Living with lupus is a bit like housing a particularly uninvited guest who likes to surprise you with new complaints. One of those might just be eye inflammation. But before you panic, let's unpack what's going on here and why it matters.
Lupus is a kind of autoimmune disorder, which basically means the body’s defense system gets a bit too enthusiastic and starts attacking its own tissues, eyes included. Believe it or not, about a third of people with lupus experience some form of eye trouble.
So, what's the big deal about eye inflammation? Well, your eyes aren't just for watching TV and spotting coffee shops. They're incredibly complex and sensitive. When inflammation strikes, they can start feeling like a desert, go blurry, or even develop some nasty pain.
Knowing the signs early on can make a world of difference. Keeping tabs on symptoms like redness, pain, or changes in vision can be crucial. It doesn't hurt to know the ropes so you can dodge more serious issues or catch them before they escalate.
- What is Eye Inflammation in Lupus?
- Common Symptoms to Watch For
- How Lupus Affects Vision
- Diagnosis and Testing
- Managing Eye Inflammation
- Tips for Healthy Eyes in Lupus Patients
What is Eye Inflammation in Lupus?
Now, let’s get down to what eye inflammation really means when you're dealing with lupus. In medical speak, this is called "ocular inflammation," but for most folks, it's simply trouble with your eyes feeling and working right. It's kinda common for folks with lupus to run into this, as lupus doesn’t exactly play favorites when it comes to the parts of your body it affects.
Lupus loves a surprise party across your body, and the eyes are no exception. Inflammation can pop up in different parts of your eyes, meaning you might deal with any number of issues. From the outer layer, known as scleritis, to the inner sections like uveitis, lupus can get at 'em all.
Common Types of Eye Inflammation in Lupus
There are a couple of frustrating ways that lupus shows up in your eyes:
- Dry Eye Syndrome: This is probably the most common. Your eyes just don't make as many tears as they should, leaving them feeling sandy and dry.
- Episcleritis and Scleritis: Redness and pain are the hallmarks here, as the inflammation takes root in the white area or even deeper.
- Retinal Vasculitis: Though rarer, this affects the retina, potentially impacting vision severely.
Why Does It Happen?
Figuring out why inflammation happens here isn't always straightforward. It boils down to your immune system doing its thing, not realizing that your eyes are friends, not foes. Because lupus is a systemic disease, these issues are systemic too, meaning they're all tied up with how the disease is playing out at a wider level.
If you’ve got lupus and start noticing eye issues, mark it down. Early action can keep things from spiraling into anything more severe. Eye inflammation isn't just a bother; it's a signal to stay ahead of your health game.
Common Symptoms to Watch For
When lupus decides to mess with your eyes, it's not exactly pulling punches. There are some telltale signs to keep an eye out for (pun intended), and catching them early can save you a ton of hassle.
Redness and Irritation
One of the first signs is redness in the eyes. They might feel itchy or just plain irritated. This is usually because the inflammation messes with the delicate tissues in your eye area.
Dry Eyes Galore
Imagine the Sahara in your eyeballs. Okay, maybe not that extreme, but dry eyes are a pretty common symptom. Your eyes might feel as if they're short on moisture, which can lead to discomfort and a scratchy feeling.
Blurry Vision
Things might start looking like you're in a watercolor painting. Blurriness is another symptom that sneaks up on you when eye inflammation gets going. It happens because swelling can mess with how your eyes focus.
Sensitive to Light
If you find yourself squinting at the slightest hint of brightness, light sensitivity might be the culprit. It's annoying and can make being outside, or even near a window indoors, a bit challenging.
Pain
Nobody likes dealing with pain, and when your eyes start to hurt, it's a signal. Eye pain, especially when you move them, is something you shouldn't ignore. It might feel like a sharp or dull ache.
| Symptom | Possible Cause |
|---|---|
| Redness | Swelling of eye tissues |
| Dry Eyes | Reduced tear production |
| Blurry Vision | Inflammation affecting focus |
| Light Sensitivity | Inflamed cornea |
| Pain | Swelling in eye orbits |
Keeping these symptoms in check means listening to your body. Don't brush off changes in your vision, especially if you're living with lupus. If anything feels off, it might be time to check in with your healthcare provider or eye doctor.
