When you’ve been on a biologic drug for years - maybe infliximab or adalimumab - your body knows it. Your symptoms are under control. Your blood tests look good. Then your doctor says, "We’re switching you to a biosimilar." You might feel confused, even anxious. Is this just a cost cut? Will you feel worse? Will your disease come back? The truth is, switching from an originator biologic to a biosimilar isn’t a gamble. It’s backed by over a decade of real-world data from tens of thousands of patients across Europe and the U.S.
What Exactly Is a Biosimilar?
A biosimilar isn’t a generic. Generics are exact copies of small-molecule drugs like aspirin or metformin. Biosimilars are copies of complex biological drugs made from living cells - proteins, antibodies, or enzymes. These molecules are too big and too intricate to be replicated exactly. But they don’t need to be. Regulatory agencies like the FDA and EMA require biosimilars to match the originator in quality, safety, and effectiveness with no clinically meaningful differences. That means your immune system reacts the same way. Your disease stays controlled. Your side effect profile stays unchanged.
Think of it like two different brands of insulin. They’re made differently, but they lower your blood sugar the same way. The same applies to biosimilars of drugs like Humira (adalimumab) or Remicade (infliximab). The first U.S. biosimilar, Zarxio (filgrastim-sndz), was approved in 2015. Since then, 37 biosimilars have cleared FDA review, mostly targeting autoimmune conditions like rheumatoid arthritis, psoriasis, and inflammatory bowel disease.
What Happens When You Switch?
Switching doesn’t mean starting over. It’s not like changing from one painkiller to another. When you switch from an originator biologic to a biosimilar, your body doesn’t have to relearn how to respond. Clinical trials and real-world studies show that after the switch, disease activity stays stable. In the NOR-Switch study, 481 patients with rheumatoid arthritis, psoriatic arthritis, or inflammatory bowel disease were switched from originator infliximab to its biosimilar CT-P13. At one year, 52.6% stayed on the biosimilar. The group that stayed on the originator? 60%. The difference wasn’t statistically significant. No surge in flares. No spike in hospitalizations.
In a 2021 study of 140 patients with chronic inflammatory disease, researchers tracked immunogenicity - the body’s tendency to build antibodies against the drug - across multiple switches: from originator to biosimilar, then to another biosimilar. Only 3 out of every 100 patient-years developed new antibodies. That’s lower than the rate seen in patients who never switched. Trough levels - the amount of drug left in your blood between doses - stayed almost identical: 4.3 μg/mL before switching, 4.1 μg/mL after.
Why Do Some People Stop Taking It?
If the science says it’s safe, why do some patients discontinue? The answer isn’t clinical. It’s psychological.
A 2021 study in Frontiers in Psychology found that 32.7% of patients reported new or worsening symptoms after switching - even though lab tests and doctor assessments showed no actual disease flare. This is called the nocebo effect: expecting something to go wrong makes you feel it. Reddit threads from patients with rheumatoid arthritis are full of posts like, "I switched to the cheaper version and suddenly I’m exhausted again." But when doctors checked their DAS28 scores (a standard measure of RA activity), their disease was still in remission.
Real reasons for stopping are usually minor: injection-site redness, a headache, or a vague feeling of "not being right." In one adalimumab biosimilar study, 7.8% of patients reported skin reactions - but only 2% of those were confirmed as drug-related. Most were coincidental. Still, those small discomforts can feel huge when you’ve been stable for years.
Another factor? Lack of communication. If you’re told, "We’re switching you," without explanation, you’re more likely to feel like a lab rat. But when patients get a 20-minute counseling session before switching - with clear info on what to expect - discontinuation drops from 18% to just 6.4%, according to the PERFUSE study.
Is Switching Safe Between Biosimilars?
What if you’ve already switched once - from originator to biosimilar - and now your insurer wants you to switch again? To another biosimilar?
It’s happening more often. In Europe, where biosimilar adoption is high, multiple switches are common. The NOR-SWITCH II extension study followed patients for two years and tracked those who switched more than once. Retention after 24 months? 89.2%. That’s higher than many people expected.
But not all studies agree. A 2022 Spanish study found a 15.3% discontinuation rate after switching from one infliximab biosimilar (CT-P13) to another (SB2) in IBD patients - higher than the 8.7% seen in those who never switched. Yet here’s the catch: trough levels didn’t drop. Antibody levels didn’t spike. The patients didn’t get sicker. They just stopped taking it because they felt different.
That’s the paradox. The science says it’s safe. The patient experience says it’s unsettling. The key is distinguishing between perceived change and real clinical risk.
Cost Savings and Access
Why are we doing this? Money. But not in the way you think.
