Antibiotic Yeast Infection Risk Calculator
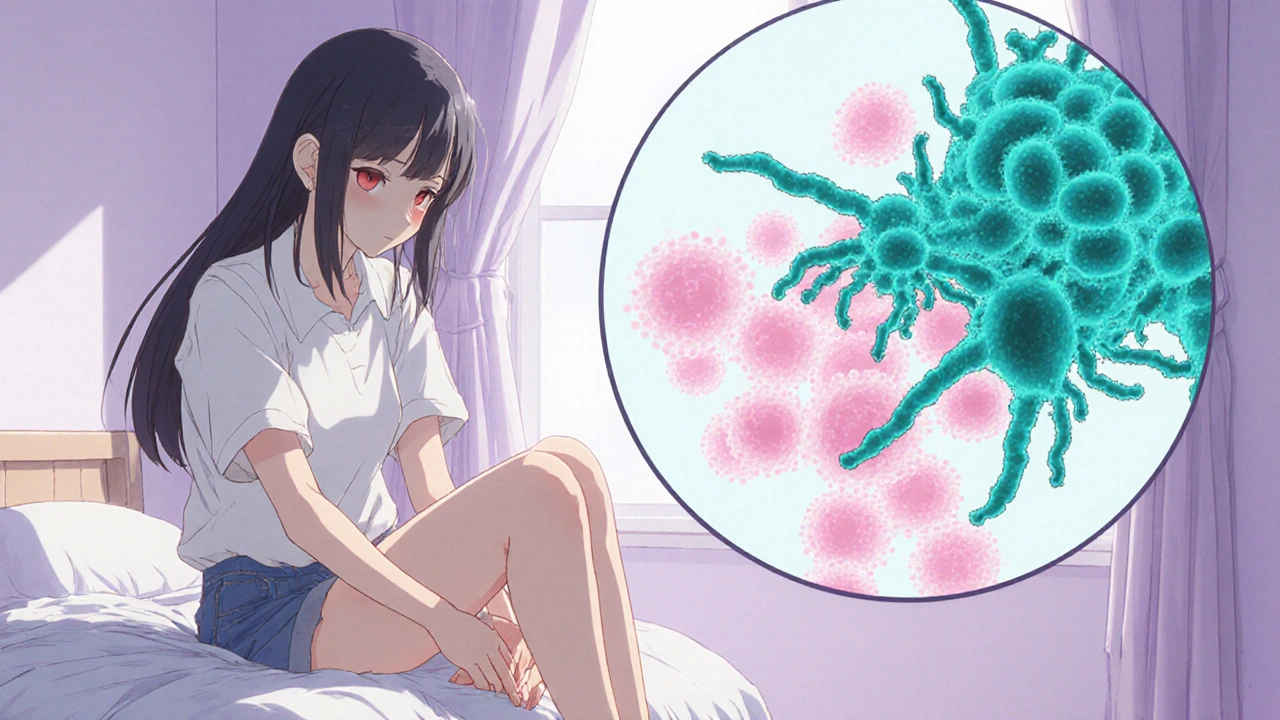
Ever taken a round of antibiotics and then found yourself dealing with intense itching, cottage‑cheese discharge, or a burning sensation? You’re not alone-those uncomfortable symptoms often point to an Antibiotic‑Induced Yeast Infection, a condition that strikes when the good bacteria in the vagina get wiped out and Candida albicans moves in unchecked.
What Happens When Antibiotics Disrupt Your Vaginal Balance
Antibiotics are great at killing harmful bacteria, but they don’t discriminate. Broad‑spectrum drugs such as amoxicillin, ampicillin, and tetracyclines also decimate the Lactobacillus species that produce hydrogen peroxide and keep vaginal pH at a healthy 3.8-4.5. When those friendly microbes disappear, the environment becomes a playground for Candida albicans the yeast responsible for 85‑90% of vaginal infections. The result is the classic yeast infection symptoms that many of us dread.
Who’s Most at Risk?
While anyone taking antibiotics can develop a yeast infection, certain factors raise the odds:
- Uncontrolled diabetes (blood glucose >180 mg/dL) - high sugar feeds yeast.
- Estrogen‑rich states such as pregnancy, hormonal contraception, or hormone therapy.
- Immunocompromised conditions, for example HIV with CD4 < 200 cells/µL.
- Use of SGLT2 inhibitors like empagliflozin (Jardiance), which pushes extra glucose into the urine.
- Frequent douching or scented feminine products that raise vaginal pH above 5.0.
- Tight synthetic underwear that traps moisture and heat.
In fact, a 2023 Evvy survey found that roughly 30 % of people with vaginas report a yeast infection after a course of antibiotics.
