Asthma Food Trigger Checker
How This Tool Works
Select foods you eat regularly to see if they're likely to help or trigger your asthma. Based on research showing how diet influences airway inflammation.
Your Asthma-Friendly Report
Great choices!
These foods support your asthma management by reducing inflammation and improving lung function.
Potential triggers
These foods may increase inflammation or trigger symptoms in sensitive individuals.
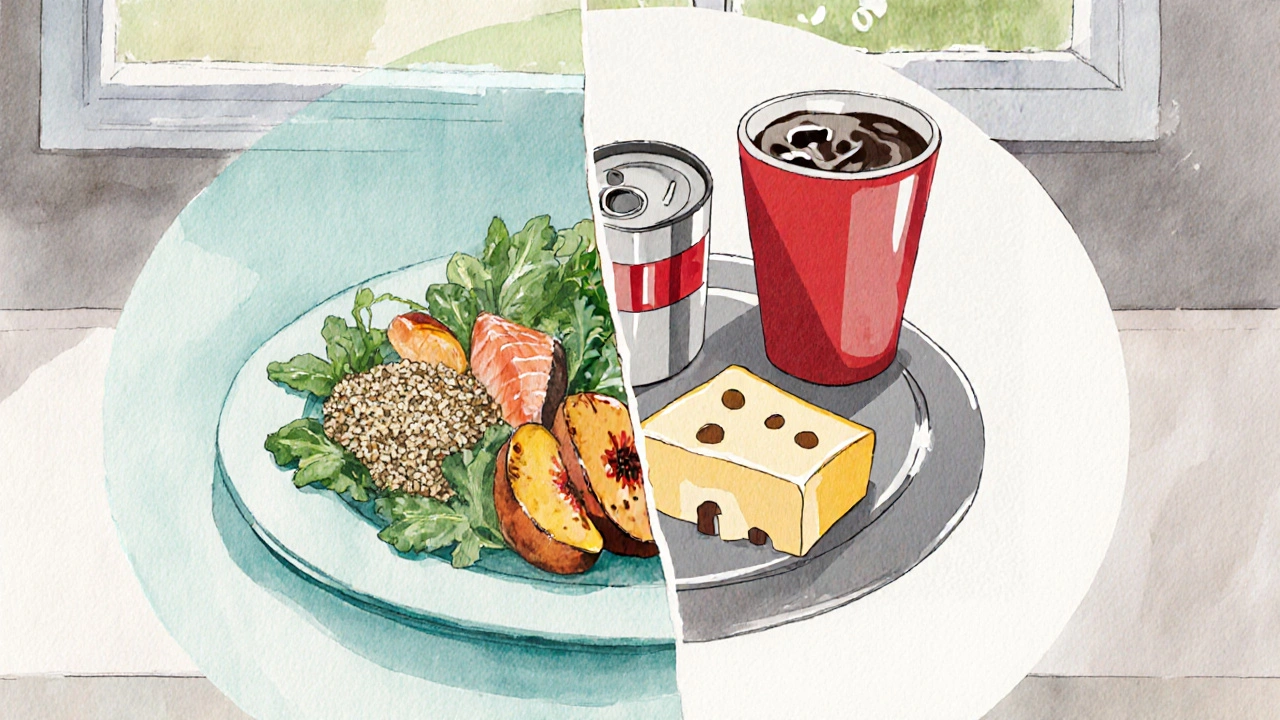
When it comes to managing Asthma is a chronic inflammatory disease of the airways that causes wheezing, shortness of breath, and coughing, many focus on inhalers and medication. Yet diet refers to the foods and drinks you regularly consume plays a surprisingly strong role in either calming or aggravating those airway eruptions. Below you’ll discover how what you eat can act like a silent partner in preventing attacks, which foods act as natural allies, and which hidden culprits should stay off the menu.
