When a drug has a NTI generics profile, even tiny changes in how much of it enters your bloodstream can mean the difference between healing and harm. Think of warfarin, phenytoin, or levothyroxine - these aren’t ordinary pills. One day, your blood level might be just right. The next, after switching to a generic version, it could drop too low or spike dangerously high. That’s why regulators around the world treat NTI generics differently than regular generics. And those differences matter - a lot.
What Makes NTI Drugs So Risky?
NTI stands for Narrow Therapeutic Index. It means the gap between a dose that works and one that causes toxicity is razor-thin. For most medications, a 10% variation in blood concentration won’t hurt. For NTI drugs, that same shift can trigger seizures, blood clots, or thyroid crashes. The FDA defines NTI drugs as those where small changes in dose or blood levels can lead to serious therapeutic failure or life-threatening side effects. That’s not theoretical. In 2021, a generic antihypertensive drug was pulled because of nitrosamine impurities - contaminants that can form during manufacturing and are especially dangerous in drugs where precision is everything.
These aren’t rare drugs. Warfarin, used to prevent strokes, is one of the most prescribed NTI drugs in the U.S. Levothyroxine, for hypothyroidism, affects millions. Phenytoin, an anti-seizure medicine, is critical for epilepsy patients. If a generic version isn’t bioequivalent down to the last decimal point, patient safety is at risk. That’s why regulators don’t just copy-paste the same rules they use for antibiotics or painkillers.
The U.S. Approach: Tighter Limits, Patchwork Rules
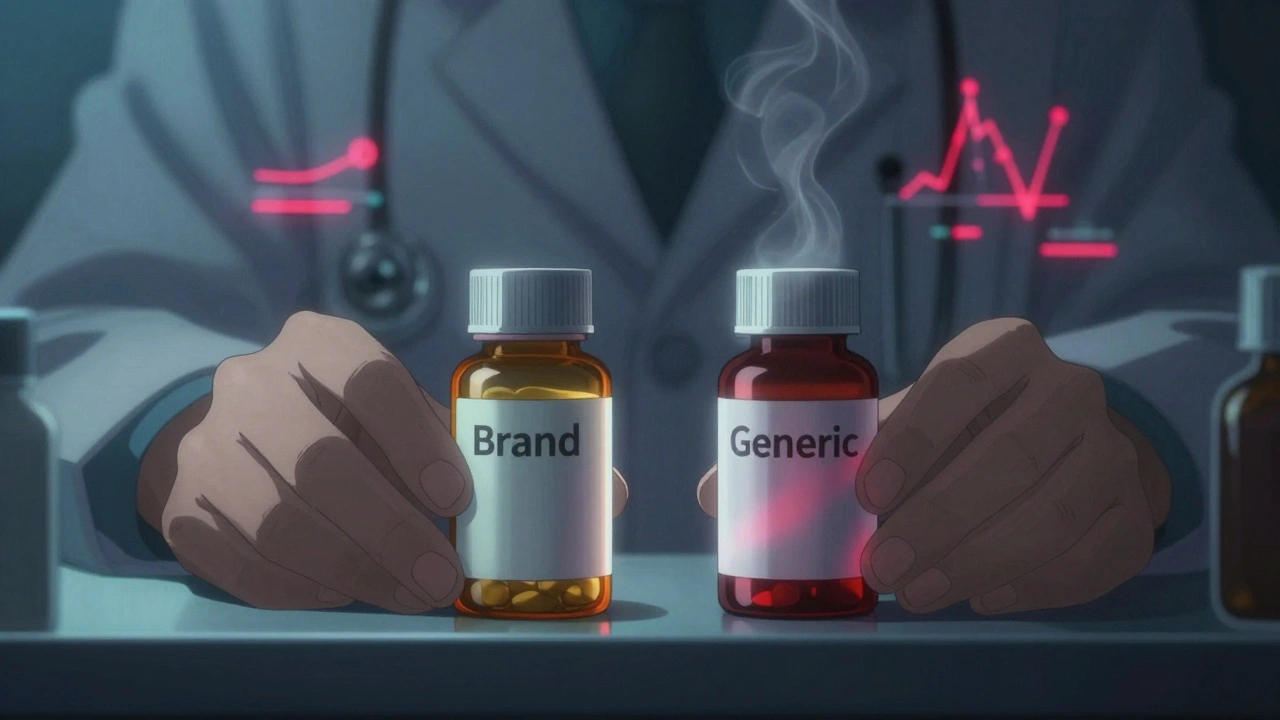
The FDA treats NTI generics like high-stakes precision instruments. For regular generics, bioequivalence is accepted if the generic’s absorption rate falls within 80-125% of the brand. For NTI drugs, the FDA tightened that to 90-111% - and sometimes even narrower. The quality assay, which measures how much active ingredient is in each pill, must be 95-105% instead of the standard 90-110%. That’s a huge difference in manufacturing control.
