Transferring a prescription shouldn’t feel like a gamble. Yet every year, thousands of people face delays, wrong dosages, or even dangerous mistakes because prescription labels get mixed up during transfer. It’s not just a paperwork issue-it’s a safety issue. A single misplaced decimal point on a label can mean the difference between a safe dose and a life-threatening overdose. The good news? There are clear, proven ways to make sure your prescription moves safely from one pharmacy to another-without losing accuracy.
Why Prescription Label Accuracy Matters More Than You Think
Medication errors linked to mislabeled prescriptions cause about 7,000 deaths in the U.S. each year. That’s not a guess-it’s from the Institute of Medicine. Most of these errors happen because labels change during transfer. A pharmacy might accidentally drop a decimal, forget to update refills, or misread a prescriber’s note. Even small things like writing ‘.4 mg’ instead of ‘0.4 mg’ can lead to a tenfold dosing error. The FDA says standardized labels could prevent 1.5 million adverse events annually. That’s why every digit, every word, every punctuation mark on your prescription label counts.
Regulations now demand exact formatting. Trailing zeros (like ‘1.0 mg’) are banned because they can be mistaken for ‘10 mg’. Leading zeros are required-so ‘0.4 mg’ is correct, but ‘.4 mg’ is not. Units must be spelled out (‘milligrams’, not ‘mg’ on some systems). These aren’t arbitrary rules. They’re based on real data from thousands of reported errors. In 2022, the National Coordinating Council for Medication Error Reporting and Prevention analyzed over 2,300 incidents and found that 12% of dosage mistakes came from unit confusion-like mixing up apothecary and metric systems. That’s why metric units are now mandatory across the board, except for insulin.
What’s Allowed in Prescription Transfers (And What’s Not)
Not all prescriptions can be transferred the same way. The rules changed dramatically in August 2023, when the DEA finally allowed electronic transfers of Schedule II controlled substances-like oxycodone or fentanyl-for the first time since the Controlled Substances Act of 1970. Before that, these prescriptions couldn’t be transferred at all. Now, you can transfer them once, electronically, and only once. No second transfers. No faxing. No phone calls.
For Schedule III-V drugs-like codeine or anabolic steroids-you can transfer up to the number of refills the prescriber originally authorized. Non-controlled prescriptions, like antibiotics or blood pressure meds, are more flexible. Most states allow multiple transfers, but rules vary. Wisconsin, for example, requires the receiving pharmacy to write the name, address, and DEA number of the transferring pharmacy on the back of the original prescription. Massachusetts has its own detailed standards under 247 CMR 9.00. There’s no single national rule anymore-but federal law now sets the minimum standard for electronic transfers.
Here’s what must be included on every transferred prescription label:
- Patient’s full name
- Drug name (no abbreviations like ‘HCTZ’-it must be ‘hydrochlorothiazide’)
- Strength in metric units (e.g., ‘5 mg’, not ‘5 mg’ with trailing zeros)
- Dosage form (tablet, capsule, liquid)
- Quantity dispensed
- Directions for use (e.g., ‘Take one tablet by mouth twice daily’)
- Prescriber’s name
- Prescription number
- Date issued
- Number of refills remaining
- Pharmacy name, phone number, and address
Any missing piece? The prescription is invalid. And if the label is altered-even by accident-it’s a violation.
How Electronic Transfers Keep Labels Safe
The safest way to transfer a prescription is electronically, using the NCPDP SCRIPT standard (version 2017071 or newer). These systems don’t just send data-they preserve it exactly as it was created. No typos. No lost refills. No truncation. A 2022 University of Florida study found these systems maintain 98.7% data integrity. Compare that to fax transfers (82.3% accurate) or phone calls (76.1% accurate). Phone transfers are still allowed for Schedule III-V drugs, but they’re risky. A pharmacist might mishear ‘20 mg’ as ‘200 mg’. That’s why most pharmacies now avoid them unless absolutely necessary.
When a transfer happens electronically, the transferring pharmacy must:
- Mark the prescription as transferred in their system
- Record the name, address, and DEA number of the receiving pharmacy
- Log the date and the pharmacist’s name who initiated the transfer
The receiving pharmacy must then:
- Add the word ‘transfer’ to the electronic record
- Include the name of the transferring pharmacy and pharmacist
- Verify all data matches the original
Pharmacies using these systems report fewer errors. One user on the Pharmacy Technician Forum said their system has a 99% success rate because it checks inventory before completing the transfer. That’s key-many transfers fail because the new pharmacy doesn’t have the drug in stock, and the patient doesn’t realize until they show up.
