Most people hear "COPD" and think of one thing: trouble breathing. But behind that single label are two very different diseases - chronic bronchitis and emphysema - that behave, feel, and respond to treatment in completely opposite ways. If you or someone you care about has been diagnosed with COPD, understanding which component is driving the symptoms isn’t just helpful - it can mean the difference between getting better and staying stuck.
What’s Really Going On in Your Lungs?
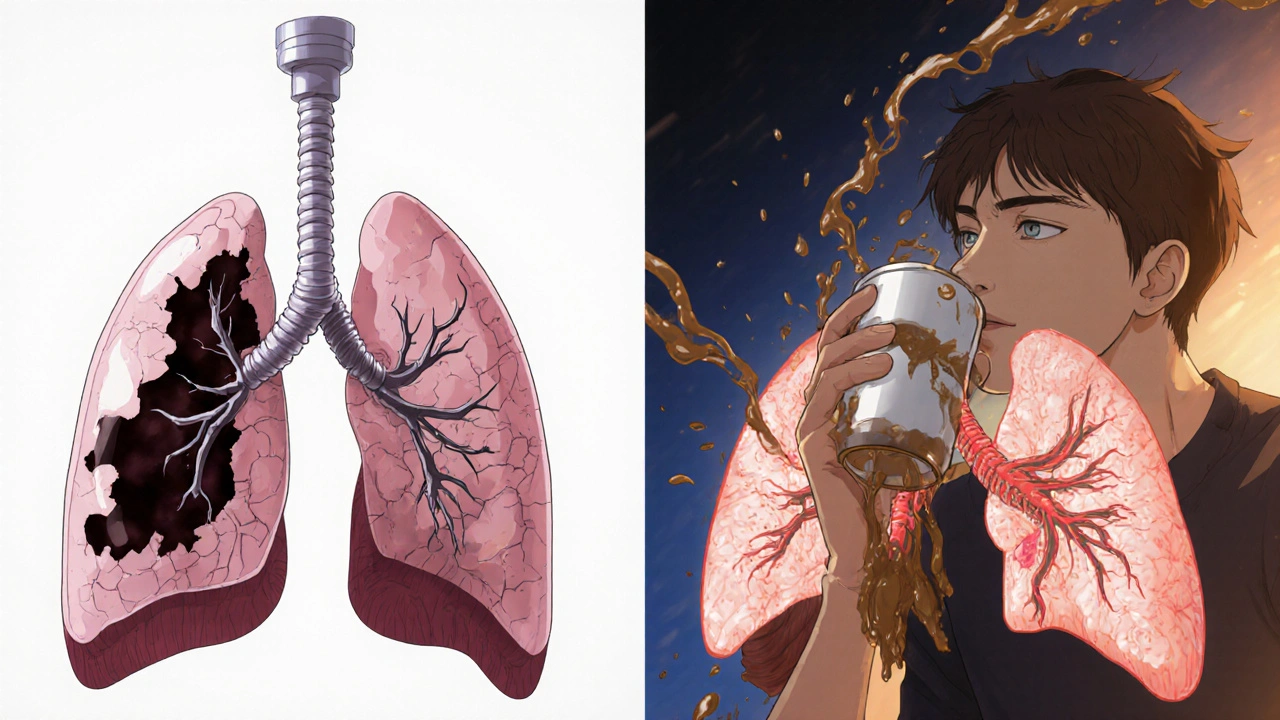
Chronic bronchitis and emphysema don’t just share a diagnosis - they attack your lungs in totally different ways. Think of your lungs like a network of tiny air sacs (alveoli) and branching tubes (bronchi). In emphysema, those air sacs are destroyed. The walls between them break down, turning small, efficient sacs into big, floppy balloons with less surface area to absorb oxygen. That’s why people with emphysema often feel like they can’t get enough air, even when they’re sitting still. Their lungs lose their natural spring, and air gets trapped.
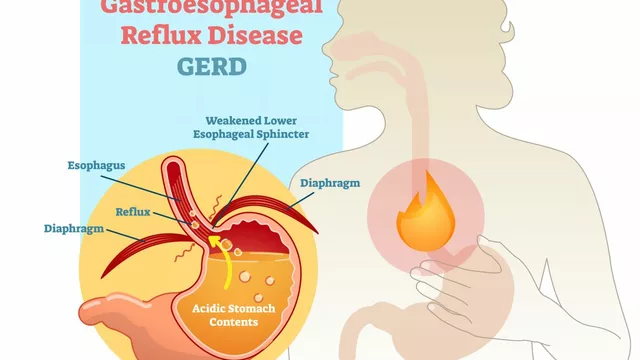
In chronic bronchitis, it’s the tubes that are the problem. The lining swells, produces way too much mucus - up to 200 mL a day, compared to the normal 10-100 mL - and the tiny hairs (cilia) that normally sweep mucus out stop working. This leads to a daily cough that won’t quit, often with thick phlegm. It’s not just annoying; it’s dangerous. That mucus plugs up airways, making breathing harder and increasing the risk of infections.
