Polypharmacy Risk Calculator
Medication Risk Assessment
This tool shows how your risk of dangerous drug interactions increases with each additional heart medication. Based on studies showing that taking multiple heart medications can significantly increase your risk of harmful interactions.
Your risk of dangerous drug interactions:
0%
Select the number of medications to see your risk
Important Safety Note
This calculator shows statistical risk based on number of medications. Your actual risk may be higher or lower based on specific drug combinations, your health conditions, liver/kidney function, and other factors. Always consult with your doctor or pharmacist about your specific medications.
Key Risk Statistics
Risk with 2 medications
Risk with 4 medications
Risk with 7+ medications
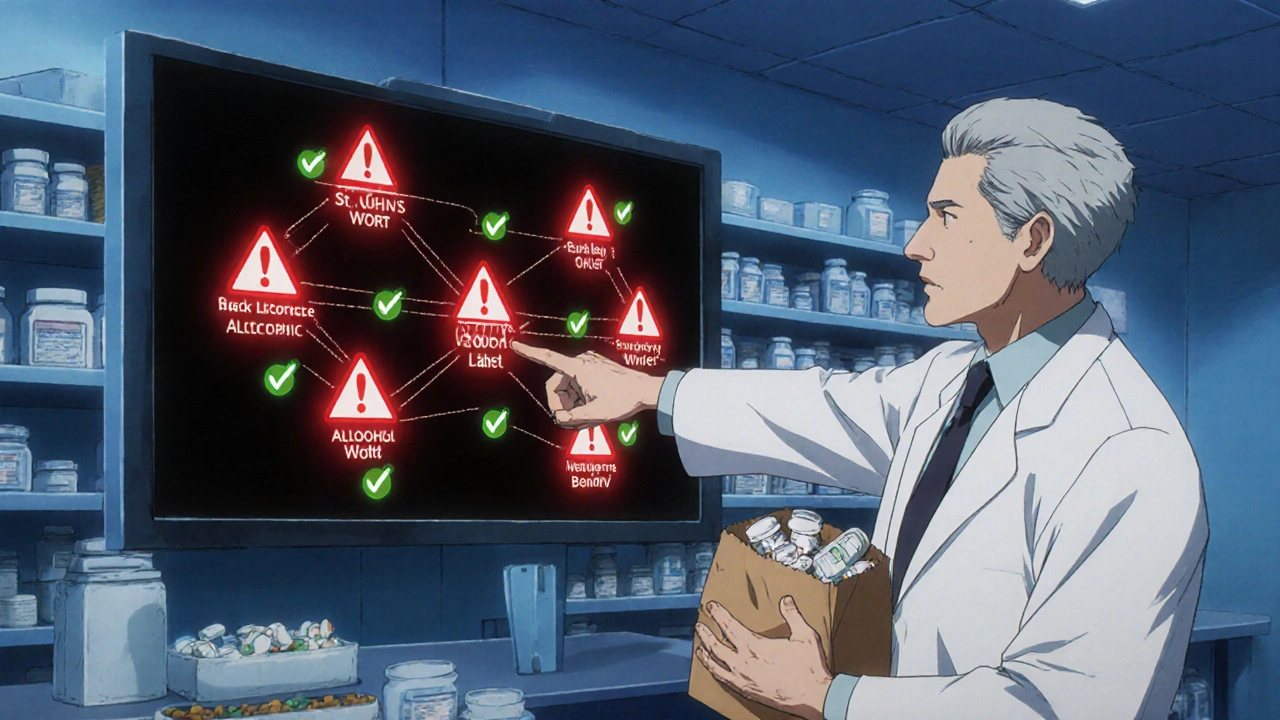
Most Dangerous Combinations
- Statins + Grapefruit Juice Emergency
- NSAIDs + Blood Pressure Meds Emergency
- Anticoagulants + NSAIDs/Aspirin Emergency
- Beta Blockers + Black Licorice High Risk
- St. John's Wort + Heart Meds High Risk
- Alcohol + All Heart Medications High Risk
When you’re managing heart disease, taking multiple medications is often unavoidable. Blood pressure pills, cholesterol-lowering drugs, blood thinners, diuretics, and heart rhythm controllers all play a role. But here’s the hard truth: combining multiple heart medications isn’t just common-it’s dangerous if you don’t know what you’re mixing.
