Stopping your medication because of side effects is one of the most common mistakes people make - and it’s often unnecessary. You’re not alone. About half of all patients quit their prescriptions early because of unpleasant symptoms. But many of those side effects aren’t dangerous, don’t last long, and can be managed - without ditching the treatment. The key isn’t enduring discomfort. It’s knowing how to talk to your doctor so they can help you stay on track.
Most Side Effects Fade With Time
It’s normal to feel off when you start a new medication. Nausea, dizziness, fatigue, dry mouth - these aren’t signs the drug is broken. They’re signs your body is adjusting. Research shows that 68% of common side effects go away within 7 to 14 days. That’s not a guess. It’s based on data from the British Heart Foundation and tracked across thousands of patients. If you quit too soon, you might miss out on the real benefits - like lower blood pressure, better mood, or reduced inflammation - that only show up after your system settles in.
Think of it like starting a new workout. Your muscles ache at first. That doesn’t mean you should stop exercising. It means you need to adjust, recover, and keep going. Same with medication. Your body is learning how to process it. Give it a couple of weeks before deciding it’s not working for you.
Track Your Symptoms Like a Pro
Going to your doctor and saying, “I feel weird,” doesn’t help. They need specifics. The best way to make your concerns heard? Keep a simple side effect diary. Write down:
- When the symptom happened (time of day, after which dose)
- How bad it was (rate it 1 to 10)
- What you were doing when it hit (eating, walking, lying down)
- How it affected your day (could you work? Sleep? Drive?)
Patients who use this method cut their chances of quitting medication by 23%, according to a 2021 study in the Journal of the American Medical Informatics Association. Why? Because numbers tell a clearer story than feelings. If you say, “I’ve had dizziness three times this week, mostly after my morning pill, and it’s a 7/10,” your doctor can immediately consider switching your timing, lowering your dose, or checking for interactions.
Apps like Medisafe or MyTherapy make this easy. But even a notebook and pen works. The goal isn’t perfection - it’s clarity.
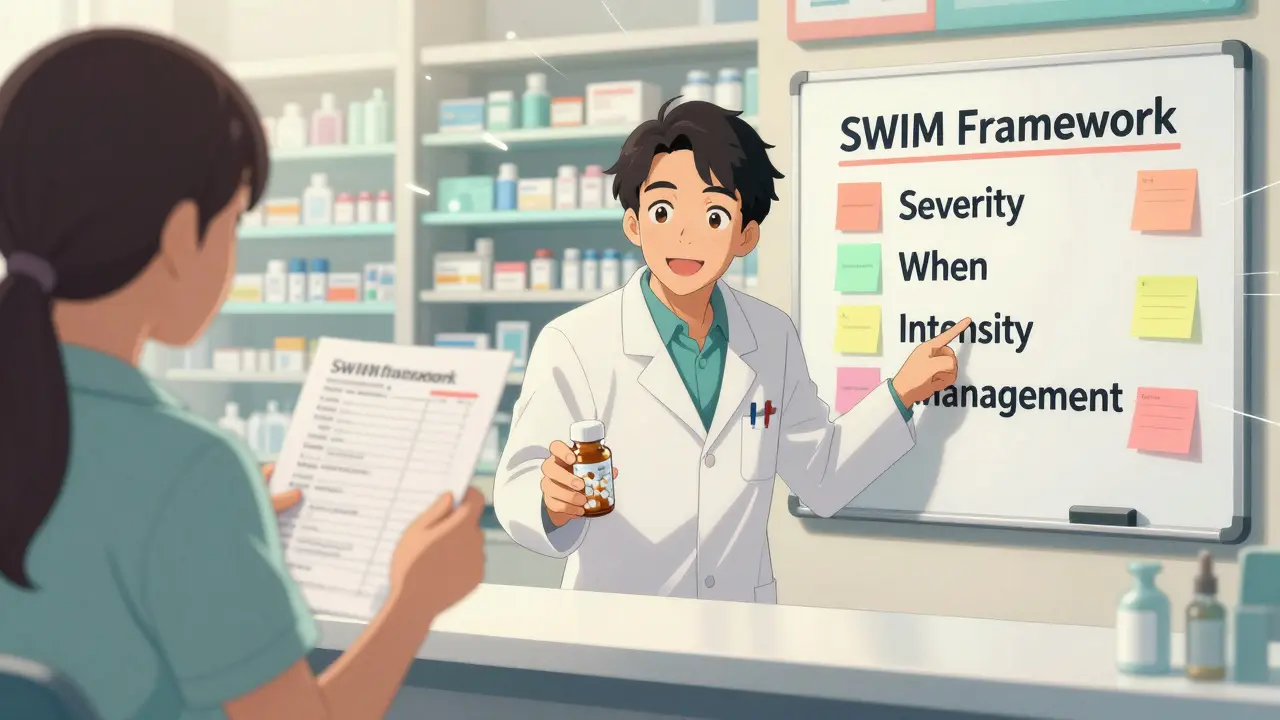
Use the SWIM Framework to Ask Better Questions
Don’t just say, “This side effect sucks.” Use a simple structure called SWIM to guide your conversation:
- Severity - How bad is it? (1-10)
- When - When does it happen? (Right after taking it? Only at night?)