These aren’t just symptoms - they’re measurable. Pulmonary tests show emphysema patients with a diffusing capacity (DLCO) below 60% of normal, meaning oxygen can’t move from the lungs into the blood efficiently. Chronic bronchitis patients, on the other hand, usually have normal DLCO but show high airway resistance. Their FEV1/FVC ratio drops below 70%, but their lungs still hold oxygen - they just can’t move it in and out easily.
The Pink Puffer and the Blue Bloater: Real-Life Signs
Doctors used to describe two classic types: the "pink puffer" and the "blue bloater." These aren’t medical terms anymore, but they still describe real patterns you’ll see.
The "pink puffer" - usually someone with emphysema - looks thin, breathes fast (25-30 breaths per minute), and has a barrel chest. They’re often not blue because they’re hyperventilating to compensate. Their oxygen levels stay around 92-95%, but they’re exhausted from working so hard just to breathe. You’ll hear them say, "I can’t say more than five words without stopping." They walk slowly, stop often, and avoid stairs.
The "blue bloater" - typically chronic bronchitis - has a different story. Their skin may look slightly blue, especially around the lips and fingertips, because their oxygen levels are low (85-89%). They’re often heavier, with swollen ankles from heart strain caused by long-term low oxygen. Their cough is constant, and they clear mucus for 20-30 minutes every morning. Many say they feel worse in winter, when cold air triggers more mucus and infections.
But here’s the catch: 85% of people with advanced COPD have features of both. That’s why it’s not about labeling someone as one or the other - it’s about understanding what’s driving their symptoms right now.
How Diagnosis Works - Beyond Just a Breathing Test
A simple spirometry test showing low FEV1/FVC tells you someone has COPD. But to know whether it’s mostly bronchitis or emphysema, you need more.
First, DLCO. If it’s below 60% of predicted, emphysema is likely. If it’s normal or only slightly low, chronic bronchitis is probably the main issue.
Then there’s the CT scan. In emphysema, you’ll see dark, patchy areas covering more than 15% of the lung - dead space where tissue used to be. In chronic bronchitis, the airway walls look thickened, with more than 60% of the airway area taken up by inflamed tissue.
The 6-minute walk test also gives clues. Emphysema patients drop their oxygen saturation below 88% within the first two minutes. Chronic bronchitis patients usually stay above 90% - but they stop walking because they’re out of breath from mucus and airway resistance, not because their blood lacks oxygen.
Without these extra tests, you’re guessing. And guessing leads to wrong treatment.

Treatment Isn’t One-Size-Fits-All
One of the biggest mistakes in COPD care is treating everyone the same. But studies show patients who get treatment matched to their phenotype have 27% fewer hospital visits.
For chronic bronchitis, the goal is mucus control. Mucolytics like carbocisteine reduce exacerbations by 22%. Hypertonic saline nebulizers help thin mucus - 73% of users report easier clearing. Roflumilast, a pill that reduces inflammation in the airways, cuts flare-ups by 17.3% in people with frequent exacerbations. But here’s the warning: inhaled steroids, often used for asthma, increase pneumonia risk by 40% in chronic bronchitis patients. So doctors now start with LAMA/LABA combos - long-acting bronchodilators - before even considering steroids.
For emphysema, the focus is on preserving lung function and reducing trapped air. Bronchodilators help, but the real game-changer is lung volume reduction. Endobronchial valves, tiny one-way devices placed via a scope, collapse damaged areas and let healthy lung tissue expand. In the IMPACT trial, patients improved their 6-minute walk distance by 35%. For those with upper-lobe emphysema and very low FEV1 (<35%), surgery can be life-changing.
And if it’s genetic? About 1-2% of emphysema cases are caused by alpha-1 antitrypsin deficiency. These patients need weekly infusions of the missing protein - 60 mg/kg - to slow lung damage. It’s not a cure, but it’s the only treatment that targets the root cause.
What Patients Are Really Experiencing
Real people don’t talk about FEV1 or DLCO. They talk about life.
One man on Reddit said he measures his morning mucus in a cup - 100 mL every day, for eight years. He spends 30 minutes every morning doing chest physiotherapy. He can’t travel far because he needs his nebulizer. Another woman with emphysema says she stopped hugging her grandchildren because she couldn’t catch her breath. She uses oxygen at home, but hates how the tank limits her. "It’s like being chained to a battery," she said.