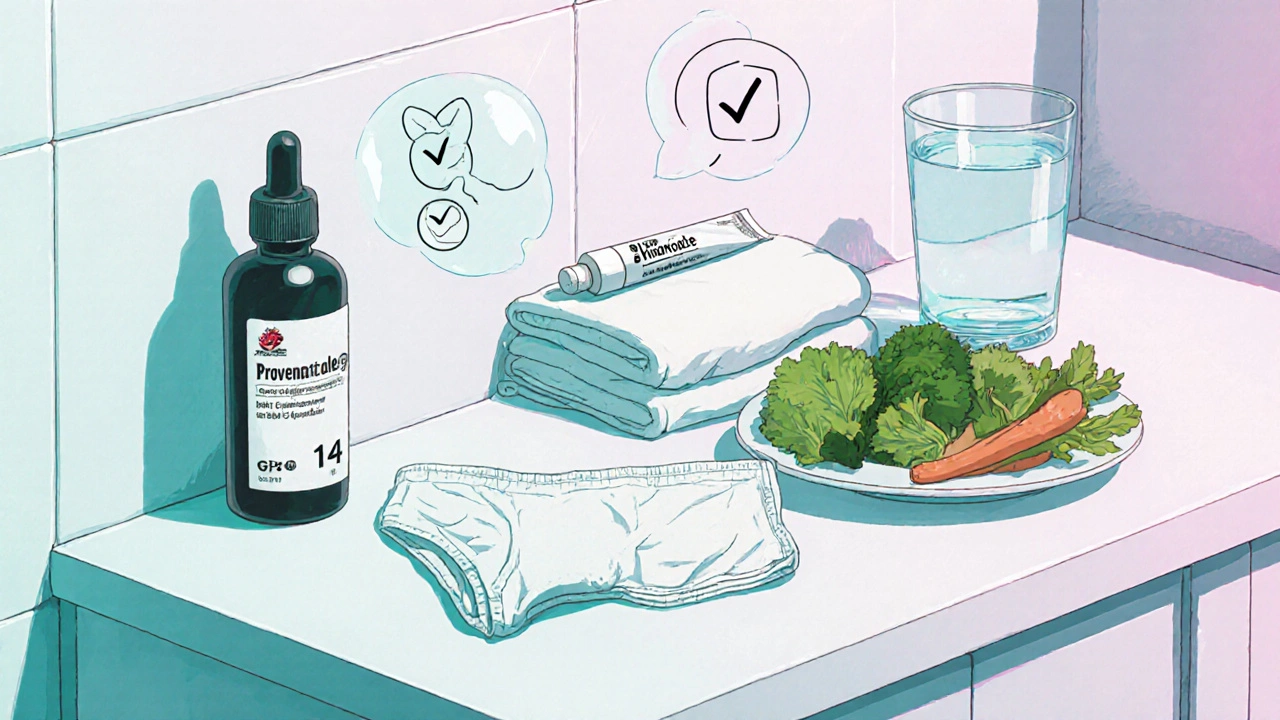
How to Prevent an Antibiotic‑Induced Yeast Infection
Prevention isn’t about magic pills; it’s a bundle of habits that keep the microbial balance in check.
1. Start a Probiotic Early
Research from Intermountain Healthcare shows that taking Lactobacillus rhamnosus GR‑1 and Lactobacillus reuteri RC‑14 at 10 billion CFU daily can slash infection rates by about half. Time it 2 hours before or after each antibiotic dose so the live cultures survive.
2. Pair an OTC Antifungal
Many clinicians recommend a prophylactic course of Miconazole (Monistat) or Clotrimazole (Gyne‑Lotrimin) on the first day of antibiotics. Studies report a 60‑70 % success rate when the antifungal is taken simultaneously.
3. Consider Fluconazole for High‑Risk Patients
If you have diabetes, recurrent infections, or are on hormonal therapy, a single 150 mg dose of Fluconazole on day 1 of antibiotics, then weekly throughout the course, has prevented up to 85 % of cases in clinical trials.
4. Dress Smart
Switch to 100 % cotton underwear. A textile study cited by Medical News Today found cotton keeps vaginal temperature 2‑3 °C lower and reduces moisture by 40 % compared with synthetics, slowing yeast growth dramatically.
5. Cut Simple Sugars
High‑glycemic foods spike blood glucose, which leaks into vaginal secretions and feeds Candida. Cutting down on sugary drinks, white bread, and yeast‑fermented foods can lower vaginal glucose by 20‑30 %.
6. Skip Douching and Perfumed Products
Douching strips away 70‑90 % of protective flora and can raise pH by up to 2 units. Stick to gentle, unscented cleansers instead.
Treatment Options When Symptoms Appear
If prevention fails, act fast. Most uncomplicated infections clear in 7‑10 days with over‑the‑counter (OTC) antifungals.
