QT Prolongation Risk Calculator
Assess Your Risk
This tool helps you understand your personal risk of QT prolongation based on your medications, health conditions, and other factors.
Click to select your medications. Add more by searching at AZCERT.org
Risk Assessment
Every year, hundreds of people die suddenly from a heartbeat that just stops - no warning, no pain, often while they’re doing something ordinary. For many, the trigger wasn’t a heart attack or a genetic flaw. It was a medication they were told was safe. The hidden culprit? QT prolongation.
QT prolongation isn’t a disease you feel. You won’t know you have it unless your ECG is checked. But when it goes too far, it can set off a deadly heart rhythm called Torsades de Pointes - a twisting, chaotic beat that can turn into sudden cardiac death. It’s not rare. Over 100 common drugs can cause it. And the risk isn’t the same for everyone.
What QT Prolongation Actually Means
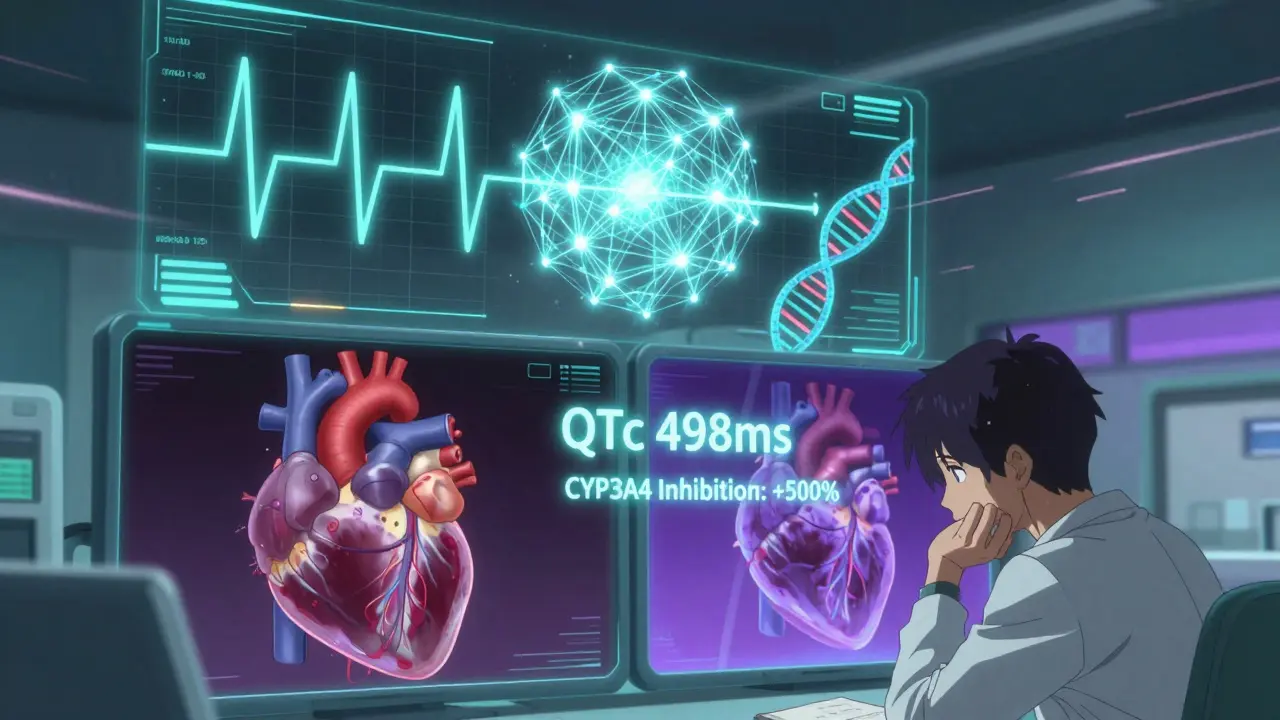
The QT interval on an ECG measures how long it takes your heart’s lower chambers to recharge after each beat. If that time stretches too long - beyond 450 milliseconds in men or 470 in women - your heart becomes vulnerable to dangerous rhythms. A QTc over 500 ms, or a jump of more than 60 ms from your baseline, is a red flag. But here’s the twist: the length of the QT interval alone doesn’t tell the whole story. Research from the ARIC study found that the shape of the T-wave - specifically how long it takes to reach its peak - is an even stronger predictor of death. Each standard deviation increase in T-wave duration raised the risk of sudden cardiac death by 21%.