Both groups struggle with medication routines. Chronic bronchitis patients often have to take 4-6 inhalers a day. Emphysema patients carry portable oxygen concentrators that deliver 2-4 liters per minute - heavy, noisy, and awkward. But both say the same thing: when they get the right treatment, life improves. One chronic bronchitis patient said, "After starting hypertonic saline, I didn’t need antibiotics for a whole year." An emphysema patient who got valves said, "I walked to the end of my driveway for the first time in five years. I cried."
What’s New in 2025?
The field is moving fast. In 2023, the FDA approved inhaled alpha-1 antitrypsin for genetic emphysema - it improved FEV1 by 20% in 12 months. In Europe, a new acoustic device that vibrates mucus loose launched in 2024 and cut exacerbations by 32%.
Researchers are now looking at blood markers. If your eosinophil count is above 300 cells/μL, you’re more likely to respond to new biologic drugs for chronic bronchitis. Clinical trials are underway.
And treatments are getting more targeted. Bronchoscopic thermal vapor ablation, a minimally invasive procedure for emphysema, shows 78% success at two years. New drugs targeting TMEM16A channels - the ones that control mucus production - are in phase 3 trials. This isn’t just about managing symptoms anymore. It’s about fixing the underlying biology.
Why This Matters for You
If you have COPD, don’t accept "it’s just COPD" as an answer. Ask: "Is it mostly bronchitis or emphysema?" Request a DLCO test. Ask about a CT scan. Find out if your treatment matches your type.
Getting the right treatment isn’t about being perfect - it’s about being precise. One wrong medication can make things worse. One right one can give you back hours of your day.
Chronic bronchitis and emphysema are not the same. And treating them like they are? That’s like treating a broken arm and a sprained ankle the same way - because both are "injuries to the limb." You wouldn’t do that. Don’t do it with your lungs either.
Can you have chronic bronchitis and emphysema at the same time?
Yes - and most people with moderate to severe COPD do. While doctors used to classify patients as either "pink puffer" or "blue bloater," research now shows that 85% of advanced COPD cases have features of both conditions. The key isn’t to pick one or the other, but to identify which one is driving the worst symptoms at this moment. Treatment should target the dominant problem first.
Is COPD the same as asthma?
No. While both cause breathing trouble, asthma is usually reversible with medication and often starts in childhood. COPD is progressive, caused mostly by long-term smoking or exposure to lung irritants, and the damage is permanent. Asthma symptoms come and go; COPD symptoms get worse over time. The treatments overlap in some ways, but the goals are different: asthma focuses on controlling inflammation and preventing attacks; COPD focuses on slowing decline and managing symptoms.
Does quitting smoking help if I already have COPD?
Yes - and it’s the most important thing you can do. Quitting doesn’t reverse damage, but it slows the decline in lung function by up to 50%. People who quit after diagnosis live longer, have fewer flare-ups, and respond better to treatments. Even if you’ve smoked for 40 years, quitting at age 60 still adds years to your life. No medication works as well as stopping smoking.
What’s the best way to clear mucus if I have chronic bronchitis?
Three proven methods: hypertonic saline nebulizers (7% salt solution), chest physiotherapy (like postural drainage and percussion), and mucolytics like carbocisteine. Some patients also benefit from newer acoustic devices that vibrate mucus loose. Drinking plenty of water helps thin mucus naturally. Avoid antihistamines and decongestants - they dry out secretions and make them harder to clear.
When should I consider lung volume reduction surgery for emphysema?
Consider it if you have severe upper-lobe emphysema, FEV1 below 35% of predicted, and you’re still struggling despite optimal medication. The procedure works best when the damage is uneven - mostly in the upper lungs. Endobronchial valves (a less invasive option) have a 65% success rate at one year and are now preferred over traditional surgery for most patients. Talk to a pulmonologist who specializes in COPD to see if you’re a candidate.
Can I still exercise with COPD?
Absolutely - and you should. Exercise doesn’t fix your lungs, but it strengthens your muscles, including your breathing muscles. A pulmonary rehab program - which includes walking, cycling, and strength training - improves your ability to do daily tasks by 30-40%. Many patients report feeling less breathless after just 6 weeks. Start slow: 5-10 minutes a day, three times a week. Use oxygen if prescribed. The goal isn’t to run a marathon - it’s to walk to the mailbox without stopping.



Man, this is the clearest breakdown of COPD I’ve ever read. I had no idea emphysema and bronchitis were basically different diseases wearing the same label. My uncle’s been labeled ‘COPD’ for years and they kept giving him steroids-he kept getting pneumonia. Now I get why. This should be mandatory reading for every GP.