Why Food Matters: The Link Between Diet and Airway Inflammation
Asthma’s core problem is inflammation of the bronchial tubes. Certain nutrients can either dampen that inflammation or trigger it. For instance, antioxidants are compounds that neutralize free radicals and reduce oxidative stress protect airway lining from damage, while high‑sugar diets boost inflammatory cytokines that fan the fire. Research from the 2023 International Allergy Journal showed that people who followed a Mediterranean‑style eating pattern experienced 30% fewer severe attacks compared with a standard Western diet.
Anti‑Inflammatory Powerhouses to Add to Your Plate
Here are the top foods that consistently show up in studies as helpers for asthma control:
- Fatty fish (salmon, mackerel, sardines) - rich in omega‑3 fatty acids essential fats that lower production of inflammatory eicosanoids. Aim for two servings per week.
- Leafy greens (spinach, kale, Swiss chard) - packed with magnesium a mineral that relaxes bronchial muscles and improves lung function. One cup cooked daily can make a difference.
- Colorful fruits (berries, oranges, kiwi) - loaded with vitamin C and various antioxidants that protect the airways from oxidative damage.
- VitaminD‑rich foods (fortified dairy, egg yolks, mushrooms exposed to UV) - low serum vitaminD is linked to higher asthma exacerbation rates. Aim for 800-1,000 IU daily from food and safe sun exposure.
- Nuts & seeds (walnuts, chia, flaxseed) - another source of omega‑3s plus fiber that supports a healthy gut microbiome, an emerging player in immune regulation.

Key Nutrients That Directly Support Lung Health
While whole foods are the easiest way to get a blend of nutrients, it helps to know which ones matter most:
- Omega‑3 fatty acids - EPA and DHA reduce airway inflammation and improve bronchodilator response.
- Magnesium - helps relax smooth muscle in the bronchi, lowering the risk of spasms during an attack.
- VitaminD - modulates immune function, decreasing the likelihood of allergic sensitisation.
- VitaminC - combats oxidative stress and may improve lung function in children with asthma.
- Quercetin - a flavonoid found in apples and onions that stabilises mast cells, limiting histamine release.
Common Food Triggers and What to Limit
Even if you love a certain snack, it might be silently sparking your airways. The culprits often fall into three groups: additives, sulfites, and high‑glycaemic foods.
- Sulfites - preservatives found in dried fruits, wine, and some processed meats. They can provoke bronchoconstriction in sensitive individuals. Look for labels that say “no sulfites added.”
- Processed foods - contain hidden trans fats, refined sugars and food dyes that boost inflammatory markers. Fast food burgers and sugary sodas belong here.
- Dairy for some - while not a universal trigger, full‑fat milk and cheese may increase mucus production in a subset of asthmatics. Try lactose‑free or low‑fat alternatives if you notice a pattern.
- Food allergens - peanuts, shellfish, soy, and eggs can trigger allergic asthma. If you have a known allergy, strict avoidance is essential.
Practical Meal‑Planning Tips to Stay on Track
Turning theory into habit is the real challenge. Below is a simple weekly template that balances the anti‑inflammatory heroes with safe, satisfying meals.
| Category | Example Food | Key Nutrient / Trigger | Why It Helps or Hurts |
|---|---|---|---|
| Eat | Salmon (grilled) | Omega‑3 (EPA/DHA) | Reduces airway inflammation and improves bronchodilator response. |
| Eat | Spinach salad with olive oil | Magnesium, Antioxidants | Relaxes bronchial muscles and protects airway cells. |
| Avoid | Canned peaches (in syrup) | Sulfites | Can trigger bronchoconstriction in sensitive people. |
| Avoid | Sugar‑laden soda | High sugar, artificial colour | Elevates inflammatory cytokines and may increase mucus. |
Sample day:
- Breakfast: Greek yogurt (or plant‑based if dairy‑sensitive) topped with blueberries and a sprinkle of ground flaxseed.
- Mid‑morning snack: A handful of walnuts.
- Lunch: Quinoa bowl with grilled salmon, roasted sweet potatoes, spinach, and olive‑oil drizzle.