Measuring QT isn’t simple. Automated machines can be off by up to 40 milliseconds. Manual readings vary between doctors. And standard ECGs can’t see the spatial spread of electrical recovery across the heart - a key factor in triggering arrhythmias. That’s why some people with borderline QTc values still go into cardiac arrest, while others with longer intervals never do.
Medications That Carry the Highest Risk
Not all QT-prolonging drugs are equal. Some are far more dangerous than others.
- Class III antiarrhythmics like dofetilide and sotalol are the most dangerous. Dofetilide alone causes Torsades in 3.3% of patients at standard doses.
- Antibiotics vary wildly. Moxifloxacin can stretch QTc by 6-15 ms. Ciprofloxacin? Barely 0-5 ms. Erythromycin, especially when taken with drugs that block its metabolism (like azole antifungals or grapefruit juice), can double your risk of sudden death - and quintuple it if you’re on a CYP3A4 inhibitor.
- Antidepressants show a clear split: citalopram at 40 mg daily increases QTc by 8.5 ms on average. Escitalopram, at the same dose, only adds 4.2 ms. That’s not a small difference - it’s the difference between a caution sign and a stop sign.
- Antipsychotics like haloperidol and ziprasidone are high-risk. Even at therapeutic levels, they can push QTc into dangerous territory.
The problem isn’t just the drug itself. It’s how it interacts. Many drugs are metabolized by the liver enzyme CYP3A4. When you take two drugs that block this enzyme - say, an antibiotic and an antifungal - the concentration of the QT-prolonging drug skyrockets. That’s why one study found the risk of sudden death jumped five-fold when erythromycin was combined with a CYP3A4 inhibitor.
Who’s Most at Risk?
If you’re healthy, young, and taking one low-risk drug, your chance of dying from QT prolongation is tiny. But add just a few risk factors, and everything changes.
- Women are more sensitive. Their baseline QTc is naturally longer. A QTc of 470 ms is normal for women but dangerous for men.
- Older adults take an average of 7.8 medications. Over a third of people over 65 are on at least one QT-prolonging drug. Polypharmacy isn’t just inconvenient - it’s deadly in this context.
- People with heart disease are 10 to 100 times more vulnerable. A structurally normal heart can handle a mild QT prolongation. A damaged heart? Not so much.
- Low potassium or magnesium is a silent amplifier. Correcting hypokalemia (keeping potassium above 4.0 mEq/L) cuts QT-related risk by 62%. Simple blood tests can prevent tragedy.
- Genetic factors play a role. Some people have inherited mutations in ion channels that make them hypersensitive - even to low doses. The NIH’s All of Us program is now collecting genomic data from 1 million people to identify these variants.
And here’s the cruel irony: most people who die from drug-induced QT prolongation don’t have arrhythmias at autopsy. The POST SCD study found 78% of these deaths had no electrical cause. Instead, they were due to heart failure, stroke, or infection. That means the drug didn’t directly trigger the arrhythmia - it made an already unstable system collapse.
What Clinicians Are Doing About It
Some hospitals are getting smarter. Mayo Clinic rolled out an automated ECG alert system in 2015 that flags high-risk QTc values and blocks prescriptions of dangerous drugs unless overridden. The result? A 37% drop in dangerous prescriptions.
The FDA and NIH launched the CiPA initiative in 2013 to replace outdated tests with better ones. Instead of just checking hERG channel blocking (which isn’t always predictive), CiPA looks at how a drug affects multiple ion channels and simulates its effect on a virtual heart. It’s more accurate. And 92% of big pharma now use it.
But the real problem is in primary care. A 2022 JAMIA study found that 78% of QTc alerts in hospitals were false alarms. Doctors get so used to ignoring them that they stop paying attention. One clinician on the American College of Cardiology forum said they’re now ordering unnecessary ECGs just to check for ondansetron - a drug with very low risk - because they’re afraid of liability. That’s not safety. That’s burnout.
