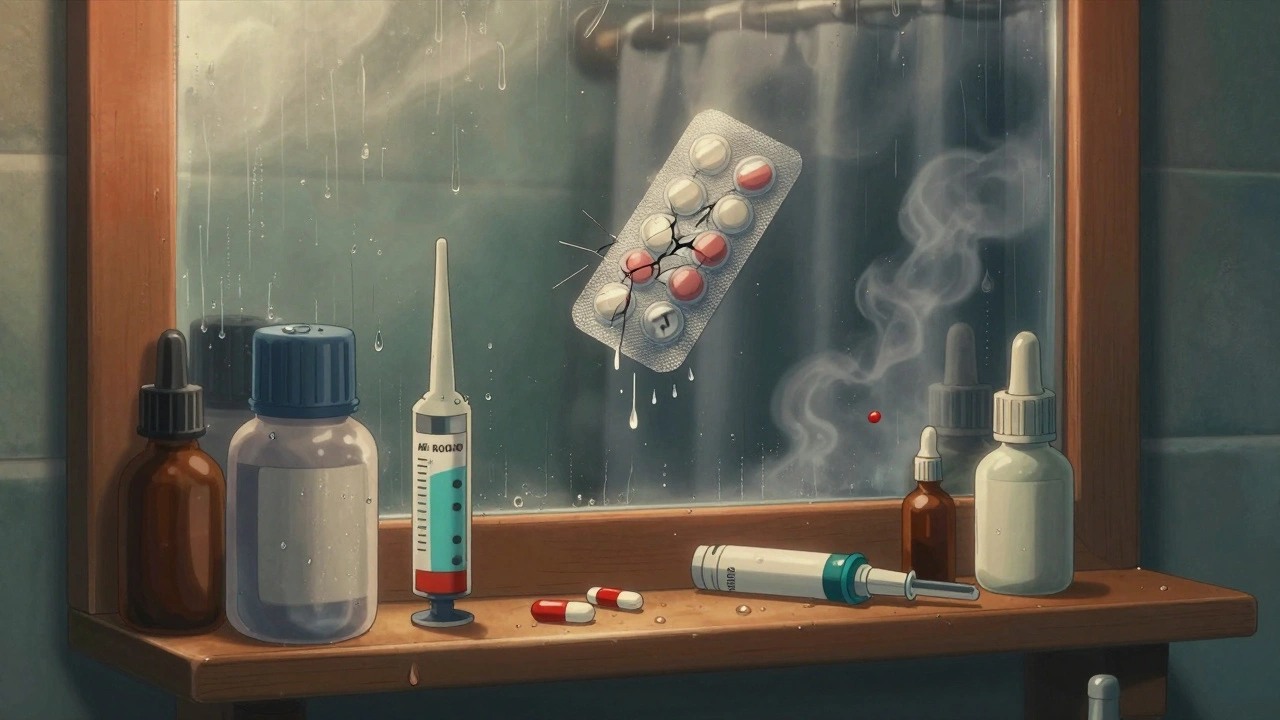
Most people assume their pills and liquids last until the date printed on the bottle-no matter where they’re kept. But if your medicine sits in a steamy bathroom or a hot car, that expiration date might be meaningless. Heat and humidity don’t just make you uncomfortable-they can break down your medication faster than you think, turning life-saving drugs into useless-or even dangerous-substances.
Why Your Medicine Doesn’t Last as Long as It Should
Pharmaceutical companies test medications under strict conditions: a steady 20-25°C (68-77°F) and 35-65% humidity. That’s the baseline for the expiration date you see on the label. But real life? Your bathroom hits 80% humidity after a shower. Your kitchen gets hotter than 32°C (90°F) near the stove. Your car hits 60°C (140°F) in the sun. None of that matches the lab. When heat and moisture creep in, the chemical structure of the drug starts to break down. It doesn’t always look different. No warning label pops up. You won’t feel it. But the active ingredient? It’s losing power. A tablet might still look fine, but if it’s been sitting above 30°C for weeks, it could be 20% weaker. That’s not a small drop-it’s the difference between controlling your blood pressure and ending up in the hospital.Which Medications Are Most at Risk?