Let me tell you something-this isn’t just medical info, this is life-changing stuff. I spent six months watching my dad struggle, thinking he was just getting old. Turns out he’s a classic blue bloater: morning cough, swollen ankles, oxygen levels dipping to 87% by dinnertime. We switched from steroids to LAMA/LABA combo after reading this, and holy hell-he’s walking to the mailbox now without stopping. That 27% drop in hospital visits? Real. I’m sending this to every family member who’s ever said ‘he’s just out of breath.’
And don’t even get me started on the pink puffer myth. People think they’re ‘strong’ because they’re thin and breathing hard, but they’re literally exhausting their bodies trying to stay alive. That’s not grit-that’s a failing engine screaming for help. We need better public awareness. This post deserves a TED Talk.
Wow. So much text for ‘your lungs are broken in two different ways.’
They’re letting this kind of info out now? Who’s paying for these studies? Big Pharma’s pushing this so we don’t question why they’re selling the same inhalers for 50 years. Bronchitis? Emphysema? Just say ‘smoker’s lung’ and save us all the BS. And why do they care if you’re pink or blue? It’s all the same damn disease-your lungs are trash and you did it to yourself.
They’ll tell you about valves and nebulizers next. Next thing you know, they’ll be charging $20,000 for a tiny plastic tube to fix what you broke by smoking a pack a day since 1992. Wake up, sheeple.
This is a remarkable synthesis of clinical data and patient experience. I’m curious-how prevalent is phenotyping in primary care settings outside academic hospitals? In many rural U.S. clinics, spirometry is the only tool available, and even that’s often underutilized. Is there any data on how often patients receive CT scans or DLCO testing in the first year post-diagnosis?
Also, I’d be interested in cross-cultural comparisons. In countries with universal healthcare, is there a higher rate of accurate phenotyping? Or does socioeconomic status override diagnostic precision regardless of system?
cops dont even know the diffrence between bronchitis and emphysema they just give u the same inhaler and tell u to stop smoking like its that easy. i bet the gov is hiding the real cause like 5g or chemtrails or something. why do u think the lung tests changed after 2010? its all a scam. i had a cousin who got better after drinking apple cider vinegar and sleeping in a pyramid. they dont want u to know that.
You say 85% have both? That’s not a gray area-that’s a failure of diagnosis. If you can’t tell which one’s dominant, you’re not a doctor, you’re a guesser with a stethoscope. And why are we still using terms like ‘pink puffer’? Sounds like something from a 1950s medical textbook. If you’re going to use slang, at least make it accurate. ‘Gasping Skeleton’ and ‘Mucus Monster’ would be more honest.
Let’s be real-this whole ‘phenotype’ thing is just a fancy way to sell more drugs. Mucolytics? Endobronchial valves? $15,000 procedures? Meanwhile, the real solution is simple: stop smoking. No tests. No pills. No valves. Just quit. But if you make it complicated, people keep paying. The system doesn’t want you cured-it wants you managed.
And don’t get me started on ‘hypertonic saline.’ That’s just salt water. You can make that at home. Why charge $50 a nebulizer treatment when you can boil water and add salt? This is capitalism disguised as medicine.
I appreciate how this breaks down the science without drowning you in jargon. My mom was misdiagnosed for three years as just having ‘asthma.’ She was a blue bloater-constant cough, mucus in the morning, no wheezing. Once they did the DLCO and CT scan, everything clicked. She started on roflumilast and now she’s sleeping through the night. It’s not just about breathing-it’s about dignity. Thank you for writing this.
I just cried reading this. My dad passed last year from COPD and they never told us the difference between bronchitis and emphysema. He was the pink puffer-thin, always out of breath, never blue. We thought he was just weak. Now I realize he was fighting his lungs every second. I wish I’d known this before. I would’ve pushed harder for the right tests. I’m sharing this with everyone I know.
Excellent overview. This aligns with the latest GOLD guidelines on COPD heterogeneity. I’d add that phenotyping also impacts rehabilitation protocols-emphysema patients benefit more from endurance training, while bronchitis patients need airway clearance techniques and infection prevention. The treatment tailoring you describe is exactly what integrated pulmonary rehab programs are moving toward. More centers need to adopt this model.
So what you’re saying is… if you’re a lazy smoker who won’t quit, we should give you a $20K valve instead of just telling you to stop? Classic American healthcare. We’d rather fix the machine than fix the idiot who broke it. Next they’ll be selling oxygen tanks with a ‘You Could’ve Quit’ sticker on them.