- Afternoon snack: Carrot sticks with hummus (check for no added sulfites).
- Dinner: Stir‑fried tofu, broccoli, and bell peppers in ginger‑garlic sauce, served over brown rice.
Adjust portions to match your calorie needs, but keep the core idea: plenty of omega‑3s, magnesium‑rich greens, and low‑sulphite, low‑additive foods.
Quick Checklist - Daily Asthma‑Friendly Eating Rules
- Include at least one omega‑3 rich protein source (fish, walnuts, chia).
- Fill half your plate with colorful vegetables or leafy greens.
- Choose fresh fruit over canned or dried fruit with preservatives.
- Swap sugary drinks for water, herbal tea, or fortified plant milks.
- Read labels - avoid “sulphite,” “artificial colour,” and “high‑fructose corn syrup.”
- If you notice a pattern, keep a food‑symptom diary for 2‑4 weeks to spot hidden triggers.
Frequently Asked Questions
Can a specific diet replace inhalers for asthma?
No. Diet is a supportive tool, not a cure. You should always follow your doctor’s prescription plan while using food as an extra layer of protection.
Is dairy always bad for asthma?
Only a minority of asthmatics react to dairy. If you notice more mucus after a cheese or milk snack, try a low‑fat or lactose‑free option and see if symptoms improve.
How long does it take to see diet‑related improvements?
Most people notice reduced night‑time coughing or fewer rescue‑inhaler uses within 4-6 weeks of consistent dietary changes.
Are supplements a good shortcut?
Supplements can help fill gaps (e.g., vitaminD or omega‑3 capsules) but whole foods offer a broader mix of protective compounds. Use supplements only after discussing with a healthcare professional.
What role does the gut microbiome play in asthma?
A diverse gut microbiome, fed by fiber‑rich fruits, veggies, and fermented foods, helps regulate immune responses and may lower the chance of allergic airway inflammation.
Putting the right foods on your plate isn’t a magic bullet, but it’s a practical, everyday way to shrink the odds of a nasty asthma flare‑up. Pair an asthma diet with your prescribed meds, stay active, and you’ll likely breathe a little easier.





Look, if you think you can just toss a few berries into your diet and magically cure your asthma, you’re living in a fantasy. The truth is that dietary choices are a responsibility, not a suggestion, and ignoring the science does more harm than good. You need to prioritize omega‑3 rich fish, magnesium packed greens, and cut out the sugary sodas that fan the flames of inflammation. Anything less is just a half‑hearted attempt at health that ends up feeding the very problem you’re trying to avoid. So stop treating this like a trend and start treating it like a commitment to your lungs.
Hey there, I totally get how overwhelming all this info can be. The good news is that you don’t have to overhaul everything overnight – start by adding a serving of salmon or a handful of walnuts a few times a week and swap out one soda for water each day. Over time you’ll notice the difference in how your breathing feels, especially at night. Keep tracking what you eat and how you feel; it’s the best way to spot personal triggers and successes.
Honestly, this “diet fixes asthma” hype feels like another wellness fad. You can’t ignore that the biggest factor is still proper medication and a well‑controlled environment. People will tell you to ditch dairy and blame it for mucus, but the evidence is mixed at best – it’s a personal trigger, not a universal rule. So take the advice with a grain of salt and focus on what your doctor says.
The article attempts to synthesize nutritional biochemistry and epidemiological findings yet it falters by inserting colloquial admonitions that undermine its scholarly tone. While the inclusion of omega‑3 fatty acids as anti‑inflammatory agents aligns with current literature, the discourse neglects to address dose‑response relationships, thereby limiting its applicability for clinicians seeking evidence‑based guidelines. Moreover, the categorical avoidance of dairy fails to acknowledge inter‑individual variability, a nuance essential for precision nutrition. In essence, the piece presents a binary view of complex pathophysiology which, while accessible, oversimplifies the multifactorial nature of asthma management.