What You Can Do
If you’re on any of these medications, don’t panic. But do ask these questions:
- Have I had an ECG in the last year? If not, ask for one - especially if you’re over 65 or on multiple meds.
- Am I taking any drugs that could interact? Check for antibiotics, antifungals, or SSRIs. Use the AZCERT.org database - it’s free, updated weekly, and ranks drugs by risk.
- Have my electrolytes been checked? Potassium and magnesium are cheap, easy tests. Ask your doctor to include them in your next blood panel.
- Am I on the lowest effective dose? For citalopram, 20 mg is safer than 40 mg. For many drugs, less is better.
- Do I have heart disease, kidney disease, or a history of fainting? If yes, your risk is higher. Talk to a cardiologist before starting any new medication.
And if you’re prescribed a new drug with a QT warning - don’t refuse it. Ask: Is this the best option? Is there a safer alternative? Are my risks being managed? Many life-saving drugs - like certain antidepressants or antipsychotics - can still be used safely if monitored.
The Bigger Picture
Overemphasis on QT prolongation has backfired. The European Heart Rhythm Association warns that 15-20% of heart failure patients have had their medications stopped unnecessarily because of a borderline QTc - and many of them died from their original condition. QT prolongation isn’t a standalone danger. It’s a risk multiplier. It needs context.
The future is in AI. The FDA approved QTguard by Verily in 2023 - an AI system that cuts false alarms by 53% by analyzing ECG waveforms, not just numbers. New guidelines now require regulators to look at T-wave shape, not just QTc length. And by 2026, the All of Us program may give us personalized risk scores based on your DNA.
For now, the best defense is awareness. Know your meds. Know your numbers. Know your risks. And don’t let fear stop you from getting the care you need - just make sure it’s the right care, at the right dose, with the right checks in place.
Can a single medication cause sudden cardiac death from QT prolongation?
Yes, but it’s rare in healthy people. High-risk drugs like dofetilide or moxifloxacin can trigger Torsades de Pointes on their own, especially at high doses or in people with existing risk factors like low potassium, heart disease, or female sex. Most cases involve a combination of drugs or underlying conditions.
Is QT prolongation reversible?
Yes, in most cases. Stopping the offending drug, correcting electrolyte imbalances (especially potassium and magnesium), and treating underlying conditions like bradycardia can normalize the QT interval within days. But if a dangerous rhythm like Torsades has already occurred, immediate medical intervention - like magnesium sulfate or pacing - is required.
Do I need an ECG before taking any new medication?
Not for every drug. But if you’re over 65, on multiple medications, have heart disease, or are starting a drug known to prolong QT (like citalopram, erythromycin, or ziprasidone), an ECG before starting is strongly recommended. It’s a simple, low-cost check that can prevent death.
Are over-the-counter drugs safe for QT prolongation?
Some aren’t. Certain antihistamines (like diphenhydramine in Benadryl) and cough syrups with pseudoephedrine can prolong QT, especially in high doses or when combined with other drugs. Herbal supplements like St. John’s Wort can also interfere with drug metabolism. Always check with your pharmacist if you’re on a QT-prolonging prescription.
How do I check if my medication is on the high-risk list?
Use the AZCERT.org database - it’s free and updated weekly. Search your medication by name and it will show you the risk level: Known Risk, Possible Risk, or Conditional Risk. Your doctor or pharmacist can also access this tool. It’s the most reliable public resource available.
Next Steps: What to Do Now
If you’re on a medication with a QT warning:
- Don’t stop it without talking to your doctor - sudden withdrawal can be dangerous.
- Ask for a recent ECG if you haven’t had one in the last 12 months.
- Request a basic blood panel: potassium, magnesium, and kidney function.
- Review all your medications with your pharmacist - including supplements and OTC drugs.
- If you’ve ever fainted, had palpitations, or had a family history of sudden death before age 50, tell your doctor. That’s critical information.
If you’re a caregiver for an elderly relative:
- Keep a list of every medication they take - even vitamins.
- Check for interactions using AZCERT.org or ask a pharmacist.
- Watch for dizziness, fainting, or irregular heartbeat - these are early warning signs.
- Push for a simple ECG if they’re on more than three medications.
QT prolongation isn’t a myth. It’s a measurable, preventable risk. And with the right questions and checks, it doesn’t have to be deadly.