How Lupus Affects Vision
If you have lupus, your vision might take a hit because this condition doesn't stick to just one body part. It can create chaos pretty much anywhere, including your eyes. So, how exactly does lupus mess with your vision health? Let's dig in.
One common way is through inflammation of the eye itself, medically known as uveitis. This can cause pain, redness, blurred vision, and even sensitivity to light. And while it sounds intense, catching it early can save you a lot of discomfort.
Retinal Issues
Another area where lupus can cause trouble is with the retina – the light-sensitive layer at the back of your eye. Some folks with lupus might experience something called 'retinal vasculitis'. This might sound like a sci-fi monster, but it's actually just inflammation that can lead to vision problems.
"It's vital to recognize changes in vision as these can be indicators of a more serious issue," says Dr. Sarah Johnson, a renowned ophthalmologist.
Dry Eye Syndrome
Then, there's the not-so-fun experience of dealing with dry eyes. Because lupus can affect tear production, you might feel like you're staring into a wind tunnel even when you're indoors. Frequent blinking or using artificial tears can help manage this particular symptom.
Treatment Considerations
The treatments for lupus-related eye issues are as varied as the symptoms themselves. Some patients see improvement with anti-inflammatory meds, while others might need more specific treatments like immunosuppressants if their symptoms get pretty severe.
On the Bright Side: Prevention
Managing lupus often feels like a full-time job, but preventive care for your eyes can really pay off. Regular eye check-ups and staying in touch with your healthcare provider can keep complications at bay and ensure that any sneaky symptoms are caught early. It's all about being proactive, and honestly, your eyes deserve that TLC.
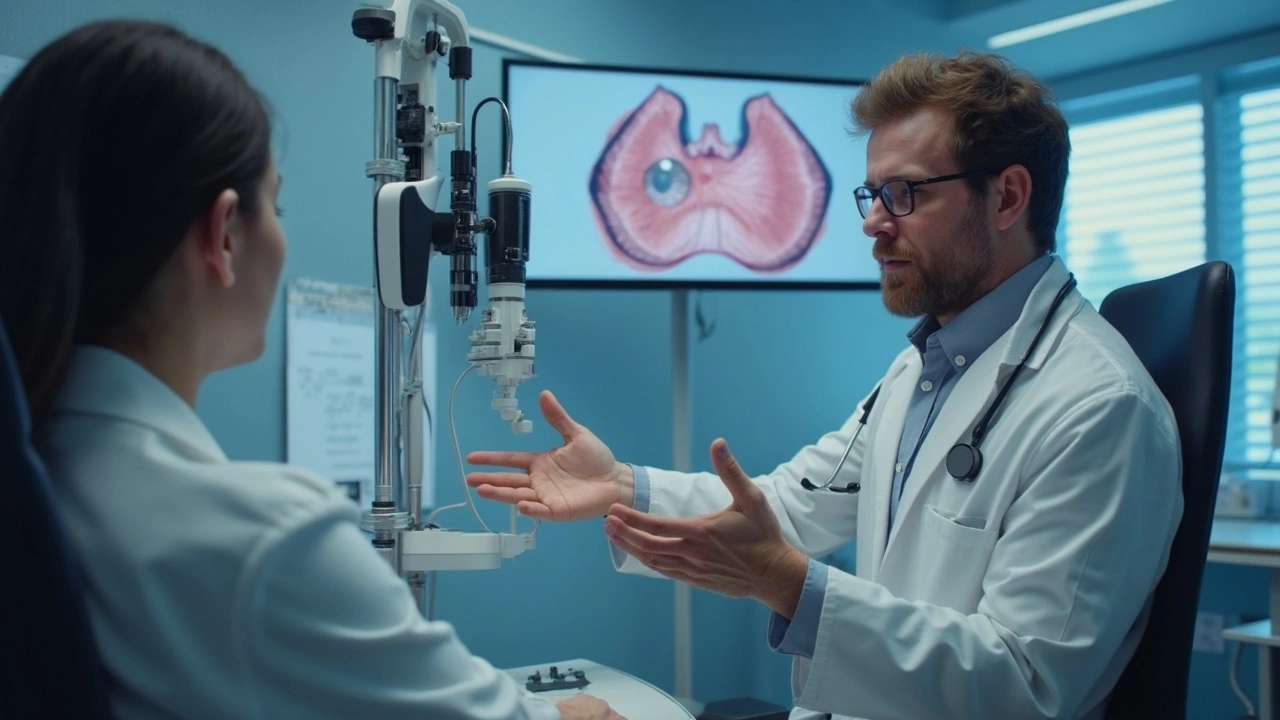
Diagnosis and Testing
When you've got lupus and start having eye inflammation symptoms, figuring out what's going on is crucial. You don't want to treat something blindly, right? So, here's the scoop on getting those peepers checked out.