Nice effort, but looks like a lot of fluff. 🙄
Absolutely love the positive spin! 🌟 Small daily steps like adding a salmon fillet or swapping soda for sparkling water can truly empower you to breathe easier. Keep pushing forward, and remember that consistency beats perfection every time! 💪😊
While the article presents useful recommendations, it neglects to cite peer‑reviewed sources for several claims, particularly regarding the purported universal benefit of magnesium. A more rigorous approach would bolster its credibility among professionals.
i hear ya man, but also, dont forget every body diffrent. u can try the recs but if sumthin dont feel right, dont force it – listen 2 ur body and keep it chill.
Consider the broader philosophical implication: we are constantly negotiating with our bodies, trying to align external dietary choices with internal physiological demands. When we treat food merely as a weapon against asthma, we risk reducing a complex, living system to a simplistic battlefield, ignoring the nuanced interplay of genetics, environment, and personal history. This reductionist view can foster aggression toward oneself when “diet failures” occur, undermining the very resilience we aim to cultivate.
Thank you for expanding the discussion. Your philosophical perspective reminds us that nutrition is not merely a list of foods but a dialogue with our bodies and cultures. It is essential to approach dietary changes with humility and awareness of individual variability.
Great points everyone! I’ve been trying the salmon and spinach combo and it really helps with my nighttime cough. If anyone’s looking for easy swaps, try swapping your usual chips for roasted chickpeas – crunchy, satisfying, and way better for the lungs.
Listen up: you either get this right or you keep choking on your own ignorance. 🍽️🚀
Whoa, calm down! 🤗 Food is a tool, not a weapon. Let’s keep it friendly and share what works without the drama.
The relationship between diet and asthma is a complex web of physiological mechanisms, psychosocial influences, and environmental factors that cannot be reduced to simplistic cause‑and‑effect statements. First, omega‑3 fatty acids modulate eicosanoid pathways, leading to a measurable decrease in airway hyper‑responsiveness in controlled trials. Second, magnesium acts as a calcium antagonist in smooth muscle, promoting bronchodilation and reducing the frequency of nocturnal symptoms. Third, vitamin D receptors on immune cells regulate cytokine production, thereby attenuating the Th2‑mediated allergic response that underlies many asthma phenotypes. Fourth, antioxidants such as vitamin C scavenge reactive oxygen species, protecting epithelial integrity from oxidative damage during allergen exposure. Fifth, fiber‑rich diets foster a diverse gut microbiome, which through short‑chain fatty acid production influences systemic inflammation and may indirectly improve lung function. Sixth, sulfites present in processed foods can trigger bronchoconstriction in susceptible individuals, making label scrutiny essential. Seventh, high‑glycemic foods elevate insulin levels, which are linked to increased inflammatory markers like CRP, contributing to airway edema. Eighth, dietary patterns rich in processed meat and trans fats are correlated with higher eosinophil counts, a marker of severe asthma. Ninth, the timing of meals relative to medication administration can affect drug absorption and efficacy, suggesting that a consistent eating schedule may enhance therapeutic outcomes. Tenth, cultural dietary habits shape exposure to allergens such as peanuts or shellfish, which can exacerbate allergic asthma if not properly managed. Eleventh, psychosocial stress associated with restrictive diets can paradoxically increase airway reactivity via the hypothalamic‑pituitary‑adrenal axis. Twelfth, individualized nutrition plans that incorporate genetic testing for polymorphisms in IL‑13 or ORMDL3 can provide targeted interventions. Thirteenth, ongoing research indicates that epigenetic modifications from diet may have transgenerational effects on asthma susceptibility. Fourteenth, patient adherence improves when dietary recommendations are presented as part of a holistic lifestyle plan rather than an isolated prescription. Finally, clinicians must integrate these multifaceted insights into shared decision‑making to empower patients toward sustainable, evidence‑based dietary changes that complement pharmacotherapy.