Not all meds are created equal. Some can handle a little heat. Others fall apart fast. Insulin is one of the most dangerous cases. If it’s left at 37°C (98.6°F) for just 24 hours, it can lose up to 20% of its potency. For someone with diabetes, that means blood sugar spikes they can’t explain. No one checks the temperature of their insulin pen-until it’s too late. Nitroglycerin, used for heart attacks, breaks down rapidly above 25°C. If your chest pain hits and your nitro doesn’t work, it’s not because you’re imagining it-it’s because the pill degraded in your wallet or purse during a summer drive. Antibiotics like amoxicillin suspension? Once opened, they need refrigeration. At room temperature, they lose 30-40% of their strength in just three days. That’s not just ineffective-it’s a direct path to antibiotic resistance. Bacteria survive, multiply, and become harder to kill. Biologics-like monoclonal antibodies for cancer or autoimmune diseases-are made of proteins. Heat above 8°C (46.4°F) can permanently destroy their shape. Once that happens, they’re useless. No second chances. Even EpiPens are at risk. Above 30°C, the internal mechanism can fail. The spring might not fire. The needle might not deploy. In a life-or-death allergic reaction, that’s not a risk you can afford.What About Common Pills Like Ibuprofen or Acetaminophen?
Solid tablets like ibuprofen, aspirin, or statins are tougher. They can handle temperatures up to 40°C (104°F) for a month and still keep 85-90% of their strength. That doesn’t mean you should store them in the attic, though. Aspirin is a sneaky one. When it absorbs moisture, it breaks down into salicylic acid and acetic acid-that’s vinegar. You might smell it. You might not. But that breakdown can irritate your stomach more than the original pill. And if you’re taking it for heart protection, losing potency means you’re not getting the full benefit.
Where NOT to Store Your Medications
The bathroom medicine cabinet is the worst place. It’s hot, wet, and full of steam. Every shower pushes humidity up to 70-90%. That’s enough to soften capsules, make tablets stick together, or cause coatings to break down. Moisture can also ruin the time-release layers on extended-release pills, making them dump their entire dose at once. The kitchen is almost as bad. Near the stove, oven, or sink, temperatures regularly climb above 32°C. Humidity spikes from boiling water or dishwashing add to the damage. Even a drawer above the fridge can get warm from the motor running. And don’t leave meds in your car-not even for an hour. On a 30°C day, the inside of a parked car can hit 60°C. That’s enough to melt capsules, warp inhalers, or even cause aerosol cans to explode. Inhalers have propellants under pressure. Heat makes them expand. One too many hot days, and you’re not just out of medicine-you’re out of a car window.What Does Degraded Medicine Look Like?
Sometimes, you can tell. Look for:- Color changes-pills turning yellow, brown, or faded
- Unusual smells-like vinegar, mold, or chemicals
- Tablets that are sticky, crumbly, or harder than usual
- Capsules that are cracked, swollen, or leaking
- Liquids that look cloudy or have particles floating in them
Where to Store Medications Instead
The best place? A cool, dry, dark spot-like a bedroom drawer, away from windows. Keep it in the original container with the cap tightly closed. That packaging was designed to block light and moisture. For insulin, epinephrine, or other temperature-sensitive drugs, use a small insulated bag with a cool pack from the pharmacy. These aren’t fancy-they cost under $10. But they can save your life during travel, heatwaves, or power outages. If you’re going on a trip, only take what you need for the days you’ll be away. Leave the rest at home in the right conditions. Don’t risk a whole bottle just because you’re too lazy to split it up.
The Real Danger: It’s Not Just About Potency
Losing strength sounds bad, but it’s not the only risk. Degraded medications can create new, harmful compounds. Broken-down antibiotics can trigger allergic reactions. Degraded thyroid meds can cause heart palpitations or weight swings. Even a slightly off dose of a seizure drug can trigger a seizure. The FDA says using expired or improperly stored meds is risky-and possibly harmful. That’s not a warning they throw around lightly. It’s based on real cases: patients who got sick because their insulin didn’t work, or whose EpiPen failed during anaphylaxis. And here’s the quiet crisis: we don’t track how many people get hurt this way. There’s no national database. No one reports, “I took my old pills and got worse.” But doctors see it. Pharmacists see it. Nurses see it. It’s happening every day.What’s Changing? What Should You Expect?
Pharmacies are starting to use better packaging: desiccants inside bottles, opaque blister packs, and temperature-sensitive labels that change color if the drug got too hot. Some companies are testing smart bottles with built-in sensors that connect to your phone-alerting you if your medicine was exposed to bad conditions. But until those become standard, you’re still the last line of defense. You’re the one who decides where the pills go. You’re the one who notices if something looks off. Climate change is making this worse. Heatwaves are longer. Humidity is higher. In places like Sydney, where summer temps regularly hit 40°C, even indoor storage can be risky if you don’t have air conditioning. The World Health Organization has flagged medication stability in hot climates as a growing public health threat. It’s not just a problem in developing countries. It’s here. Now.What to Do Today
1. Check every medicine in your home. Look for discoloration, odd smells, or damaged packaging. 2. Move your meds out of the bathroom and kitchen. Find a drawer in a cool room. 3. Ask your pharmacist if any of your prescriptions need special storage. Don’t assume-they’ll tell you. 4. When traveling, use a cool pack. Keep insulin, EpiPens, and thyroid meds in a small insulated bag. 5. Dispose of anything suspicious. Don’t risk it. Pharmacies often have take-back programs. Expiration dates are a promise. But that promise only holds if you keep the conditions right. Heat and humidity don’t care about your schedule. They don’t care if you’re busy, tired, or forgot. They just keep working-slowly, quietly-breaking down your medicine. You don’t need to be a scientist to protect your health. You just need to know where to put the bottle.Can I still use my medicine after the expiration date if it looks fine?