Every extra pill you take increases your risk. One study found that people taking just two heart medications had a 13% chance of a harmful drug interaction. That number jumps to 38% with four medications. And if you’re on seven or more? Your risk hits 82%. These aren’t hypothetical numbers. These are real risks happening in hospitals and living rooms across Australia and beyond.
Why Heart Medications Are Especially Risky
Heart drugs don’t play nice with much of anything. They’re designed to work precisely-too little and your condition worsens; too much and you risk organ damage, irregular heartbeat, or even sudden death. Many of these drugs are processed by the same liver enzymes, especially CYP3A4. When two drugs compete for the same enzyme, one can get stuck in your system longer than it should.
Take statins, for example. These are among the most commonly prescribed heart medications. But if you drink grapefruit juice-even just one quart a day-you’re blocking the enzyme that breaks down statins. That means your blood levels of the drug can spike by nearly 50%. The result? Muscle breakdown (rhabdomyolysis), kidney failure, and in rare cases, death. The FDA warns this isn’t just a myth. It’s a documented, preventable danger.
Unsafe Combinations You Must Avoid
Some combinations are so dangerous they’re considered medical emergencies. Here are the top ones you need to know:
- Statin + Grapefruit Juice - As mentioned, this combo can cause toxic statin levels. Even a single glass daily can be enough to trigger problems.
- NSAIDs (like ibuprofen) + Blood Pressure Medications - Over-the-counter painkillers can cancel out the effects of ACE inhibitors, beta blockers, and diuretics. Worse, they raise your risk of kidney damage and fluid retention.
- Anticoagulants (warfarin, apixaban) + NSAIDs or Aspirin - Mixing these increases bleeding risk dramatically. A simple fall could turn deadly.
- Beta Blockers or Calcium Channel Blockers + Black Licorice - Natural black licorice contains glycyrrhizin, which raises blood pressure and lowers potassium. This can undo weeks of careful medication management.
- St. John’s Wort + Any Heart Medication - This popular herbal supplement speeds up how fast your body clears out drugs like beta blockers, statins, and antiarrhythmics. Your pills stop working. Your condition worsens.
- Alcohol + All Heart Medications - Alcohol doesn’t just interact-it multiplies risk. It can lower blood pressure too much, worsen heart rhythm problems, and increase liver damage when combined with statins or anticoagulants.
And don’t forget the hidden players: antihistamines like diphenhydramine (Benadryl), decongestants like pseudoephedrine (Sudafed), and even some antacids. These over-the-counter items can interfere with absorption, raise blood pressure, or trigger dangerous heart rhythms like QT prolongation.
What’s Safe? The Rules of Thumb
There’s no blanket answer. But there are clear rules that reduce risk:
- Use one pharmacy for everything. Pharmacists can track every pill you take and flag interactions your doctor might miss. Don’t switch between pharmacies for convenience.
- Do a brown bag review every six months. Take every medication-prescription, over-the-counter, vitamins, supplements-to your doctor or pharmacist. Don’t rely on memory. People forget. Supplements get added. Doses change.
- Never start a new supplement without asking. Turmeric, garlic, fish oil, ginseng-they all interact. Just because it’s “natural” doesn’t mean it’s safe with your heart meds.
- Know your meds by their generic names. Brand names change. Generic names don’t. If you know your statin is atorvastatin, not just “the cholesterol pill,” you can better track interactions.
- Watch for sudden changes. If you feel dizzy, weak, swollen, or your heart starts racing after starting a new drug-even if it’s just a cold medicine-call your doctor. Don’t wait.
Polypharmacy and Older Adults: A Silent Crisis
Over 90% of adults over 65 with heart disease take five or more medications. That’s not just common-it’s the norm. But the older you are, the more your body changes. Your liver slows down. Your kidneys filter less. Your gut absorbs differently. What was safe at 55 can become dangerous at 75.
