Immunosuppressant Vaccine Timing Calculator
Vaccine Safety Assessment
Getting vaccinated while on immunosuppressants isn’t just a matter of showing up at the clinic. It’s a precise balancing act-too early, and the vaccine won’t stick; too late, and you risk infection. For people taking steroids, rituximab, methotrexate, or other immune-weakening drugs, the difference between a live and an inactivated vaccine can mean the difference between protection and serious illness.
Why Live Vaccines Are Off-Limits
Live vaccines contain a weakened version of the actual virus. In healthy people, that’s enough to trigger a strong immune response without causing disease. But for someone on immunosuppressants, that weakened virus can still replicate and cause real illness. The risk isn’t theoretical-it’s documented. The MMR vaccine (measles, mumps, rubella), varicella (chickenpox), and the old Zostavax (shingles vaccine) are all off-limits if you’re moderately or severely immunocompromised.The BC Centre for Disease Control (August 2025 guidelines) is clear: live vaccines are contraindicated unless you’re on very low-dose steroids and your specialist says otherwise. Even then, it’s rare. One patient on Reddit shared how their oncologist accidentally scheduled them for the nasal flu vaccine-LAIV (live attenuated influenza vaccine)-while they were on rituximab. They had to cancel at the last minute after their infectious disease doctor intervened. That kind of mistake happens because many providers don’t track immunosuppression levels closely enough.
Inactivated Vaccines Are Safe-But Not Always Effective
Inactivated vaccines don’t contain live viruses. They use dead virus parts, proteins, or mRNA to teach your immune system what to fight. These are safe for people on immunosuppressants. But here’s the catch: your immune system might not respond well.Studies show that only 15% to 85% of immunocompromised people develop protective antibodies after mRNA COVID-19 vaccines (Pfizer-BioNTech or Moderna), compared to over 90% in healthy people. That’s why the IDSA 2025 guidelines (Infectious Diseases Society of America) recommend two additional doses of the 2025-2026 COVID-19 vaccine for immunocompromised adults, not just one.
For influenza (flu), you still get one annual dose of the inactivated shot-no nasal spray. For hepatitis B (Engerix-B, Recombivax HB), you need the full three-dose series. And for pneumococcal disease (PCV20 or PPSV23), both vaccines are recommended, given at least one year apart.
Timing Is Everything
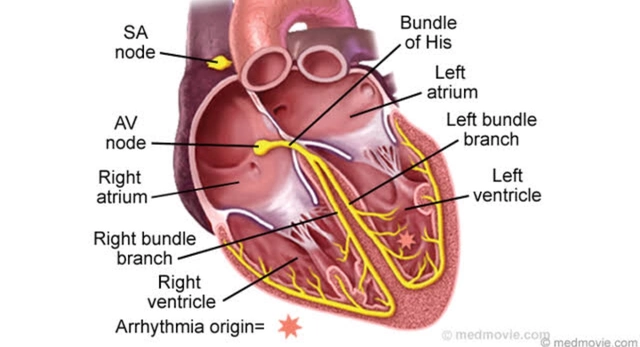
When you get the vaccine matters just as much as which one you get. The goal is to catch your immune system at its strongest point.If you’re on rituximab or ocrelizumab-B-cell depleting drugs-you need to wait at least six months after your last dose before getting any vaccine. The best window is 3 to 6 months after the last infusion, when your B-cells are starting to come back. If you’re still on regular infusions, schedule your vaccine about four weeks before your next one.
For people on cyclophosphamide, vaccines should be given during the "nadir week"-the week after your chemo cycle when your white blood cell count is recovering. For those on corticosteroids like prednisone, avoid vaccination if you’re taking 20 mg or more daily for two weeks or longer. Wait until the dose drops below 20 mg.
And if you’re starting immunosuppressants soon? Get all your vaccines at least 14 days before your first dose. That’s the window where your immune system still has enough strength to respond.
What About the COVID-19 Vaccine?
The mRNA COVID-19 vaccines (Pfizer and Moderna) are the gold standard for immunocompromised people. The Novavax (protein-based) vaccine is also an option if you can’t get mRNA. You need more doses than healthy people: two additional shots after your initial series, and possibly more depending on your condition.One patient with rheumatoid arthritis shared that skipping methotrexate for a week after each vaccine dose helped her develop detectable antibodies-something she hadn’t managed before. While this isn’t a universal recommendation, it shows that small adjustments can make a difference. Always talk to your doctor before changing your medication schedule.
Who Should Get Vaccinated?