What Patients Need to Do (Yes, You Have a Role Too)
You’re not just a passive recipient. You’re part of the safety chain. Under the DEA’s 2023 rule, you must initiate the transfer. You can’t just show up at a new pharmacy and ask them to pull your prescription. You have to call or go in and request it. And before you do, ask: ‘Do you carry this medication?’
In California, after a 2022 law allowed outsourcing facilities to dispense prescriptions, 23% of transfer attempts failed because patients didn’t confirm the pharmacy had the drug. That meant three to five days without treatment. For controlled substances, that’s dangerous. Schedule II prescriptions can only be filled once. If the pharmacy doesn’t have it, you’re stuck until your prescriber issues a new one.
Here’s what to do:
- Call your new pharmacy first. Ask if they can fill your prescription.
- Have your prescription number, prescriber’s name, and drug name ready.
- Confirm how many refills remain.
- Ask if they use electronic transfer systems-avoid fax or phone if possible.
And never assume your old pharmacy sent it. Always follow up. If your meds don’t show up within 24 hours, call the new pharmacy. Ask them to check their system for incoming transfers.
Common Problems-and How to Avoid Them
Even with good systems, things go wrong. Here are the top three issues and how to dodge them:
1. System Incompatibility
Not all pharmacy software talks to each other. In 2022, the National Community Pharmacists Association found 18% of pharmacies reported data truncation during transfers-meaning part of the label got cut off. If your directions say ‘Take one tablet twice daily for 14 days’ and only ‘Take one tablet’ comes through, that’s a problem. Always double-check the label when you pick up your meds. If anything looks off, ask the pharmacist to verify the original.
2. Staff Turnover and Training Gaps
Pharmacists and technicians change jobs. New staff may not know the updated DEA rules. Training takes about 8.5 hours to reach 95% compliance, according to the American Pharmacists Association. If you notice a pharmacist hesitating or asking a lot of questions about your transfer, it’s okay to ask: ‘Are you familiar with the 2023 DEA transfer rules?’ Most will appreciate the reminder.
3. Inconsistent State Rules
Dr. Jerry Phillips, former FDA director of medication errors, called state transfer rules a ‘patchwork’ that increases risk. A pharmacy in Texas might accept a faxed transfer of a Schedule III drug, but one in New York won’t. If you’re moving or traveling, always check your new state’s pharmacy board rules. You can find them online-just search ‘[State] pharmacy board prescription transfer rules’.
What’s Coming Next: The 2025 Labeling Rule
The FDA’s Patient Medication Information (PMI) rule takes full effect in 2025. It requires all prescription labels to be written in plain language, with a paper copy as the default (unless you ask for digital). Labels will include:
- Clear warnings (e.g., ‘May cause drowsiness’)
- Instructions in simple sentences
- Barcodes that scan for accuracy before dispensing
- Automated checks for drug interactions and dosage limits
Early adopters say it’s expensive-$12,500 to $18,750 per pharmacy to upgrade systems. But it’s coming. And when it does, your labels will be easier to understand and harder to misread. The goal? Reduce medication errors by 30%, as Dr. Michael Cohen of ISMP predicted. That’s not just a number-it’s fewer hospital visits, fewer overdoses, fewer deaths.
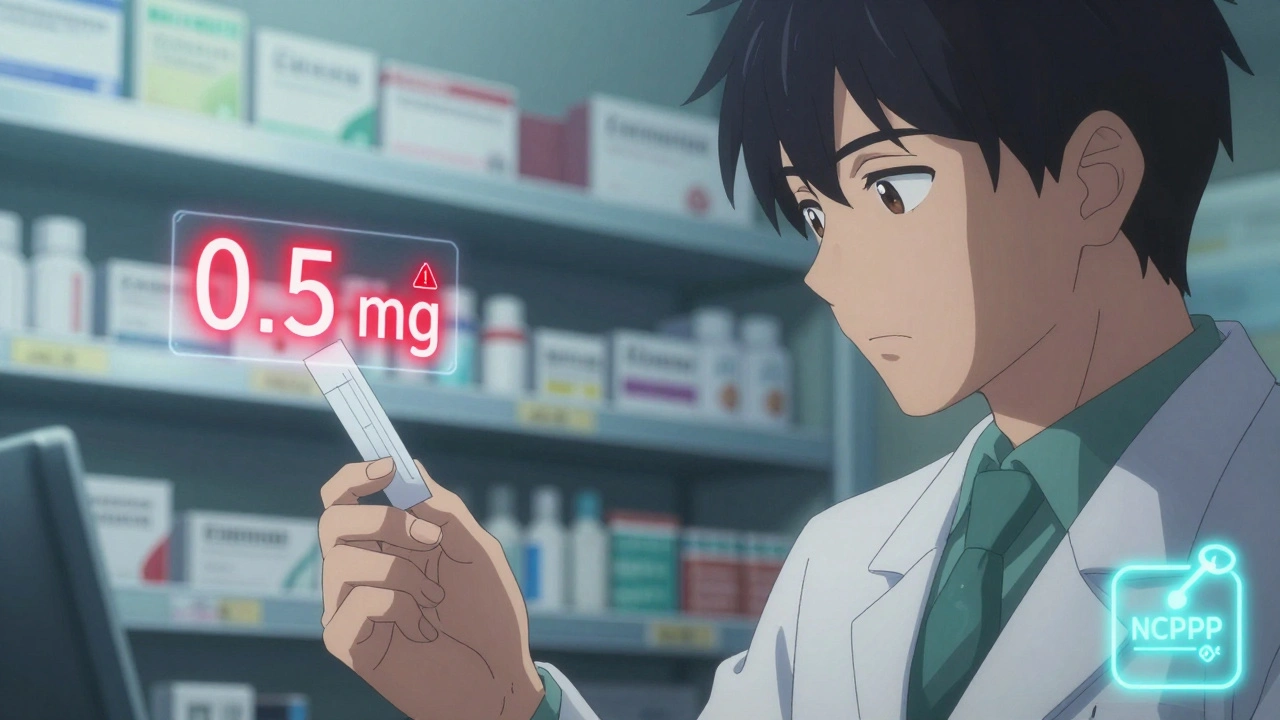