- Intensity - Is it getting worse, better, or staying the same?
- Management - What have you tried? (Did eating food help? Did lying down reduce it?)
This isn’t just for doctors. Pharmacists are trained to help too. If you’re unsure, ask your pharmacist before your next appointment. They can often suggest quick fixes - like taking the pill with a small snack to reduce nausea, or switching from morning to bedtime dosing to avoid daytime drowsiness.
A real case from GoodRx: A patient on blood pressure meds had severe nausea every morning. Instead of quitting, she asked her pharmacist: “What if I take it with a cracker?” The change cut her nausea from 5-6 times a day to 1-2 times a week. She stayed on the medication. Her blood pressure improved. She didn’t need a new drug.
Side Effects Can Be a Sign It’s Working
This might sound strange, but hear it out. Some side effects aren’t bugs - they’re features. A 2021 study published in PMC showed that when patients were told, “This mild headache or fatigue is a sign the medicine is doing its job,” their anxiety dropped by 37%, and they were 29% less likely to quit. It’s not about ignoring discomfort. It’s about reframing it.
For example, if you’re on an antidepressant and feel more anxious at first, that’s not a reason to stop. It’s a common early response as your brain chemistry adjusts. If you’re on a statin and get mild muscle soreness, it doesn’t mean you’re damaged - it could mean the drug is actively lowering your cholesterol. Your doctor can test for real risks (like elevated CK levels) - but only if you tell them.
Never assume a side effect means the drug is harmful. Ask: “Is this normal? Is it temporary? Is there a way to make it easier?”
Don’t Guess. Don’t Adjust. Don’t Quit Alone
Some people lower their dose because they think “less is safer.” Others skip doses to avoid side effects. Both are dangerous. Antibiotics, for example, need full courses to kill all the bad bacteria. Stopping early can lead to resistant infections. Blood thinners, seizure meds, and heart medications can cause serious harm if stopped abruptly.
Never change your schedule without talking to your provider. But you can ask: “Can we try taking this at night instead of morning?” or “Could we lower the dose for a week and see how I feel?” Most doctors will say yes - if you come prepared with your symptom diary and clear questions.
A 2022 survey from HealthUnlocked found that patients who asked about timing changes were 4.2 times more likely to stick with their medication. That’s not luck. It’s communication.
Prepare Before Your Appointment
Don’t walk in blind. Before your visit, make a list:
- All your medications (including supplements and OTC drugs)
- When you take each one
- Any side effects you’ve tracked
- One or two things you’d like to change
GoodRx found that patients who brought a full medication list reduced the risk of dangerous interactions by 32%. It also shows your doctor you’re serious about staying on track. Bring your symptom diary. Print it out. Email it ahead of time. The more detail you give, the more they can help.
What If It’s Really Bad?
Not all side effects are mild. If you experience:
- Swelling of the face, lips, or throat
- Severe rash or blistering
- Chest pain or irregular heartbeat
- Sudden confusion or difficulty speaking
- Signs of liver damage (yellow skin, dark urine, severe nausea)
Call your doctor immediately or go to urgent care. These aren’t normal adjustments. They’re red flags. But if it’s fatigue, dry mouth, mild nausea, or occasional dizziness - those are usually fixable.
Doctors Want You to Stay on Your Meds
Many patients assume their doctor will just say, “Stop it.” But that’s not what most providers want. The American Medical Association’s 2021 guidelines say doctors should frame side effects as “manageable,” not “deal-breakers.” They’re trained to help you stay on treatment. That’s why Kaiser Permanente’s pharmacist-led side effect program cut medication discontinuation by 22% in just one year.