Start with Your Regular Check-Up
Your regular doc might be the first port of call. They'll look at your symptoms and might refer you to an eye specialist to dig deeper. This could mean some tests to figure out exactly what's causing the trouble.
What to Expect at the Eye Doctor
At the eye specialist's office, they'll probably do a few different tests. Here are the usual suspects:
- Eye Exam: A thorough look at your eyes to check for redness, swelling, or other visible signs of eye inflammation.
- Visual Acuity Test: Basically, a fancy way to see if your vision has gone all wonky. Reading those pesky eye charts and more.
- Slit-lamp Examination: This lets the doc see the different parts of your eye in detail, looking for issues like uveitis or retinal damage.
Dr. Elaine Fitch, an ophthalmologist, says, "It’s vital to assess any changes in vision or eye discomfort, especially in patients with autoimmune disorders like lupus."
Special Tests for Lupus-Related Eye Issues
Beyond the basic tests, you might need specialized evaluations:
- OCT (Optical Coherence Tomography): Think of it as an MRI for the eye. It gives a detailed picture of your retina and can pinpoint any swelling or damage.
- Fluorescein Angiography: This test involves injecting a dye to check the blood flow in the retina. It’s useful if there's a suspicion of blood vessels causing problems.
These tests can not only diagnose but help in tailoring the treatment plan to manage the issue effectively and keep your eyes as healthy as possible while living with lupus.
Managing Eye Inflammation
Dealing with eye inflammation when you have lupus can be a bit of a juggling act, but it's definitely manageable with the right approach. From tweaks in your daily routine to working closely with your doc, let's break down some practical ways to take care of your peepers.
Daily Habits to Support Eye Health
First off, staying hydrated is key. Drinking plenty of water helps keep your eyes from feeling like they've been stranded in the Sahara. Also, take regular breaks from screens. The 20-20-20 rule is a nifty trick: every 20 minutes, look at something 20 feet away for, you guessed it, 20 seconds.
If your eyes feel dry or itchy, over-the-counter artificial tears can offer some relief. Just make sure you’re picking preservative-free options to keep any additional irritation at bay.
Medical Treatments
Sometimes, home care isn’t enough, and you might need a bit more muscle from your healthcare team. Anti-inflammatory eye drops, like corticosteroids, are often prescribed to help quell the inflammation and ease discomfort. However, these come with their baggage, as long-term use can cause side effects. It’s super important to follow your doc's instructions and report any changes in symptoms.
Nutrition and Lifestyle
Don’t underestimate the power of what's on your plate. A diet rich in omega-3 fatty acids—think fatty fish like salmon or a daily flaxseed smoothie—can do wonders. It’s also wise to incorporate foods packed with vitamin C and E, like citrus fruits and nuts—they're known to support overall vision health.
Regular Check-ups
Finally, regular visits to the eye doctor should be penciled into your calendar. They can track any changes and help catch issues early, keeping your vision on point. During these visits, you might undergo tests like OCTs (optical coherence tomography) to get a detailed view of your eye’s health.
In summary, keeping a close eye on your lifestyle, teaming up with medical experts, and being proactive about your health are crucial steps to tackle the effects of lupus on your eyes. Remember, staying informed and vigilant can help you see the world a bit clearer.
Tips for Healthy Eyes in Lupus Patients
Keeping your eyes healthy when you’re dealing with lupus isn't just about fixing problems; it’s also about preventing them. This can be a bit like trying to keep a cat in a dress—tricky but definitely doable with the right approach.
Regular Check-Ups are Key
The number one rule is regular check-ups. Get your eyes checked by an ophthalmologist at least once a year. The earlier issues are caught, the easier they are to deal with.
Moisturize, Moisturize, Moisturize!
Dry eyes are a common complaint. Keep your eyes hydrated with over-the-counter artificial tears. They’re a quick fix to relieve uncomfortable dryness. Just remember, this doesn't replace medical advice if things are more severe.