But here’s the catch: the FDA sets the standard, but states decide if pharmacists can swap brand for generic. Twenty-six U.S. states have special rules for NTI drugs. North Carolina requires both doctor and patient to sign off before substitution. Connecticut, Idaho, and Illinois demand extra warnings for anti-epileptic generics. Some states even ban substitution for levothyroxine entirely.
Pharmacists report real-world problems. A 2019 survey found 67% of U.S. pharmacists get calls from doctors asking them not to substitute NTI generics. On Reddit, pharmacists share stories of patients whose thyroid levels swung wildly after switching brands - even when the FDA said the generics were equivalent. One pharmacist wrote: “I’ve had three cases this year where patients had abnormal TSH levels after switching generics. We had to go back to the brand.”
Europe’s Fragmented System: Centralized Goals, Local Realities
The European Medicines Agency (EMA) has a more unified approach on paper. It offers a Centralized Procedure that, if approved, lets a generic be sold across all EU countries. But in practice, it’s messy. Only 68% of new generic applications used this route in 2022 - up from 42% in 2018 - meaning most still go through national systems with different rules.
Where the U.S. focuses on bioequivalence limits, Europe leans into pricing. In 24 of 27 EU countries, governments control how much generics cost. Spain forces the first generic to launch at least 40% cheaper than the brand. Others tie prices to the original drug’s cost. This drives fierce competition - but also pushes manufacturers to cut corners. The EMA’s bioequivalence standards are strict, but not as numerically rigid as the FDA’s. Still, they require multi-point dissolution testing and often demand studies in healthy volunteers, not patients, to reduce variability.
European pharmacists aren’t immune to confusion. A 2022 survey by the European Association of Hospital Pharmacists found 58% struggled with substitution rules across borders. A generic approved under the Decentralized Procedure in Germany might not be allowed in France. That creates a patchwork that’s hard for patients and providers to navigate.
Canada and Japan: Precision with Flexibility
Canada takes a pragmatic route. Health Canada allows foreign reference products - like the U.S. brand - to be used in bioequivalence studies, as long as they match the Canadian formulation exactly. They also require detailed dissolution profiles across multiple pH levels, which helps predict how the drug behaves in different parts of the body. This flexibility helps speed up approval without sacrificing safety.
Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) is known for its meticulous standards. They’ve published detailed guidance for topical NTI drugs - a category with complex absorption patterns. Their approach is highly technical, with heavy reliance on in vitro testing and predictive modeling. Japanese regulators expect manufacturers to prove stability under extreme conditions - heat, humidity, light - long before approval.
The Global Push for Harmonization
There’s a growing consensus that the current patchwork doesn’t work. That’s why the International Generic Drug Regulators Pilot (IGDRP) was launched in 2012. It includes the U.S., EU, Canada, Japan, South Korea, Switzerland, Taiwan, and Singapore. The goal? Align testing methods, data requirements, and approval timelines.
Progress is slow but real. In 2023, the ICH adopted the M9 guideline on biowaivers - a big step toward reducing unnecessary animal and human testing for certain NTI drugs. The FDA’s GDUFA III, also launched in 2023, adds new post-market surveillance requirements for NTI generics. The EMA is moving more applications into its Centralized Procedure. Experts believe these efforts could cut approval times by 25-30% over the next decade.