OTC Options
- Butoconazole (Gynazole‑1): 80‑90 % cure rate in a week.
- Clotrimazole 1 % cream: apply daily for 7 days; a 2022 Cochrane review showed a 15 % boost in success versus a single‑dose regimen.
- Miconazole 2 % suppository: 7‑day course works well for most people.
Prescription Regimens for Complicated Cases
- Fluconazole 150 mg repeat every 72 hours for three doses - about 95 % efficacy.
- For non‑albicans Candida (e.g., C. glabrata), boric acid 600 mg vaginal suppository nightly for 14 days offers ~70 % success.
Special Situations
Pregnant patients can’t take fluconazole in the second or third trimester due to a 4.5‑fold rise in birth defects. In those cases, topical azoles or boric acid are safer choices.
What Not to Do
Antibiotics won’t treat yeast - they make it worse. About 22 % of patients mistakenly add another antibiotic, extending discomfort. Also, self‑diagnosing without a clinician can lead to treating bacterial vaginosis or other conditions with antifungals, which won’t help.
Common Myths and Mistakes
Myth: “If I’m on antibiotics, I’ll definitely get a yeast infection.”
Reality: Risk varies; narrow‑spectrum agents like nitrofurantoin spare more good bacteria and cut infection odds by roughly 30 % compared with broad‑spectrum drugs.
Myth: “A single OTC dose is enough.”
Reality: A 7‑day regimen improves cure rates by up to 15 % over one‑time treatments, especially when the infection is already established.
Myth: “All probiotic supplements work the same.”
Reality: Only products that list specific strains (GR‑1, RC‑14) and deliver ≥10 billion CFU have demonstrated clinically meaningful reductions.

Quick Reference Checklist
- Start probiotic (GR‑1 + RC‑14) 2 hrs before/after each antibiotic dose.
- Take an OTC antifungal (Miconazole or Clotrimazole) on day 1 of antibiotics.
- If high‑risk, ask your doctor about a weekly Fluconazole 150 mg prophylactic.
- Wear cotton underwear; avoid tight synthetics.
- Skip douching, scented wipes, and yeast‑fermented foods.
- Monitor blood sugar; keep glucose <180 mg/dL.
Next Steps
Feeling ready to protect yourself? Talk to your prescriber next time you get an antibiotic. Ask about a narrow‑spectrum option, request a probiotic recommendation, and confirm whether a prophylactic antifungal is appropriate for your health profile. If symptoms sneak up, grab an OTC azole from the pharmacy and start the 7‑day course immediately - the sooner you treat, the quicker you’re back to normal.
Why do antibiotics lead to yeast infections?
Antibiotics kill the Lactobacillus bacteria that keep vaginal pH low. Without that acid‑protective environment, Candida albicans multiplies and causes infection.
Can I prevent a yeast infection while on antibiotics?
Yes. Taking a probiotic (Lactobacillus rhamnosus GR‑1 + L. reuteri RC‑14) together with an OTC antifungal like miconazole, wearing cotton underwear, and avoiding douching dramatically lowers the risk.
What if I’m pregnant?
Avoid fluconazole in the second and third trimesters. Use topical azoles (clotrimazole or miconazole) or boric acid suppositories under a doctor's guidance.
How long does treatment usually take?
Most uncomplicated cases clear in 7‑10 days with OTC creams or suppositories. Prescription regimens for recurrent or severe infections may last 2‑3 weeks.
Are there any foods that help prevent yeast overgrowth?
Focus on low‑glycemic vegetables, healthy fats, and probiotic‑rich foods like yogurt containing at least 1 billion CFU of Lactobacillus acidophilus per serving. Cut back on sugary drinks, white bread, and alcohol, which can raise vaginal glucose.
| Strategy | Typical Dose / Timing | Evidence of Effectiveness |
|---|---|---|
| Probiotic (GR‑1 + RC‑14) | 10 billion CFU daily; start 2 hrs before/after each antibiotic | ~50 % reduction in yeast infections (Intermountain Healthcare, 2023) |
| OTC Antifungal (Miconazole, Clotrimazole) | Begin day 1 of antibiotics; 7‑day course | 60‑70 % prevention success (Healthline, 2023) |
| Fluconazole Prophylaxis | 150 mg on day 1, then weekly during antibiotics | 85 % prevention in high‑risk patients (Mayo Clinic, 2023) |
| Cotton Underwear | Wear 100 % cotton daily | Moisture reduction 40 %; temperature drop 2‑3 °C (Medical News Today, 2023) |
| Dietary Sugar Cut | Eliminate added sugars, refined carbs | Vaginal glucose drop 20‑30 % (Intermountain Healthcare, 2023) |


If you’re on antibiotics, grab a probiotic and start it before the yeast gets a foothold. Don’t wait for the itch to start, act now.