No. The expiration date is the last day the manufacturer guarantees the medicine is fully potent and safe-only if stored correctly. If it’s been exposed to heat or humidity, it may have degraded even before that date. Looking normal doesn’t mean it’s still working. Taking it could be ineffective or harmful.
Does refrigerating all medications make them last longer?
No. Only specific medications-like insulin, some antibiotics, and biologics-need refrigeration. Others, like tablets and capsules, can break down faster in the fridge due to moisture. Always check the label or ask your pharmacist. Storing the wrong medicine in the fridge can do more harm than good.
What should I do if I think my medication has been damaged by heat?
Stop using it immediately. Look for signs like color changes, odd smells, or damaged packaging. Contact your pharmacist or doctor-they can advise if you need a replacement. Never try to guess whether it’s still safe. For life-saving drugs like insulin or EpiPens, err on the side of caution.
Can I store my medications in the fridge to avoid heat?
Only if the label says so. Most solid pills and capsules should be kept at room temperature in a dry place. Fridges create condensation, which introduces moisture-another enemy of medication stability. Moisture can cause tablets to crumble or capsules to stick. Always follow the storage instructions on the bottle.
Are there any medications that are immune to heat and humidity?
No medication is completely immune. But solid oral tablets like ibuprofen, acetaminophen, and most statins are more stable than liquids, injections, or biologics. Even these can degrade over time if exposed to extreme conditions. The key is consistency: keep them cool, dry, and out of direct light. No exceptions.




I never thought about my bathroom cabinet being a science experiment for my meds. Learned something today. Thanks for the reminder.
So you're telling me my 3am painkiller stash by the toilet was basically a science project? Cool. I'll just keep doing that then.
This is actually really important. I had a friend whose insulin went bad during a heatwave and they ended up in the ER. Never leave meds in the car.
Of course the pharma giants want you to buy new pills every month. They don't care if your aspirin works fine for 2 years. They just want your money. And don't get me started on how the FDA is in their pocket. You think they'd tell you if your meds were secretly turning toxic?
I always keep my meds in a sealed plastic container with a silica pack in my bedroom drawer... and I just checked my insulin pen-still cool. Thank you for validating my weird habits.
I used to store my blood pressure meds in the kitchen near the stove because it was convenient. Now I feel like an idiot. I moved them last night. No more excuses.
The degradation kinetics of thermolabile biologics under elevated RH and T° conditions are frankly under-discussed in public health discourse. One must consider the Arrhenius equation in relation to protein denaturation thresholds-especially in the context of climate-induced thermal stressors. Also, 🌡️🔥💊
I appreciate the clarity and precision of this post. It’s not often that medical advice is delivered with such thoroughness and practical guidance. For those unfamiliar with pharmaceutical stability, this is a masterclass in patient safety.
I’ve been wondering why my thyroid med stopped working last summer-then I remembered I left it in my purse during a road trip to Florida. The car hit 120 degrees. Now I think about it, maybe that’s why I gained 20 pounds and had panic attacks. And now I’m thinking… what if the FDA knows this happens to millions and just doesn’t care? What if they’re letting people get sick so they keep buying new prescriptions? And what if the silica gel packs in the bottles are actually a scam because they don’t last long enough? And what if the expiration date is just a lie because the real shelf life is way longer and they’re just forcing us to repurchase? And what if my EpiPen didn’t work last time because the manufacturer knew it’d fail in heat and they didn’t fix it because it’s cheaper to pay off lawsuits than to engineer better packaging?
I’ve got a cousin with diabetes who lives in Arizona. She carries her insulin in a little insulated case with a cold pack. She’s been doing it for years. Smart person. I’m going to start doing the same with my blood pressure meds.
I never realized how much moisture affects pills. I used to leave my antibiotics on the sink. Now I know why they tasted weird. I’m moving them to the closet.
I work in a pharmacy. We get people bringing in meds that have been left in cars, bathrooms, and sunlit windows. The most heartbreaking? Parents who gave their kid expired epinephrine because they didn’t know it needed refrigeration. Please, please, please check the label. Or ask. We’re here to help.
I just checked my meds. My ibuprofen is fine. My EpiPen? Still good. My insulin? Still cold. I’m not a genius. I just didn’t ignore the warning signs. You don’t need to be a scientist to save your life. Just don’t be lazy.