Studies show that people over 65 make up 40% of those at highest risk for dangerous drug interactions. And it’s not just about the pills. Polypharmacy increases fall risk, confusion, and hospitalizations. A 2023 University of Rochester study linked taking seven or more medications to a 30% higher chance of functional decline.
Some doctors are now talking about “deprescribing”-safely removing drugs that may no longer be necessary. But patients often resist. They fear stopping a pill will mean their condition is worsening. Or worse, that their doctor has given up on them. That fear is real. But the alternative-taking pills that interact, cause side effects, or do nothing-is worse.
Technology Isn’t Enough
You might think your doctor’s electronic system catches all these risks. It doesn’t. Clinical decision tools flag about 77% of major interactions. But they miss 23%. Why? Because they don’t know your exact diet, your alcohol intake, your genetic makeup, or whether you took your pill with grapefruit juice this morning.
Some people have genetic variants that make them slow or fast metabolizers of certain drugs. A standard warning might not apply to you. That’s why pharmacogenomic testing is becoming more common-it looks at your DNA to predict how you’ll react to specific medications. It’s not routine yet, but it’s the future.

What You Can Do Today
You don’t need a PhD to protect yourself. Start here:
- Write down every medication and supplement you take-every single one. Include dosages and times.
- Bring that list to every appointment-even if you’ve been there before.
- Ask your pharmacist: “Could any of these interact with each other?”
- Stop drinking grapefruit juice if you’re on a statin.
- Switch from ibuprofen to acetaminophen for pain if you’re on blood pressure meds.
- Never mix alcohol with heart medications, even one drink.
These aren’t suggestions. They’re survival steps.
Final Reality Check
Heart medications save lives. But they can also kill you-if you don’t treat them with respect. The goal isn’t to avoid pills. It’s to take them safely. Every extra drug adds complexity. Every interaction adds risk. And that risk grows exponentially, not linearly.
There’s no magic formula. But there’s a simple truth: the more pills you take, the more you need to be vigilant. Your life depends on it.
Can I take ibuprofen with my blood pressure medication?
No, not regularly. Ibuprofen and other NSAIDs can reduce the effectiveness of blood pressure medications like ACE inhibitors, beta blockers, and diuretics. They can also cause fluid retention, raise blood pressure, and increase kidney damage risk-especially if you already have heart failure. Use acetaminophen (paracetamol) instead for pain relief, and only for short periods.
Is grapefruit juice really that dangerous with statins?
Yes. Grapefruit juice blocks an enzyme (CYP3A4) that breaks down statins like atorvastatin, simvastatin, and lovastatin. Even one glass a day can increase drug levels by 47%, raising your risk of muscle damage and kidney failure. If you’re on one of these statins, avoid grapefruit entirely. Other citrus fruits like oranges and lemons are safe.
Can I take St. John’s Wort for depression if I’m on heart meds?
Absolutely not. St. John’s Wort speeds up how quickly your body removes many heart medications-including beta blockers, statins, and antiarrhythmics. This can cause your drugs to stop working. Your blood pressure may spike, your cholesterol may rise, or your heart rhythm could become dangerous. There is no safe dose when combined with heart meds.
Does alcohol interact with all heart medications?
It interacts with most. Alcohol can lower blood pressure too much, cause irregular heartbeats, increase bleeding risk with blood thinners, and damage the liver when taken with statins. Even one drink a day can interfere. If you have heart failure, arrhythmia, or high blood pressure, the safest choice is no alcohol.
What over-the-counter drugs should I avoid with heart meds?
Avoid decongestants like pseudoephedrine (Sudafed), NSAIDs like ibuprofen or naproxen, first-generation antihistamines like diphenhydramine (Benadryl), and antacids containing aluminum or magnesium if you’re on digoxin or certain antibiotics. Always check with your pharmacist before taking anything new-even cough syrup or sleep aids.
Should I stop taking a medication if I think it’s causing side effects?
Never stop suddenly. Some heart medications, like beta blockers or blood thinners, can cause dangerous rebound effects if stopped abruptly. Call your doctor or pharmacist right away if you feel dizzy, swollen, short of breath, or notice unusual bruising or muscle pain. They can help you adjust safely.
Can I use herbal supplements like turmeric or garlic with heart meds?