The list is long: anyone with- Organ transplants (kidney, liver, heart, lung)
- Hematologic cancers (leukemia, lymphoma, multiple myeloma)
- Autoimmune diseases on biologics (rheumatoid arthritis, lupus, psoriasis)
- Chronic steroid use (≥20 mg prednisone daily for ≥14 days)
- Primary immunodeficiencies
- Recent stem cell transplants
Even if you’re not sure whether you’re immunocompromised, ask your doctor. The ICD-10 codes (Z94.0, D47.Z, L40.5) updated in January 2025 now help providers identify these patients automatically in electronic records.

Coordinated Care Saves Lives
The biggest problem isn’t the science-it’s the coordination. Too often, your rheumatologist, oncologist, and primary care doctor aren’t talking to each other. That’s why the University of Washington study found that patients with end-stage kidney disease who had structured vaccination scheduling had 42% fewer breakthrough COVID-19 infections.Specialized clinics like the Immunocompromised Vaccine Access Network (IVAN) now work directly with cancer centers to give vaccines during chemo breaks. Epic Systems’ January 2026 software update now flags immunocompromised patients in EHRs and auto-schedules vaccination reminders based on their medication history.
But you still need to be your own advocate. Keep a printed record of:
- Every immunosuppressant you take (name, dose, start date)
- When your last infusion was (especially for rituximab)
- Which vaccines you’ve had and when
Bring this to every appointment. Many pharmacies still run out of the updated COVID-19 vaccines, delaying protection during winter surges. Don’t wait for your doctor to call-ask for the vaccine at your next visit.
Protecting Your Circle
Your vaccine isn’t the only one that matters. The people around you need to be protected too. The IDSA 2025 guidelines stress that household members and close contacts should be fully vaccinated, including annual flu shots and updated COVID boosters. One study showed this "cocooning" strategy cut household transmission by 57%.That means your partner, kids, and caregivers need to be up to date-not just for their own safety, but to keep you safe. If someone in your home gets the flu or a cold, they should avoid close contact until they’re symptom-free.
What’s Next?
The field is moving fast. The CDC and IDSA are launching a national registry to track how well vaccines work in different immunocompromised groups. Researchers are testing new adjuvanted vaccines designed specifically for weak immune systems. In five years, point-of-care immune tests may tell your doctor exactly when your body is ready to respond to a vaccine.For now, the rules are clear: avoid live vaccines, get inactivated ones at the right time, and don’t assume your doctor knows your full history. Ask questions. Bring your meds list. Push for coordination. Your life depends on it.
Can I get the flu shot if I’m on prednisone?
Yes, but only if you’re taking less than 20 mg of prednisone (or equivalent) daily for 14 days or longer. If you’re on a higher dose, wait until your doctor reduces it. Always get the inactivated flu shot-not the nasal spray. Timing matters: aim for when your immune system isn’t at its lowest point, like between chemo cycles or after steroid tapering.
How long after rituximab can I get a vaccine?
Wait at least six months after your last rituximab infusion. The best time is 3 to 6 months after the last dose, when your B-cells are starting to recover. If you’re still getting regular infusions, schedule your vaccine about four weeks before your next one. Never get live vaccines after rituximab-this includes MMR, varicella, and the nasal flu vaccine.
Do I need more than one COVID-19 vaccine dose?
Yes. If you’re immunocompromised, you need two additional doses of the 2025-2026 mRNA COVID-19 vaccine after your initial series. Some people need more depending on their condition. The Novavax protein vaccine is also approved as an alternative. Don’t assume one dose is enough-your immune system may not respond fully without extra shots.
Can my family get live vaccines if I’m immunocompromised?
Yes. Household members can safely receive live vaccines like MMR and varicella. The risk of you catching the virus from them is extremely low. In fact, the CDC and IDSA recommend that everyone in your household be fully vaccinated-including live vaccines-to reduce your exposure. This "cocooning" strategy significantly lowers your risk of infection.
What if my pharmacy doesn’t have the right vaccine?
Call ahead. Many pharmacies run out of the updated COVID-19 vaccines, especially during flu season. If they don’t have it, ask for a referral to a specialty clinic, hospital pharmacy, or immunocompromised vaccine program like IVAN. Don’t delay-your protection window is narrow. Your doctor can help you find an alternative location with the right supply.