Your doctor isn’t trying to force you to suffer. They’re trying to keep you healthy. But they can’t do that if you don’t tell them what’s going on. Silence leads to quitting. Communication leads to solutions.
You’re Not Alone - And You Don’t Have to Quit
Thousands of people have been where you are. One Reddit user, u/MedPatient92, shared how showing their doctor a spreadsheet of dizziness episodes led to a simple dosing schedule change - no drug switch needed. Another patient in Sydney swapped their morning statin to bedtime and stopped waking up with muscle aches. Neither quit. Both stayed healthy.
Medication isn’t a one-size-fits-all fix. It’s a tool. And like any tool, it needs fine-tuning. The goal isn’t to feel perfect right away. It’s to feel better over time - without losing the benefits of your treatment.
You don’t have to choose between side effects and healing. You just need to know how to ask the right questions - and give your body (and your doctor) a chance to help you get there.
What if my side effects don’t go away after two weeks?
If side effects persist beyond 14 days, it’s time to revisit your treatment plan. Bring your symptom diary to your doctor and ask: ‘Can we adjust the dose, switch to a similar medication, or add something to help manage this?’ Many side effects can be resolved without stopping the original drug - like adding an anti-nausea pill for stomach issues or changing the time you take it. Don’t wait until it gets worse.
Can I just stop taking my medication if I don’t like the side effects?
No - not without talking to your doctor first. Stopping certain medications suddenly can cause serious problems. Blood pressure meds can cause rebound spikes. Antidepressants can trigger withdrawal symptoms. Seizure drugs can trigger seizures. Even if you think the side effects are worse than the condition, quitting cold turkey is riskier than working with your provider to find a better solution.
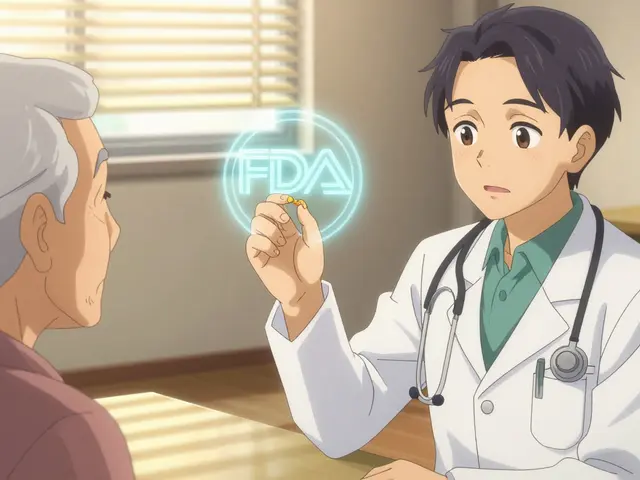
Should I look up side effects online before my appointment?
Yes - but stick to trusted sources like the FDA’s medication guides, Mayo Clinic, or the NHS website. Avoid forums or anecdotal stories. Many side effects listed are rare. Your doctor can tell you what’s common vs. unusual for your specific case. Knowing what’s normal helps you ask better questions and avoid panic.
Is it okay to ask my pharmacist instead of my doctor?
Absolutely. Pharmacists are medication experts trained to help with side effects. They can tell you if a symptom is typical, suggest food or timing changes, check for interactions, and even call your doctor to suggest a dose adjustment. Many pharmacies offer free medication reviews - use them. You don’t need a doctor’s appointment to get help.
What if my doctor says ‘just deal with it’?
If your doctor dismisses your concerns, it’s time to find someone who listens. You have the right to care that respects your experience. Ask for a referral to a specialist or a different provider. Medication adherence is a partnership. If your provider isn’t willing to work with you, you deserve better. There are doctors who specialize in medication management - especially for chronic conditions like hypertension, depression, or diabetes.



Okay so I started this new antidepressant and holy hell the first week was like my brain was being rewired by a drunk electrician. Dizziness, nausea, crying at commercials for laundry detergent-like, why did I even watch that ad? But I kept a little notebook like the post said, wrote down every time I felt like I wanted to throw my phone out the window. Turned out it was always right after breakfast. So I switched to taking it at night. Now I just wake up feeling like a human again. No drug change. No panic. Just a tiny tweak. If you’re suffering, don’t quit-just track it. Your brain isn’t broken, it’s just learning.