Turmeric and garlic can both thin the blood. If you’re on warfarin, apixaban, or aspirin, they can increase bleeding risk. Garlic may also lower blood pressure too much when combined with antihypertensives. There’s no proven benefit that outweighs the risk. Skip them unless your doctor approves.
How often should I review my medications with my doctor?
At least every six months-or every time you see a new doctor, start a new medication, or fill a prescription at a new pharmacy. Many people don’t realize their meds have changed until they’re hospitalized for an interaction. Keep a current list and bring it everywhere.
Is it safe to take supplements with heart medications if my doctor says it’s okay?
Even if your doctor says yes, proceed with caution. Many doctors aren’t trained in supplement interactions. Always ask: “What’s the evidence this helps?” and “What could go wrong?” If there’s no strong reason to take it, it’s often safer to leave it out.
What’s the biggest mistake people make with heart meds?
Assuming that because a pill is prescribed, it’s automatically safe to take with everything else. The biggest danger isn’t the drugs themselves-it’s the assumption that more pills = better care. The truth? Less is often more. Regular reviews and open communication with your care team are the only real safeguards.




Just wanted to say this post saved my life. I was on six meds, including a statin, and drinking grapefruit juice every morning because I thought it was healthy. My legs started aching like I’d run a marathon-I didn’t connect it until I read this. Went to my pharmacist, stopped the juice, and within two weeks the pain faded. Never thought a fruit could nearly kill me. Don’t assume ‘natural’ means safe.
Really appreciate how clear this is. I’ve seen so many older relatives get lost in pill regimens-each doctor adds something, no one takes a step back. The brown bag review idea? Brilliant. My grandma did that last year and ended up ditching three supplements that were doing nothing but costing her $200/month. She said she felt lighter, not just physically, but mentally. Less fear, more clarity.
Why are we even trusting doctors anymore I mean really think about it the pharmaceutical companies own the FDA and your statin is just a money scheme to keep you sick and buying more pills and dont even get me started on grapefruit juice its all a distraction from the real agenda the real danger is the system itself not the meds the meds are just the symptom not the disease
This is why America’s healthcare is a joke. Everyone’s on ten drugs because the system rewards prescribing not healing. I’ve seen patients on 12 meds-none of them needed. They’re just profit centers. Stop blaming grapefruit juice. Blame the pill-pushing machine.
There’s a deeper philosophical tension here: we treat health as a technical problem to be solved with more interventions, when perhaps it’s an existential one requiring restraint. The more we add, the less we listen-to our bodies, to our histories, to the quiet signals of imbalance. The real innovation isn’t in new drugs, but in the courage to stop. To ask: ‘Do I really need this?’ Not ‘What else can I take?’
Look, I get it, you’re all very concerned about your ‘meds’ and your ‘interactions’-but in India, we’ve been managing heart conditions for generations with turmeric, yoga, and fasting. No pills. Just wisdom. You Americans overcomplicate everything. One glass of grapefruit juice? Please. That’s just fearmongering by Big Pharma to sell you more blood thinners. My uncle, 82, takes three pills and a spoon of honey every morning. Still hikes mountains. You’re all just addicted to the system.
Let me ask you something-how many of these ‘safe’ combinations were approved by the FDA after a 3-month trial with 200 people? And how many of those people were over 70? Or had kidney issues? Or took supplements? The data is fabricated. The interactions are buried. The ‘warning labels’ are in 5-point font. This isn’t medicine-it’s a controlled experiment on the elderly, and you’re all just waiting for your turn. I’ve seen the internal memos. They know. They just don’t care.
While the general advice is sound, the post lacks nuance regarding pharmacogenomics. CYP3A4 polymorphisms vary significantly across populations-particularly in South Asian and African descent groups where slow metabolizer phenotypes are more prevalent. The blanket avoidance of grapefruit juice may be unnecessary for individuals with rapid metabolism. Additionally, deprescribing protocols should be stratified by frailty index, not age alone. A 75-year-old with robust renal function and no polypharmacy may tolerate more than a 65-year-old with sarcopenia and CKD. The guidelines cited are population-level heuristics, not individualized medicine.