Final Checklist Before You Leave the Pharmacy
Before you walk out with your transferred prescription, do this quick check:
- Is your full name spelled correctly?
- Does the drug name match what your doctor prescribed? (No abbreviations like ‘MOM’ or ‘HCTZ’)
- Is the strength written with a leading zero? (e.g., 0.5 mg, not .5 mg)
- Is there a trailing zero? (e.g., 1 mg, not 1.0 mg)
- Do the directions make sense? (If it says ‘take every 4 hours’ but you were told ‘twice daily’, ask for clarification)
- Is the number of refills correct?
- Does the label include the pharmacy’s phone number?
If anything looks off, don’t leave. Ask the pharmacist to verify the original electronic record. Better safe than sorry.
Can I transfer a Schedule II prescription more than once?
No. As of August 2023, DEA rules allow only one electronic transfer for Schedule II controlled substances like oxycodone or fentanyl. After that, the original prescription is voided, and a new one must be written by your prescriber. This rule was created to reduce diversion and misuse.
What if my new pharmacy says they can’t accept my electronic transfer?
Some rural or small pharmacies still use outdated systems that don’t support NCPDP SCRIPT standards. If this happens, ask if they can receive the transfer via fax or phone-but only for Schedule III-V drugs. For Schedule II, you’ll need to contact your prescriber for a new prescription. Always confirm your new pharmacy’s capabilities before initiating the transfer.
Why can’t I just call my old pharmacy to transfer my prescription?
You can’t. The DEA requires the patient to initiate the transfer. This prevents unauthorized access and ensures you’re aware of where your prescription is going. Your old pharmacy won’t transfer it unless you specifically request it at the new pharmacy. This is a safety feature, not a bureaucracy.
Are handwritten prescriptions still allowed for transfers?
Handwritten prescriptions can be transferred, but only if they’re scanned into an electronic system first. The DEA’s 2023 rule requires all transfers between retail pharmacies to be electronic. Paper prescriptions must be digitized using a certified system before transfer. Faxing a handwritten script is not allowed for Schedule II drugs and is discouraged for others.
What should I do if I get the wrong dosage after a transfer?
Stop taking the medication immediately. Call your pharmacist and your prescriber. Report the error to the pharmacy’s quality assurance team. You can also report it to the FDA’s MedWatch program. Keep the incorrect label and packaging as evidence. Most pharmacies will replace the medication at no cost and review their process to prevent future errors.



Just transferred my dad’s oxycodone script last week-electronic, no drama. The new pharmacy’s system flagged a trailing zero in the original label. Saved us from a potential overdose. Seriously, folks: check those decimals. It’s not paranoia, it’s protocol. 🇦🇺
There’s something deeply human about how we treat medication labels like sacred texts-and yet, we treat them like old napkins. This post isn’t just about rules. It’s about dignity. That decimal point? It’s not a typo. It’s a life. We’re not just dispensing pills-we’re holding someone’s fragile trust in our hands. And when the system fails, it’s not a glitch. It’s a betrayal.
That’s why I’m grateful for these standards. Not because they’re bureaucratic, but because they’re compassionate. They force us to slow down. To see the person behind the prescription.
Let’s not just comply. Let’s honor it.