Antibiotics wipe out the good Lactobacillus species, so the vaginal pH climbs and Candida can thrive. Taking a strain‑specific probiotic like GR‑1 and RC‑14 two hours apart from each dose gives the friendly bacteria a chance to survive. Adding an OTC azole on day one creates a double‑layered shield. Simple habits like cotton underwear and ditching douches also help keep the balance.
Oh wow, another “miracle cure” list that pretends we can outsmart microbes with pills. As if the universe would pause while we pop probiotics like candy. Spoiler: most of us just end up with a wallet lighter and a schedule fuller.
Wear cotton and skip scented wipes.
The cascade that follows a blanket antibiotic dose is more than a simple extermination of pathogens. It is a deep ecological disturbance that echoes through the microbiome's hidden networks. When Lactobacilli vanish the pH climbs and Candida finds a foothold. This shift is not random but a predictable outcome of competitive release. The body, in its wisdom, tries to rebalance by feeding the opportunist yeast with extra sugars that leak from the bloodstream. In the context of diabetes or SGLT2 inhibitors that leaky sugar becomes a banquet. The notion that a single probiotic capsule can magically restore equilibrium is a myth; you need strain specificity and timing. GR‑1 and RC‑14 are among the few with documented colonization power. Taking them two hours apart from the antibiotic allows survivorship. Pairing an over‑the‑counter azole on day one creates a hostile environment for the fungus while the probiotic rebuilds the protective flora. Ignoring this dual strategy is akin to patching a roof with a single nail. Moreover, the choice of underwear matters because heat and moisture accelerate fungal growth. Cotton fabrics act like a breathable shield while synthetics trap steam. The cumulative effect of these simple measures can cut infection rates by over half according to recent trials. So think of prevention as a layered defense, not a single bullet.
Thank you for sharing such a thorough guide. The step‑by‑step approach makes it easy to follow, especially the timing of probiotics relative to antibiotics. I also appreciate the emphasis on lifestyle factors like breathable underwear. For anyone feeling overwhelmed, remember that small consistent actions add up to big protection. Keep up the great work! :)
Sure, because everyone loves a daily dose of antifungal with their antibiotics.
Yeast loves sugar so ditch the sweets ok
Listen up folks, this isn’t some boring lecture – it’s a battle plan. If you’re taking broad‑spectrum meds, arm yourself with probiotics, a pump of miconazole, and a pair of cotton boxers. No more letting Candida run wild while you sit on a throne of synthetic fibers. Get aggressive, protect your flora, and show those antibiotics who’s boss!
Oh my god, the moment I read “burning sensation” I was like, “NO! Not again!”
It’s like a tiny hellfire party down there and nobody invited me.
But then I saw the tip about swapping to cotton and it felt like a rescue mission.
Seriously, if you skip the scented wipes you’re basically giving your vagina a mercy‑kiss.
Stay strong, queens, we got this!
I love how detailed this guide is, but let’s be real – most people ignore the simple steps like ditching douches. If you’re already suffering, you probably missed the basics. Start with cotton undies and a probiotic, and maybe you’ll avoid another round of misery.
Picture this: you’re lounging on a sunny Saturday, feeling like the queen of the world, when suddenly a rash of relentless itching crashes your party like a rogue wave. The itch spreads, the discharge becomes a theatrical display, and you’re left wondering if the universe conspired against your comfort. You recall the article’s checklist – probiotics, antifungal, cotton underwear – but you’re too caught up in the drama of the moment to act. Then you remember the line about “high‑glycemic foods feeding the yeast,” and you swear off that sugary latte forever, feeling like a heroine in a health saga. The next day, you dutifully pop a probiotic capsule two hours after your antibiotic dose, as if performing a ritual to appease the microscopic gods. You slide on those breathable cotton briefs, feeling like you’ve donned armor made of clouds. The antifungal cream arrives like a secret weapon, spreading cool relief across the battlefield of your nether regions. By the end of the week, the itching fades, the discharge clears, and you stand victorious, clutching the guide like a trophy. Moral of the story: when life throws yeast at you, fight back with science, style, and a sprinkle of drama. And remember, every heroic journey begins with a single, well‑timed probiotic.
Implementing a prophylactic regimen leverages synergistic microbiome modulation optimizing host‑pathogen equilibrium hence reducing candidal overgrowth risk. Deploy GR‑1/RC‑14 pre‑dose, integrate azole on day one, maintain breathable textiles – outcome: robust resilience.
In the grand tapestry of health, each microbe plays a note in the symphony of balance. When antibiotics silence one section, we must fill the silence with intention and care. A probiotic is not just a supplement, it's a reminder that restoration is possible. Keep the melody alive. :)