Let me just say this: if your doctor is still scheduling live vaccines for immunocompromised patients, they’re not just negligent-they’re endangering lives. I’ve seen it firsthand. LAIV in a rituximab patient? That’s not a mistake, that’s malpractice. The BC CDC guidelines are crystal clear, and yet hospitals are still using 2019 protocols. Someone needs to sue a hospital system for this. It’s not just about vaccines-it’s about systemic incompetence in immunology care.
wait so if u r on prednisone u cant get the flu shot? i thought u could? lol my doc said just dont get the spray one but i got the shot last year and felt fine? maybe im just lucky? idk maybe i shoulda asked more q’s
Look, I get the guidelines, but let’s be real-how many of these recommendations are based on underpowered studies with small n’s? The 15-85% antibody response range for mRNA vaccines in immunocompromised patients? That’s a wild spread. It’s not even a useful metric. And why are we assuming everyone responds the same way? Some people on low-dose methotrexate have robust responses. Others on steroids don’t respond even after extra doses. The one-size-fits-all approach is outdated. We need personalized immune profiling, not checklists. But nope, we’re still using flowcharts from 2018.
There’s a metaphysical layer here, you know? Vaccines aren’t just biological tools-they’re symbols of our collective fear of death, our desperate grasp at control over chaos. The fact that we’re debating whether a 20 mg prednisone dose disqualifies someone from a flu shot reveals our society’s pathological need to quantify everything, even the ineffable. We reduce life to dosages and windows, ignoring the soul’s resilience. Maybe the real vaccine isn’t the shot-it’s the courage to trust your body, even when the system says you’re broken.
bro i got my 4th covid shot last week and my rheum doc told me to skip methotrexate for 7 days after 😍 i felt like a science experiment but it worked!! antibodies up!! 🤓✨ also my dog got his rabies shot and now he’s my personal vaccine guardian 🐶💉 #immunocompromisedlife
This entire post is a waste of time. You’re overcomplicating it. If you’re immunosuppressed, you’re already a walking infection risk. Vaccines won’t save you. Stop pretending medicine can fix biology. Just stay home. Wear a mask. Don’t go anywhere. That’s the only real protocol. All this jargon? Just noise. You’re not special. You’re just sick.
For anyone reading this: keep a printed log. Every. Single. Dose. Every. Infusion. Every. Date. I’ve seen patients lose weeks of protection because they couldn’t recall when their last rituximab was. Don’t rely on memory. Don’t rely on your portal. Print it. Laminate it. Carry it. Your life is not a Google Doc. Your immune system doesn’t care about your EHR login. Be the advocate. Ask for IVAN. Ask for the specialty pharmacy. Don’t wait. Don’t hope. Act. Your life is worth the effort.
I’ve been on ocrelizumab for six years now. I’ve had three rounds of the 2025-2026 COVID vaccine, two flu shots, two pneumococcal vaccines, and a hepatitis B series-all timed to my infusions. But here’s the thing no one talks about: the emotional toll. Every time I schedule a vaccine, I feel like I’m begging my body to cooperate. It’s not just medical-it’s psychological. I cry before every shot. I don’t tell anyone. But I’m tired of being a statistic in a study. I want to know if my immune system remembers anything anymore. Or am I just a ghost in a medical algorithm?
Newsflash: the CDC doesn’t know what they’re doing. They’re just copying WHO. And WHO copied the EU. And the EU copied a 2012 paper from Japan. Nobody’s doing original research. And yet, we’re all supposed to follow this like it’s scripture? I’ve been on methotrexate for 12 years. I’ve had every vaccine they’ve thrown at me. I’m still alive. My antibody levels? Barely detectable. But I’ve never gotten sick. So maybe the whole ‘you need 4 doses’ thing is just corporate greed wrapped in medical jargon. Just sayin’.
My mom has lupus and takes mycophenolate. She got her flu shot last week and was so proud-she even took a selfie with the nurse. I told her to keep her meds list on her fridge. Now her whole family knows what to do. It’s not about being perfect. It’s about being prepared. And if your doctor doesn’t know the difference between PCV20 and PPSV23? Find a new one. You deserve better.
Oh wow. So we’re now in the era of ‘vaccine scheduling as a full-time job’? Next thing you know, we’ll need a permit to breathe in public. Let me get this straight: if you’re on immunosuppressants, you’re not just a patient-you’re a walking compliance checklist. ‘Don’t forget to wait 6 months after rituximab, but only if you’re not on steroids, unless your B-cell count is above 10, but only if you’re not in a rural area where the vaccine is out of stock, and your doctor hasn’t retired.’ This isn’t medicine. This is a Kafkaesque bureaucracy dressed in lab coats. And we’re supposed to be grateful?