctor just said ‘you’re getting older’ but we pushed back and got it cut to 2.5mg. He’s been fine since. I wish more doctors listened instead of just checking boxes. It’s not about being weak-it’s about being smart with medicine. We need to stop treating seniors like failed versions of young adults and start treating them like their own category.
It’s funny how we think of medicine as this exact science but then give the same pills to a 25-year-old athlete and a 78-year-old with arthritis and call it fair. Our bodies aren’t machines with interchangeable parts. They’re ecosystems that change with time. A drug that was a gentle breeze at 40 becomes a hurricane at 80. And we still act surprised when people fall or get confused. Maybe we need to stop thinking about dosage and start thinking about harmony-what does the body need now, not what it needed 40 years ago?
My grandma took Benadryl for years because she thought it was ‘just an allergy pill’. Then she started forgetting her own name for a few hours after taking it. We switched her to a non-anticholinergic antihistamine and she’s like a different person. I’m so glad this article mentioned the Anticholinergic Burden Scale. I printed it out and showed it to her doctor. She didn’t know it existed. Why aren’t these tools taught in med school? Why are we still guessing?
My uncle died because his doctor kept giving him 10mg of warfarin like he was 50. He bled out internally and they said it was ‘unpredictable’. Unpredictable? No. It was criminal negligence. His creatinine clearance was 42. He was on 6 meds including ibuprofen daily. The hospital didn’t even check his meds until he was in the ICU. If this doesn’t make you furious, you’re not paying attention. This isn’t aging-it’s medical malpractice disguised as routine care.
The data is clear. The science is settled. Yet, the gap between evidence and practice remains vast. Why? Time constraints, institutional inertia, and a systemic undervaluing of geriatric care. We have tools-START/STOPP, Beers Criteria, pharmacogenomic screening-but they remain underutilized. The real tragedy isn’t the lack of knowledge-it’s the lack of will. We know what to do. We just don’t prioritize it. And that’s not just inefficient-it’s unethical.
You think this is bad? Wait till you see what happens when a 75-year-old is on 12 meds and their daughter brings them to a Walmart clinic and says ‘just fix the pain’. No one checks interactions. No one knows what’s in the cabinet. I had a patient on amitriptyline, lisinopril, ibuprofen, melatonin, and OTC cold meds-all prescribed by different doctors. She was in a wheelchair from dizziness. Her daughter blamed ‘old age’. I told her: no. This is polypharmacy murder. And the system lets it happen every single day. Someone needs to hold these doctors accountable.
Just started my dad on 2mg of apixaban instead of 5mg after his creatinine clearance dropped. He’s been fine. No bleeding. No confusion. Simple fix. Why do we make it so complicated? Start low go slow. It’s not rocket science. Just common sense. And stop giving seniors the same doses as 30-year-olds. We’re not helping. We’re hurting.