Protect from the Sun
Whenever you step outside, think of sunglasses as your best friends. UV rays can make eye inflammation worse. Grab a pair with UV protection, and you’re good to go.
Stay Away from Smoke
Avoiding smoke is a savvy move. Smoking or even just being around smoke can worsen eye issues. Plus, it’s not great for your overall health either.
Keep It Clean
Makeup may make you look and feel great, but keeping it around too long? Not so much. Take it off before bed and make sure all your products are hypoallergenic.
Eat for Eye Health
Nourishing your body with a calcium-rich diet can be beneficial, according to studies. Foods high in omega-3s like salmon or flaxseeds can support vision health, which is especially important for those with eye inflammation risks.
Quick Tips at a Glance
- Annual eye exam
- Use artificial tears
- Wear UV-blocking sunglasses
- Avoid smoking and smoky areas
- Remove makeup daily
- Include omega-3s in your diet
Remember, managing lupus and eye inflammation together is a balancing act. But with these basic steps, you’re much more likely to keep seeing clearly on this adventure.




Ever wonder why the mainstream medical community barely mentions eye inflammation in lupus? It's because they don't want you to see the hidden agenda, the pharma giants that profit from your suffering. The truth is, they've been suppressing low‑cost anti‑inflammatory eye drops for decades. Meanwhile, patients are left juggling steroids that bring a laundry list of side effects. Think about the pattern: every time a natural remedy pops up, the headlines go silent. This isn't coincidence, it's a coordinated effort to keep you dependent. If you start questioning the narrative, you might find a whole underground network of researchers willing to share real solutions. Stay vigilant, the eyes may be the windows, but also the mirrors reflecting the conspiracy.
The relationship between systemic lupus erythematosus and ocular pathology is well documented; however, many patients remain unaware of the early warning signs. Redness, photophobia, and episodic blurry vision should prompt immediate ophthalmologic evaluation, not mere observation. While artificial tears provide symptomatic relief, they do not address the underlying immunologic mechanisms. Therefore, regular slit‑lamp examinations are indispensable for monitoring disease progression. Moreover, adhering to prescribed immunosuppressive therapy can mitigate severe complications, including retinal vasculitis. In sum, proactive care supersedes reactive treatment; neglect is the greatest risk.
Yo, if you got lupus and your eyes feel like sandpaper, don't wait till it hurts like hell. Grab some preservative‑free drops and hit up your rheum doc quick. Those steroids can be a real pain in the butt if you use 'em wrong. Also, try the 20‑20‑20 rule-look 20 feet away for 20 seconds every 20 minutes. Trust me, staying off the screens for a bit helps a lot. Keep your head up and your eyes moister!
From a neuro‑immunological perspective, ocular involvement in systemic lupus erythematosus can be conceptualized as a breach of the blood‑retinal barrier, precipitating a cascade of inflammatory mediators. This etiological framework underscores the importance of cytokine profiling in both serum and aqueous humor to tailor biologic therapy. In practice, integrating tear film osmolarity measurements can augment traditional slit‑lamp findings, offering a quantitative biomarker for disease activity. As mentors, we should empower patients with actionable data, facilitating shared decision‑making. Remember, interdisciplinary collaboration-rheumatology, ophthalmology, and immunology-optimizes outcomes. Let us champion evidence‑based protocols while acknowledging individual variability in disease phenotypes.
Our nation has always prided itself on pioneering medical breakthroughs, yet we allow foreign pharmaceutical lobbies to dictate patient care for lupus eye disease. It is an affront to our sovereignty when vital research is outsourced and the profits flow overseas while our citizens suffer. We must demand home‑grown solutions, fund domestic labs, and support veteran researchers who understand our unique genetic makeup. The American spirit thrives on resilience; let us apply that same fire to combat ocular inflammation. No more waiting for imported drugs that come with hidden strings. Rise up, protect our health, and reclaim our medical independence.
It's essential to recognize the value of both domestic innovation and global collaboration; progress often stems from shared knowledge across borders. While advocating for local research, we can also encourage transparent partnerships that prioritize patient welfare above profit.