⚠️ ALERT: BIG PHARMA IS USING THESE ‘STANDARDS’ TO TRACK YOU! 🕵️♀️
Did you know the barcode on your label is linked to your phone? And the ‘electronic transfer’? That’s just the NSA’s new way of monitoring your pain meds. I heard a pharmacist at CVS say they’re building a database that connects your prescriptions to your social media. 😳
Also, ‘leading zeros’? That’s just the first step. Next they’ll make you wear a chip. I’m switching to herbal tea. 🌿 #BigPharmaIsWatching
The regulatory framework governing prescription transfers is not merely a procedural artifact; it is a critical component of pharmacovigilance infrastructure. The adoption of the NCPDP SCRIPT standard, particularly version 2017071 and later, represents a paradigmatic shift from analog risk mitigation to digital integrity assurance.
Furthermore, the elimination of trailing zeros and the mandatory inclusion of full drug nomenclature are not arbitrary conventions-they are evidence-based interventions derived from the analysis of over 2,300 medication error incidents by the National Coordinating Council for Medication Error Reporting and Prevention. These are not suggestions. They are clinical imperatives.
It is also noteworthy that the requirement for patient-initiated transfers under the DEA’s 2023 rule serves as a necessary safeguard against unauthorized access, aligning with the principles of patient autonomy and informed consent as codified in the HIPAA Privacy Rule.
Pharmacies that resist electronic integration are not merely outdated-they are endangering public health. The cost of upgrading systems pales in comparison to the cost of preventable harm.
Man, I used to think transferring prescriptions was just a hassle-until my wife almost got the wrong dose of her blood pressure med last year. We were rushing, didn’t check the label, and the pharmacy had accidentally dropped the ‘0’ in ‘0.5 mg’-turned it into ‘.5 mg’ and the system didn’t catch it because it was a fax transfer. She ended up in the ER with a heart palpitation.
After that, I became a total label nerd. Now I check every single thing before I walk out: name, strength, refills, directions. I even ask them to read it back to me. I know it sounds crazy, but I’d rather be annoying than dead.
And yeah, I call the new pharmacy first now. No more ‘oh, they’ll send it over.’ Nope. I’m the one who has to say ‘hey, I need my script moved.’ It’s weird how much power you have when you just speak up.
Also, if your pharmacy still uses fax? Run. Seriously. Even if it’s ‘convenient.’
And if you’re moving states? Google your state’s pharmacy board. I did it before I moved from Ohio to Florida. Saved me three days without my meds. You’re not just a patient-you’re your own best advocate. Don’t forget that.
Let’s be real-this whole ‘standardization’ nonsense is just another way for the government and Big Pharma to control the population. You think they care about your safety? No. They care about liability. They care about lawsuits. They care about making sure you never question your meds, never challenge the system, never think for yourself.
Why can’t you just call your old pharmacy? Because they want you to feel powerless. Why do you have to initiate the transfer? So you’re the one taking responsibility when something goes wrong. That’s the game.
And don’t get me started on the ‘plain language’ rule. They’re dumbing down medicine for people who can’t read. You think a 70-year-old with diabetes needs to see ‘Take one pill daily’? No-they need to know the science. They need to understand the mechanism. But no, let’s treat everyone like children.
And barcodes? That’s surveillance. They’re tracking your every pill. You think that’s for safety? It’s for control.
Wake up. This isn’t healthcare. It’s corporate compliance dressed up in a white coat.
I just had to transfer my antidepressant script last month and honestly? I was terrified. I didn’t know what to ask, I was scared they’d say ‘we don’t carry it’ and I’d be without for days...
When I called the new pharmacy, the tech on the other end just said, ‘Hey, I’ve been there. Let me walk you through it.’ She even checked if I had any allergies in their system. I cried a little.
It’s easy to think of pharmacies as faceless machines-but they’re not. People are trying. Really trying. And sometimes, when you’re in that vulnerable place, a little kindness makes all the difference.
Thank you to every pharmacist who double-checks. You’re doing more than you know. 💛
Everyone’s acting like this is some groundbreaking revelation. Newsflash: this has been common sense for decades. The fact that we need a 2,000-word guide to prevent a decimal point from killing someone is a national disgrace. We’re talking about life-or-death precision in a system run by underpaid, overworked, poorly trained staff using 15-year-old software. And we’re surprised when people die?
The real problem isn’t the rules-it’s the culture. We treat medication like a commodity, not a clinical intervention. We optimize for speed, not safety. We cut corners because ‘it’s just a script.’
And now we pat ourselves on the back for ‘fixing’ it with electronic transfers? That’s not innovation-that’s damage control. We’re still playing whack-a-mole with preventable deaths.
Until we stop treating pharmacists as order-fillers and start treating them as clinical partners, none of this matters. The system isn’t broken. It was designed this way.