Originator biologics cost $20,000 to $30,000 a year. Biosimilars launch at 15% to 35% less. In 2023, Humira biosimilars entered the U.S. market at a 35% discount. That’s not just savings for insurers. It’s access for patients who couldn’t afford treatment before. In Australia, where public drug coverage is strong, biosimilars have cut biologic spending by 40% since 2020 without increasing hospitalizations.
Health plans now mandate switches. By 2023, 85% of U.S. health plans required patients to switch to biosimilars if available. In Europe, over 60% of filgrastim prescriptions are biosimilars. These aren’t just theoretical savings - they’re freeing up billions to fund other treatments.

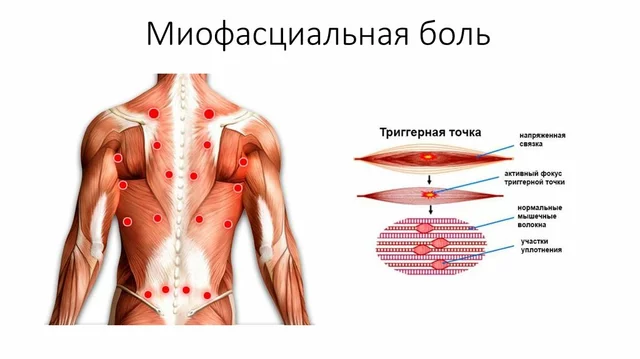
When Switching Might Not Be Right
Biosimilar switching isn’t for everyone. If your disease is active - your DAS28 score is above 3.2, your fecal calprotectin is high, your PASI score is over 10 - switching isn’t advised. Stability is key. You’re not switching to fix a problem. You’re switching to maintain control.
Also, if you’ve had multiple switches already, or if you’ve developed antibodies to the originator, your doctor may hold off. The data on repeated switching is still growing, and while it looks promising, caution is still warranted in complex cases.
And if you’re pregnant, planning to be, or breastfeeding - talk to your doctor. Most biosimilars are considered safe, but data is more limited than for originators. Shared decision-making matters here.
What You Can Do
If you’re being asked to switch:
- Ask for a clear explanation: "Why now? What’s different?"
- Request a pre-switch counseling session - even if it’s not offered.
- Ask about monitoring: Will you check your trough levels? Your disease score? How often?
- Keep a symptom journal for the first three months. Note energy, pain, fatigue - not just flares.
- Don’t assume every new symptom means the drug failed. Stress, sleep, infection - all can mimic flare symptoms.
Most importantly: don’t stop taking it without talking to your doctor. Stopping a biologic cold turkey can trigger a severe flare.
The Bottom Line
Biosimilar switching isn’t experimental. It’s routine. It’s safe. It’s effective. The evidence is overwhelming: your disease won’t flare because you switched. Your body won’t reject the new version. Your immune system won’t suddenly turn on you.
What might change? Your out-of-pocket cost. Your pharmacy’s label. Maybe your peace of mind - temporarily.
For every patient who feels worse after switching, dozens more report no change at all. In the DANBIO registry, 68% of patients switching from originator infliximab to its biosimilar reported no issues. The rest? They got answers. They got support. And their disease stayed in remission.
The future of biologic treatment isn’t about sticking with the original brand. It’s about getting the right medicine - at the right price - without compromise. Switching isn’t a step backward. It’s a step forward for the whole system - and for you, if you’re ready for it.
Is switching to a biosimilar safe for my condition?
Yes, for most people with stable autoimmune conditions like rheumatoid arthritis, psoriasis, or inflammatory bowel disease. Studies involving over 10,000 patients show no increase in flares, serious side effects, or hospitalizations after switching from originator biologics to biosimilars. The FDA and EMA both confirm biosimilars have no clinically meaningful differences in safety or effectiveness.
Will I feel different after switching?
Some people report feeling different - more tired, more achy, or anxious - but that’s often due to the nocebo effect, not the drug itself. Studies show these feelings usually fade within weeks. If your doctor checks your disease activity scores and lab values, they’ll likely show no change. Keeping a symptom journal can help you tell the difference between real flare and psychological discomfort.
Can I switch back to the originator if I don’t like the biosimilar?
Yes, you can. If you’re truly not tolerating the biosimilar - and your doctor confirms your disease is worsening - switching back to the originator is possible. However, this isn’t always covered by insurance. Make sure to document your symptoms and discuss your concerns early. Most patients who switch back do so because of perceived issues, not confirmed clinical failure.
Are biosimilars as effective as the original drug?
Yes. Clinical trials and real-world data show biosimilars match the originator in how well they control disease. For example, in IBD patients switching from originator infliximab to the biosimilar CT-P13, 90.6% maintained remission. In psoriasis, drug retention rates after switching were nearly identical to staying on the originator. The difference isn’t in effectiveness - it’s in cost.
Why do some countries allow automatic substitution while others don’t?