In accordance with established clinical guidelines, it is advisable for individuals with systemic lupus erythematosus to undergo comprehensive ophthalmologic assessments at least annually. Such examinations should encompass visual acuity testing, intraocular pressure measurement, and detailed slit‑lamp evaluation. Early detection of ocular inflammation can markedly reduce the risk of irreversible visual impairment. Patients are encouraged to adhere strictly to prescribed therapeutic regimens and report any new ocular symptoms promptly. Maintaining meticulous medical records will facilitate optimal longitudinal care.
Hey folks, here’s a quick cheat‑sheet for managing lupus‑related eye issues: 1️⃣ Keep a water bottle handy-hydration keeps your tear film happy. 2️⃣ Use preservative‑free artificial tears at least three times a day, especially after screen time. 3️⃣ The 20‑20‑20 rule isn’t just a meme; it really does give your eyes a break. 4️⃣ Schedule an eye exam every six months if you’ve had any inflammation episodes-early catches save vision. 5️⃣ Talk to your rheumatologist about adding hydroxychloroquine if you’re not already on it; it can help control systemic activity. 6️⃣ Finally, wear UV‑blocking sunglasses outdoors; they protect against light‑induced flare‑ups. Stay proactive and you’ll keep those windows to the world clear!
Totally agree, the 20‑20‑20 rule saved my eyes during marathon coding sessions.
Great roundup, thanks for the concise guide!
Don't let lupus dictate your vision-take charge, follow the eye‑care plan, and remember every small step adds up to big improvements in quality of life.
When we examine the interplay between autoimmunity and ocular health, we encounter a microcosm of the body's broader struggle for homeostasis. The eye, with its immune‑privileged status, serves as a unique laboratory for studying inflammatory cascades. Recognizing patterns of cytokine expression in uveitis can illuminate pathways applicable to other organ systems. Moreover, patient narratives reveal the psychological burden of fluctuating vision, underscoring the need for holistic care. As we advance therapeutics, integrating patient‑centered outcomes will ensure that scientific gains translate into lived improvements. Let us continue to bridge bench research with bedside empathy, fostering a comprehensive approach to lupus eye disease.
It is tempting to adopt a deterministic view of lupus‑related ocular complications, assuming they are inevitable and unmodifiable. However, such a fatalistic stance neglects the substantial body of evidence demonstrating the efficacy of early intervention. Numerous cohort studies have shown that patients who undergo routine slit‑lamp examinations within six months of diagnosis experience markedly lower rates of retinal vasculitis. In contrast, delayed assessment often correlates with irreversible retinal scarring and permanent visual field loss. Moreover, the pathophysiological mechanisms underlying scleritis are increasingly elucidated, revealing targetable interleukin‑6 pathways. Biologic agents that inhibit these cytokines have yielded promising outcomes in randomized trials, reducing both pain and tissue destruction. Yet, skeptics argue that the high cost of these therapies renders them inaccessible to the average patient. While cost remains a legitimate concern, insurance frameworks in many regions have adapted to accommodate biologic coverage for severe autoimmune manifestations. Ignoring these developments in the name of budgetary caution is, in effect, an ethical oversimplification. Additionally, lifestyle modifications-including omega‑3 supplementation, smoking cessation, and meticulous UV protection-contribute additive benefits that cannot be dismissed as mere ancillary measures. The convergence of pharmacologic precision and patient‑driven self‑care forms a synergistic paradigm that challenges the notion of therapeutic futility. Critics who perpetuate the narrative of hopelessness inadvertently undermine patient morale, which is itself a critical component of disease management. Clinical guidelines now explicitly endorse a multidisciplinary approach, integrating rheumatology, ophthalmology, and nutrition expertise. The literature unequivocally supports this model, citing improved visual acuity scores and reduced flare frequency. Therefore, to claim that lupus‑induced eye inflammation is an untreatable destiny is a misrepresentation of contemporary medical consensus. Embracing proactive, evidence‑based strategies offers a realistic pathway to preserve vision and enhance overall quality of life.
While I concur with the emphasis on multidisciplinary care, it is also vital to address socioeconomic barriers that impede access to advanced therapies; initiatives such as patient assistance programs and sliding‑scale clinics can bridge this gap 🌟. By fostering equitable resource distribution, we ensure that the therapeutic advancements you described reach those most in need.
Oh sure, because the next step is obviously to replace our doctors with conspiracy‑theorist influencers who claim eye drops are a government mind‑control tool 🙄.