Why It Costs So Much and Takes So Long
Developing an NTI generic isn’t like copying a song. It’s like rebuilding a Swiss watch with identical gears. The process takes 18-24 months and costs $5-7 million - nearly double the price of a regular generic. Why? Because you need:
- Multiple bioequivalence studies with healthy volunteers
- Stress testing under extreme conditions
- Advanced dissolution modeling across pH levels
- Extensive analytical validation for every batch
And even then, the rejection rate is 22% higher than for non-NTI generics. One failed dissolution profile can delay approval by a year. That’s why smart companies engage with regulators early - through FDA’s Complex Generic Drug Product Development Meetings or EMA’s Scientific Advice sessions. Those early talks can shave off 30-45 days from the timeline.
Market Reality: Growth Amid Risk
The global NTI generics market hit $48.7 billion in 2022 and is expected to hit $72.3 billion by 2027. The U.S. leads with 42% of sales; Europe follows at 34%. Teva, Mylan, Sandoz, and Hikma control over 40% of the market. But adoption varies wildly. Warfarin generics are used in 92% of cases in the U.S. Levothyroxine? Only 67%. Why? Because doctors still fear the swings.
Here’s the irony: a 2021 study of 12,500 patients across 15 European countries found that when strict bioequivalence rules were followed, NTI generics performed just as well as brands - 94.7% of the time. The problem isn’t the science. It’s the fear, the inconsistency, and the lack of trust.
What’s Next?
The future of NTI generics lies in smarter science and better communication. The FDA is planning to adopt population bioequivalence methods by 2025 - a new statistical approach that looks at how groups of people respond, not just averages. That could make approval more accurate for complex formulations like extended-release pills.
Meanwhile, manufacturers are investing in predictive modeling and AI-driven dissolution tools to catch problems before they reach the lab. Regulators are pushing for shared databases of bioequivalence data. And prescribers? They’re slowly learning that not all generics are created equal - and that the right generic, properly tested, can be just as safe as the brand.
The bottom line: NTI generics aren’t just another drug. They’re a test of how well global systems can protect patients when precision isn’t optional - it’s life or death.
Are all generic drugs the same as brand-name drugs?
No. For most drugs, generics are considered equivalent if they absorb into the body within 80-125% of the brand. But for NTI drugs - like warfarin, phenytoin, or levothyroxine - the acceptable range is tighter: often 90-111%. Even small differences in absorption can cause serious side effects or treatment failure. That’s why regulators apply stricter standards to NTI generics.
Why do some doctors refuse to allow generic substitution for NTI drugs?
Many doctors have seen patients experience unstable blood levels after switching generics - even when the FDA says they’re equivalent. Studies show that 67% of U.S. pharmacists get requests from physicians to avoid substituting NTI generics. Levothyroxine and anti-seizure drugs are the most common concerns. While properly tested generics are safe, inconsistent manufacturing or state-level substitution rules add uncertainty.
Which countries have the strictest NTI generic regulations?
The U.S. FDA has the most numerically precise standards, with tighter bioequivalence limits (90-111%) and quality assay ranges (95-105%). Japan’s PMDA requires extensive stress testing and detailed dissolution profiles. Canada allows foreign reference products but demands high-quality data. The EMA has strong standards but lacks full harmonization across its 27 member states, leading to variability in practice.
Is it safe to switch between different generic versions of an NTI drug?
It depends. If all versions meet the same strict bioequivalence criteria - like those required by the FDA or EMA - then switching should be safe. But in places with inconsistent standards or where pharmacists switch brands without oversight, patients may experience fluctuations. Experts recommend sticking with one generic manufacturer unless there’s a clear medical reason to change.
What’s being done to improve global NTI generic standards?
The International Generic Drug Regulators Pilot (IGDRP) brings together regulators from the U.S., EU, Canada, Japan, and others to align testing methods. The ICH M9 guideline, adopted in 2023, helps reduce unnecessary testing. The FDA’s GDUFA III now requires better post-market monitoring. These steps aim to reduce approval times, improve consistency, and build trust in generic NTI drugs worldwide.



Man i just switched my levothyroxine brand last month and my heart was racing for a week. Thought i was having a panic attack but nope, just my thyroid going haywire. My doc had to switch me back and now i just stick with the brand even though it costs 3x more. Worth it.
The regulatory fragmentation is honestly a nightmare for global patients. I work with patients who travel between the US and UK and the inconsistency in what generics they can get is absurd. One pharmacy says it’s fine, another refuses. No one has a clear answer. The science is there, but the system isn’t built to handle cross-border trust. We need a unified bioequivalence standard, not 30 different versions of the same rule.