In the U.S., only "interchangeable" biosimilars can be substituted at the pharmacy without doctor approval. The FDA requires extra studies to prove switching back and forth won’t change outcomes. The EMA doesn’t require this - they consider all biosimilars switchable because the data shows safety. Australia follows a similar model to Europe. The difference is regulatory philosophy, not science.
What if I’m worried about my immune system reacting?
Immunogenicity - your body making antibodies against the drug - is monitored closely in switching studies. Data from multiple trials shows antibody formation rates are low and similar whether you switch or stay on the originator. In one study of patients who switched twice, antibody rates were only 3 per 100 patient-years. That’s less than the rate seen in people who never switched. Your doctor can check your drug levels and antibody status if you’re concerned.


Switching to a biosimilar was the best decision I ever made for my RA. I was terrified at first, but my doctor walked me through the data, and after three months, I felt exactly the same-just with a $15 co-pay instead of $300. No flares, no weird side effects. If you’re worried, track your symptoms. You’ll likely see it’s all in your head, not your joints.
The FDA’s approval of biosimilars is not a scientific triumph-it is a bureaucratic surrender to corporate cost-cutting disguised as progress. These molecules are not identical, and to claim otherwise is to ignore the fundamental biology of protein folding, glycosylation, and immunogenicity. We are treating patients like data points in a spreadsheet, not human beings with immune systems that remember.
They’re switching us to biosimilars because Big Pharma and the government are in cahoots. You think this is about savings? Nah. It’s about tracking you. The new drug has a microchip. They’re monitoring your body’s response so they can sell you more stuff later. Read the fine print on the label. It’s all there if you know where to look.
It is my profound conviction, grounded in empirical evidence and international clinical consensus, that the transition from originator biologics to biosimilars constitutes a paradigmatic advancement in equitable healthcare delivery. The regulatory frameworks of the EMA and FDA, while differing in nomenclature, converge upon an identical epistemological foundation: clinical equivalence. To resist this transition is to prioritize perceived familiarity over demonstrable efficacy and public health stewardship.
Switching to biosimilars changed my life. No more $2K/month bills. I’m still in remission. My DAS28? Still 1.8. The only thing that changed? My wallet. Stop overthinking it. Your body doesn’t care what’s on the label-it cares if the drug works. And it does.
You say the science says it’s safe, but have you ever met someone who actually got worse after switching? No? Because they’re too scared to speak up. The system silences dissent. They call it ‘nocebo’ when you feel worse, but if you feel better on the originator, that’s just ‘confirmation bias.’ Double standards. Classic.
I switched and woke up one morning with my skin crawling. My doctor said it was stress. But I know. They swapped my medicine for something that’s basically a knockoff. I’m not a guinea pig. I’m not paying $50 to be someone’s experiment. This is how they get us hooked on cheaper junk. Next they’ll switch my insulin to a generic version made in a basement.
Look, I get it. It’s scary to change something that’s been working. But if you’ve been stable for years, this isn’t a risk-it’s an opportunity. The data doesn’t lie. And if you’re worried, talk to your doctor. Ask for the study numbers. Read the patient stories. You’ll find most people are fine. And if you’re not? You can switch back. No shame in that. Just don’t let fear make the decision for you.
In India, we’ve been using biosimilars for over a decade. They’re not perfect, but they’re life-changing for people who couldn’t afford treatment. I’ve seen patients go from bedridden to walking again-on biosimilars. The fear isn’t about the drug. It’s about losing control. But sometimes, control is an illusion. What matters is function. What matters is survival. The science is clear. The rest is noise.
Biosimilars are not inferior. They are equivalent. The data is overwhelming. The FDA says so. The EMA says so. The real question is why anyone would oppose access to affordable treatment. If you’re not worse off, why resist? The cost savings are real. The outcomes are real. The fear? That’s just fear.
I switched to the biosimilar and didn’t tell anyone. I was scared. But after a month, I realized I felt the same. My pain didn’t come back. My energy didn’t drop. I just saved $200 a month. No drama. No magic. Just science and savings. If you’re thinking about switching, do it. You’ve got nothing to lose but the bill.
Oh, so now we’re supposed to trust the system? The same system that told us Vioxx was safe? The same system that let Big Pharma price Humira at $70,000 a year? Biosimilars are just the next chapter in the same book: profit before people. The data? It’s funded by the same companies selling the drugs. Of course they say it’s safe. What else would they say?
I switched last year. Felt weird for two weeks. Then nothing. My doctor checked my labs. Everything’s normal. I don’t know why I was so scared. Sometimes the scariest part is the thought of change, not the change itself.
Let’s be real. The only reason biosimilars exist is because the originators are about to lose patent protection. This isn’t science-it’s capitalism. They’re not trying to help you. They’re trying to make money. And you’re being sold a lie that it’s safe because the numbers look good on paper. But what about the 5% who get wrecked? Where’s their story? It’s buried in the appendix.