You people are so naive. This whole ‘just track your symptoms’ thing is just pharmaceutical propaganda dressed up as self-help. The system doesn’t want you to question meds-it wants you compliant. Side effects exist for a reason: your body is rejecting a foreign chemical. Why not ask why you need the drug in the first place? Maybe the real solution isn’t dosing schedules-it’s diet, sleep, therapy. But no, let’s just keep popping pills and calling it ‘management.’
There’s a deeper philosophical layer here that most miss. We treat medication like a tool, but it’s actually a negotiation between biology and control. The side effects aren’t noise-they’re feedback. The body is screaming, ‘I don’t recognize this molecule.’ But instead of listening, we quantify it, chart it, and call it ‘data.’ We’ve outsourced our intuition to spreadsheets. Is tracking symptoms empowering-or are we just becoming better at tolerating things we should question? Maybe the real victory isn’t staying on the drug… but rethinking why we’re on it at all.
Oh wow. A 23% reduction in quitting because you wrote down how you felt? How revolutionary. Next they’ll tell us that journaling your existential dread reduces your need for therapy. Let me guess-the study was funded by a pharma company that sells the app you’re supposed to use? I’m not impressed. People quit meds because they’re tired of being told their suffering is ‘normal.’ And now we’re supposed to be grateful for a checklist? What a joke.
THIS. THIS RIGHT HERE. I was ready to quit my anxiety med after three days-I thought I was dying. But I started the SWIM method and guess what? The dizziness only happened after coffee. I switched to taking it after lunch. No more panic attacks. No new prescription. Just better timing. And my doctor was so impressed she gave me a handwritten note saying ‘You’re doing it right.’ You are NOT weak for feeling side effects. You’re STRONG for speaking up. Keep going. You got this. I’m rooting for you.
Let’s address the elephant in the room: the entire premise assumes that taking psychiatric or cardiovascular medication is inherently beneficial. What if the condition itself is overdiagnosed? What if the ‘benefits’ are statistically marginal but marketed as life-saving? You’re not just managing side effects-you’re reinforcing a medical-industrial complex that profits from chronic dependence. The real solution isn’t better communication-it’s systemic de-pathologization. But of course, that’s too inconvenient for a Reddit post.
Look, I get it-you want to feel better. But in America, we’ve turned medicine into a consumer product. You don’t ‘manage’ side effects. You demand results. If your blood pressure med makes you tired, switch to something that doesn’t. If your antidepressant gives you brain fog, find one that doesn’t. This ‘wait two weeks’ nonsense is just gatekeeping. You’re not a lab rat. You’re a patient. And if your doctor won’t adjust, find one who will. We have options. Use them.
Just took my meds with a banana instead of on empty stomach. Nausea gone. No doctor visit needed. This post saved me hours of stress. Thank you.
I think Jerian and Phil are both onto something-but they’re coming from opposite ends. The system is flawed, yes. But for many of us, meds are the only thing keeping us alive. I don’t want to dismantle the system-I want to fix it from the inside. That’s why I track. That’s why I ask questions. That’s why I bring my list to appointments. You can critique the structure and still fight to make it work for you. It’s not hypocrisy. It’s survival with integrity.
Oh wow, you tracked your dizziness? How cute. Did you also meditate on it? Did you write a poem about it? Maybe you should try crystals next. Some of us have real problems-not ‘mild nausea’ that disappears if you take it with toast. My side effects cost me my job. Your ‘SWIM framework’ doesn’t pay rent. Stop acting like this is just a lifestyle hack.
I cried so hard after my first dose I had to call my mom. I thought I was dying. I almost quit. Then I took it at night. Now I sleep better than I have in years. Side effects aren’t the enemy. Silence is. Just talk. Please. Just talk.
For real-try taking statins with a handful of almonds. My muscle pain dropped by like 80%. I didn’t even tell my doc. Just did it. Also, if you’re on antidepressants and feel worse at first? That’s totally normal. Your brain is rearranging the furniture. It’s not broken. Just… messy. Give it time. And maybe a snack.
My pharmacist told me to take my BP med with grapefruit juice. Said it boosts absorption. I did. My numbers dropped 20 points in a week. Never even told my doctor. Just kept doing it. Side effects? None. So yeah-pharmacists are the real MVPs. Don’t wait for your doc to fix it. Go ask the person who actually knows the drug.