I’m a pharmacist in rural Ohio and let me tell you, the phone calls about NTI generics never stop. Patients come in confused, scared, some even crying because their TSH jumped 3 points after a switch. We don’t have the time to explain dissolution profiles or pH-dependent absorption. All we can say is ‘stick with what works.’ The FDA’s 90-111% rule sounds good on paper, but in real life, patients aren’t numbers. They’re people who lose sleep over pill changes.
Of course the FDA has the strictest rules. Because America always has to be the most careful, even when it’s unnecessary. Other countries manage fine. We’re just scared of lawsuits and insurance companies. Meanwhile, real people suffer because we won’t let them save money on meds. It’s not safety-it’s control dressed up as science.
One might argue that the entire NTI regulatory paradigm is a modern myth, constructed by pharmaceutical monopolies to preserve market dominance under the guise of safety. The bioequivalence thresholds are statistically arbitrary. The human body is not a lab rat. The notion that a 9% variance in absorption constitutes ‘life or death’ is a narrative, not a law of nature. We worship precision where chaos is inevitable.
I had a friend on warfarin who switched generics and ended up in the ER with a blood clot. She was fine before. Now she’s terrified to ever switch again. I didn’t even know NTI drugs were a thing until that happened. This isn’t just about science-it’s about trust. And right now, patients don’t trust the system. And honestly? I don’t blame them.
My mom’s on levothyroxine and she’s been on the same generic for 7 years. One day the pharmacy switched her without telling her and she got dizzy, nauseous, and couldn’t sleep for three days. We called the doctor, they blamed the pharmacy, the pharmacy blamed the manufacturer. No one took responsibility. This isn’t regulation-it’s chaos with a FDA stamp on it.
So the US spends $7 million to make a generic that’s ‘safer’… and India makes it for $500k and it works fine? Interesting. Maybe the real issue isn’t the science-it’s the profit margins. The more complicated the rules, the fewer companies can play. And guess who wins? The ones who already own the brand.
Okay but have you considered that maybe the reason NTI generics are so controversial is because doctors are just lazy and don’t want to learn new things? They see ‘generic’ and immediately think ‘dangerous’ without checking the actual bioequivalence data. Meanwhile, patients are stuck paying $300 for a pill that should cost $20. This isn’t science, it’s fear-based capitalism.
Just had a pharmacist tell me my generic phenytoin was ‘equivalent’ but refused to fill it because ‘it’s not the same brand.’ I asked what that even means if it passed FDA testing. He shrugged. This system is broken. We need transparency-like QR codes on bottles showing the exact manufacturer and batch data. Not this vague ‘trust us’ nonsense.
The current bioequivalence paradigm is fundamentally inadequate for complex formulations like extended-release NTI drugs. The Cmax and AUC metrics are population-level aggregates that mask inter-individual variability in absorption kinetics. We need population bioequivalence models and in vitro-in vivo correlation (IVIVC) frameworks to properly assess therapeutic equivalence. Until then, we’re optimizing for regulatory compliance, not clinical outcomes.
If a pill works, why does it matter who made it? People are scared of change. But if two pills have the same active ingredient and pass the same tests, they should be interchangeable. Maybe the real problem isn’t the drugs-it’s the fear we’ve been taught to feel about them.
Did you know the FDA’s NTI guidelines were written by former pharma executives? Of course they’re strict-because they want to keep you buying the brand. The ‘impurities’ they scare you about? Most are harmless at trace levels. They just need you to believe it’s dangerous so you keep paying $500 a month. Wake up.
There’s a deeper question here: why do we treat medicine like a machine when it’s part of a living, breathing system? Patients aren’t test tubes. Their gut flora, their stress levels, their sleep-all affect absorption. Maybe instead of tightening limits, we should be giving doctors better tools to monitor patients individually. Precision medicine isn’t about the pill-it’s about the person.
Just want to add that in my clinic we started using a digital tracker for patients on NTI drugs-logs their symptoms, meds, sleep, diet. We found that 70% of ‘generic-related’ fluctuations were actually due to diet changes or missed doses. The drug wasn’t the problem. The system was. We now only switch generics with patient consent and a 2-week monitoring window. Simple. Effective. No drama.